Achilles Tendinopathy is characterized by pain, swelling, and limited function of the tendon, and may include calcification or ossification. Regardless of the specific pattern, several terms are used to describe calcification/ossification within or surrounding the Achilles Tendon, including Heterotopic Ossification of the Achilles Tendon, Calcifying Tendonitis, Ossified Tendonitis, Calcific Periarthritis, and Apatite Deposition. In contrast to Calcific Tendinitis, Ossific Tendinitis microscopic examination reveals one or more segments of mature lamellar bone formation within the substance of the tendon, either at the insertion or within the body of the tendon.
1. Overview
Extensive Ossification of the Achilles Tendon (EOAT) is an uncommon condition characterized by the presence of heterotopic ossification within the substance of the Achilles Tendon and is distinct from other tendinopathies associated with tendon mineralization. The purpose of this scoping review of the literature on EOAT is to describe the pathogenesis, patient population, presentation, management, and outcomes of this rare condition. Fifty-four articles were included in the scoping review after screening and selection. According to the literature, EOAT often presents with pain and swelling around the Achilles Tendon and is frequently associated with acute trauma. EOAT is more common in men, and although the exact mechanisms of the pathology are not fully understood, EOAT may demonstrate specific molecular signaling patterns. The lack of knowledge regarding the molecular mechanism may be a significant hindrance to the management of the condition. Even though a standard treatment regimen for EOAT does not exist, conservative management for six months in patients without complications is recommended. Those who have an acute fracture of the ossification should be managed more aggressively and will often require surgical repair with autograft, although there is no standardized procedure at this time. Clinicians should be aware of the typical presentation, risk factors, and management options of patients with EOAT. Additionally, they should be cautious when selecting treatment strategies and conduct a thorough evaluation of long-term outcomes with various treatment modalities, which this review provides. Most important, this review highlights the need for further research to determine the best course of clinical treatment of EOAT injuries, in order to establish a standard treatment regimen.
2. Achilles Tendinopathy
Achilles Tendinopathy and related conditions often result from a failed healing response to chronic tendon injury
[1]. Achilles Tendinopathy is characterized by pain, swelling, and limited function of the tendon, and may include calcification or ossification
[2]. Regardless of the specific pattern, several terms are used to describe calcification/ossification within or surrounding the Achilles Tendon, including Heterotopic Ossification of the Achilles Tendon, Calcifying Tendonitis, Ossified Tendonitis, Calcific Periarthritis, and Apatite Deposition
[2][3]. In contrast to Calcific Tendinitis, Ossific Tendinitis microscopic examination reveals one or more segments of mature lamellar bone formation within the substance of the tendon, either at the insertion or within the body of the tendon
[4][5][6]. Rarely, the Achilles Tendon completely or partially ossifies over time. We refer to this condition as Extensive Ossification of the Achilles Tendon. In this review, “extensive” is defined as ossification within or surrounding the Achilles Tendon that comprises at least roughly one-third of the affected tendon.
Extensive Ossification of the Achilles Tendon differs from other types of Achilles tendinopathies in several ways. First, many individuals with EOAT report a history of acute trauma or surgery to the Achilles, often decades before
[2]. This is in contrast to other types of tendinopathy which tend to occur after chronic degeneration. Second, EOAT may go unnoticed for decades until the heterotopic bone fractures
[3][5]. Third, because EOAT is rare, little research has been conducted to identify the pathophysiology, risk factors, treatments used, and outcomes of these treatment approaches.
Despite the lack of a defined pathophysiology, an important distinguishing factor of EOAT is that it may cause the ossified Achilles to fracture after decades of being silent, which often presents with acute tenderness, pain, localized edema, and decreased range of motion. Diagnosis is confirmed with plain radiographs and is characterized by the presence of one or more segments of ossified masses of variable sizes within the body of the Achilles Tendon
[7].
When Achilles Tendon radiopacities are identified on plain radiographs, they are characterized as falling into one of four types. Type I refers to radiopacities at the tendon insertion. Type II refers to radiopacities found 1–3 cm proximal to tendon insertion, and Type III refers to larger, more proximal radiopacities. Type III ossifications are further divided into Type IIIa and Type IIIb. Type IIIa is characterized by partial ossification. Type IIIb indicates complete ossification of the tendon
[8][9][10]. The diagnosis can be further delineated with ultrasound or magnetic resonance imaging
[11].
Various treatments for Achilles Tendinopathy, Calcific Tendinopathy, and Insertional Calcific Tendinopathy have been studied extensively
[1]. Conservative management strategies that have been utilized include eccentric exercise techniques, orthotics, medications such as non-steroidal anti-inflammatory drugs (NSAIDs) and nitric oxide patches, shock wave therapy, ultrasound therapy, and various types of locally injected medication. Multiple surgical treatment approaches are also commonly utilized
[1]. These include removal of the ossified Achilles and replacing it with an autograft from tendons of the semitendinosus, gracilis, fascia lata, gastrocnemius-soleus muscle, and flexor hallicus longus
[5][12][13][14][15].
