Clear cell renal cell carcinoma (ccRCC) is a type of kidney cancer that arises from the cells lining the tubes of the kidney. The tumor immune microenvironment (TIME) of ccRCC is a complex interplay of various immune cells, cytokines, and signaling pathways. One of the critical features of the ccRCC TIME is the presence of infiltrating immune cells, including T cells, B cells, natural killer cells, dendritic cells, and myeloid-derived suppressor cells. The complex interplay between the immune system and the tumor in ccRCC has important implications for developing new treatment strategies. Immunotherapy, which aims to activate the immune system to recognize and eliminate tumor cells, has shown promise in the treatment of ccRCC, and several immune-based therapies have been approved for clinical use.
- ccRCC
- clear cell renal cell carcinoma
- mccRCC
- metastatic clear cell renal cell carcinoma
1. Immune Checkpoint Inhibitors
2. Targeted Therapies