3. Discussion
Ossification of the Achilles Tendon is an uncommon condition with an unknown prevalence. There are a limited number of studies, most of which are case reports of patients who present with an acute fracture of the ossified mass. Other reports describe patients without a fracture who have a large ossification and presented with pain and swelling. Since many ossified Achilles Tendons are silent for decades and may or may not result in an acute fracture of the ossification, many patients likely are asymptomatic and have undetected ossification.
3.1. Presentation
Extensive Ossification of the Achilles Tendon usually presents decades after an acute traumatic event to the lower leg. A common traumatic event is lower leg surgery during childhood. However, in some cases, there is no attributable prior traumatic event. Patients who present with a fracture to the ossified Achilles Tendon most commonly describe acute pain and swelling of the lower leg and occasionally an audible “pop.” The condition is approximately twice as common in men
[16]. There is no current explanation for the male preponderance, but hormones and varying activity levels should be considered
[16]. The mean age of presentation, calculated from our collection of 30 case reports and clinical images, is 55 years old with a range of 24 to 84 years old
[17][18]. On physical examination, the ossified Achilles Tendon may have an indurated feel, with some reports suggesting the presence of a palpable gap at the site of the fracture. The mass is typically not tender or painful until the ossification fractures or the Achilles Tendon ruptures. Depending on whether the Achilles Tendon is intact or not, the patient may have a positive Thompson test
[4]. Extensive Ossification of the Achilles Tendon may also present without an associated fracture. In cases of Extensive Ossification without an acute fracture, patients often present with insidious pain and swelling to the affected heel, restricted range of motion, and limitations in activities of daily living
[19][20].
3.2. Diagnostic Criteria
When providers suspect the presence of EOAT, the first imaging modality that should be performed is plain radiographs or in-office ultrasound if available. In-office ultrasound will likely reveal the hyperechoic mass and may detect a fracture if present
[21]. Plain radiographs should be obtained to view the extent of the ossification and whether there is a fracture present
[7][11][22]. Plain films are also used to categorize the ossification based on the location of ossification in the Achilles Tendon. The Morris classification, which classifies Achilles calcification/ossification based on the distance from the insertion of the tendon onto the calcaneus, is sometimes used. Additionally, obtaining plain film radiography soon after the initial office visit will provide a baseline upon which future imaging can be used to compare. Although Magnetic Resonance Imaging (MRI) is not required to make the diagnosis of EOAT
[18], it can be used as an adjunctive diagnostic method to assess the integrity of the tendon, providing more detail regarding the composition and location of the ossification and the extent of soft tissue destruction. Magnetic Resonance Imaging is also useful in identifying a hematoma
[2].
3.3. Histology
Calcification and ossification are two distinct forms of tendon mineralization. Calcium that deposits in normal, healthy tissue is called metastatic calcification. Calcium that deposits in damaged tissue is called dystrophic calcification. In calcific tendinitis, the tissue contains calcium phosphate and/or calcium carbonate, which is not organized into an orderly structure microscopically. Additionally, the calcification in calcific tendinitis may regress over time as part of healing
[23]. In contrast, the term ‘ossification’ suggests the formation of bone
[24]. True ossific tendonitis will demonstrate crystals of hydroxyapatite, which are organized into lamellar bone
[4][5]. Heterotopic bone formation usually occurs via endochondral ossification
[16]. Both calcific tendonitis and ossific tendonitis are more common in men. Achilles Tendon ossification is much rarer than Achilles calcific tendonitis
[5].
3.4. Pathobiology and Risk Factors
Heterotopic ossification, defined as bone developing de novo in soft tissue, may be a consequence of degenerative changes in collagen caused by vascular insufficiency. Vascular insufficiency leads to chronic tissue hypoxia, leading to an inflammatory cascade that causes mesenchymal stem cells in the tendon to differentiate towards bone development
[2][25][19][26]. Up to 62% of patients who undergo percutaneous or open repair of the Achilles Tendon develop mineralization, but the proportion of cases which progress to Extensive Ossification is unknown
[27].
The etiology of Achilles Tendon ossification is likely to be multifactorial and may be a result of overt trauma, repetitive micro trauma, surgery, or burns to the Achilles Tendon
[28][29][26]. Some systemic diseases have been seen in conjunction with ossification, including diffuse idiopathic skeletal hyperostosis, fluorosis, ochronosis, Wilson’s disease, renal failure Reiter’s syndrome, ankylosing spondylitis and gout, although these conditions have not been proven as causative
[25][26]. In the reports of EOAT, there were no abnormalities in the bloodwork that would suggest presence of the associated disorders.
Despite no recognized abnormalities in routine bloodwork, there may be a genetic predisposition, as ossification of the Achilles has been reported in biological siblings without history of trauma or surgery to the tendon. The age of presentation of the siblings were 50, 54, and 64 years old
[20]. This indicates that, if there is a hereditary component, the age of onset is consistent with most cases that are reported, which have an average age of presentation of 55 years old. Furthermore, two rare inherited conditions that cause heterotopic bone formation include fibro-dysplasia ossificans progressiva and progressive osseous hetero-plasia. Fibro-dysplasia ossificans is caused by a mutation of Activin receptor type-1 (ACVR1), which is a bone morphogenetic protein (BMP) type I receptor. The mutation causes overstimulated BMP signaling, leading to inappropriate ossification
[30]. Progressive osseous hetero-plasia (POH) is an inherited condition caused by an inactivating mutation in the GNAS locus, which leads to inappropriate ossification of the dermis and adipose tissue
[30].
Genetic predisposition to tendon calcification/ossification has also been studied in murine models, and there is evidence suggesting that TFG-B/BMP superfamily protein upregulation, BMP type1 receptor mutations, hypoxia inducible transcription factor (HIF), and bone-cartilage-stromal progenitor (BCSP) phenotype may contribute to endochondral ossification, which is the most frequent ossification pattern documented
[16][29][31]. The underlying pathophysiology of fibro-dysplasia ossificans progressiva and progressive osseous heterotopia, along with other molecular studies demonstrating the role of cell signaling pathways, suggest that heterotopic ossification is likely to be due to dysregulation of certain signaling pathways. The dysregulation may be induced by acute or chronic trauma, genetic makeup, or a combination of the two, ultimately resulting in a failed healing response of the Achilles Tendon. The genetic makeup of the patients who were included within this scoping review is not available. Further genetic studies would help to delineate the genome associations of EOAT.
3.5. Treatment
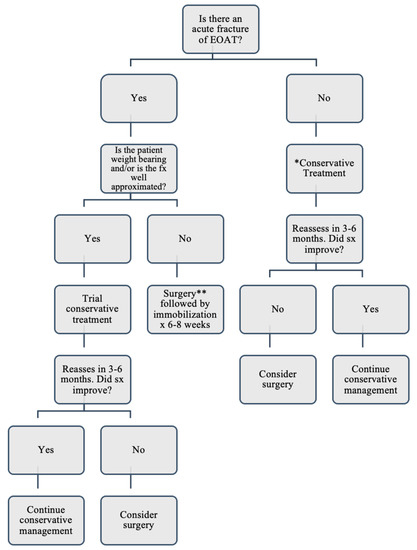
Figure 2 provides an algorithm with a reasonable approach to treating EOAT based on the treatment methods in the literature. To determine the most appropriate treatment in a patient with EOAT, medical providers should consider the pattern of onset, functionality of the patient, and the integrity of the Achilles Tendon. Currently, there is insufficient evidence to suggest that patients with Extensive Ossification have better outcomes with surgery than conservative treatment. However, the extent of the ossification has been reported to be one of several determining factors when deciding to treat surgically rather than conservatively. If the patient presents with EOAT that is painful but not fractured, the evidence in this scoping review recommends beginning with conservative treatment, including eccentric exercises, ice, heat, topical diclofenac or other topical agents, oral non-steroidal anti-inflammatory drugs (NSAIDs), and physical therapy
[9]. However, if the patient presents with EOAT and an acute fracture of the ossification, the provider should determine whether surgery or conservative management is the best initial option. The physician should consider the severity of the patient’s symptoms, weight bearing ability, and how much of the tendon is intact. If the fracture of the ossification is well approximated and if the patient has mild to moderate pain when weight bearing, has adequate range of motion, and can still perform limited function, beginning with conservative treatment would be an acceptable approach, bearing in mind conservative treatments have not consistently been effective for treating EOAT
[5][32]. Surgical excision and reconstruction followed by immobilization is shown to be the treatment of choice for those who have not responded to conservative methods
[1][5][32][17][19][20][33]. If conservative treatment does not reduce symptoms within approximately 3–6 months, the provider and patient should consider surgical reconstruction. Finally, if the patient has severe pain and/or cannot bear weight, or if there is complete rupture of the Achilles Tendon, surgical reconstruction as the initial treatment would be appropriate. Although several surgical treatments have been reported, the primary goal of surgical treatment is to preserve the continuity and function of the Achilles Tendon
[4][13]. Some instances may require complete removal of the ossification and tendon and replacement with an autograft. Several types of autografts have been reported, including grafts from the semitendinosus, gracilis, fascia lata, tendon of the gastrocnemius-soleus muscle, and flexor hallicus longus tendons
[5][12][13][15]. Use of each one of these types of autografts have resulted in successful short-term outcomes in the case reports, often restoring full functionality; however, only one of the reports included outcomes after one year. Therefore, it is reasonable for the surgeon to choose a surgical approach based on personal preference and the extent of the tissue damage until further evidence of this condition suggests an optimal standard approach
[13]. Following surgery, the ankle should be immobilized in equinus for six to eight weeks
[5][12][13][32][17][34][20], at which point the patient can begin bearing weight.
Figure 2. Management of Patients Presenting with an Extensive Ossification of the Achilles Tendon. * Conservative treatment: eccentric exercises, ice, heat, topical diclofenac or other topical agents, oral non-steroidal anti-inflammatory drugs (NSAIDs), and physical therapy. ** Surgery: various methods have achieved the same results of restoring continuity and function of the AT.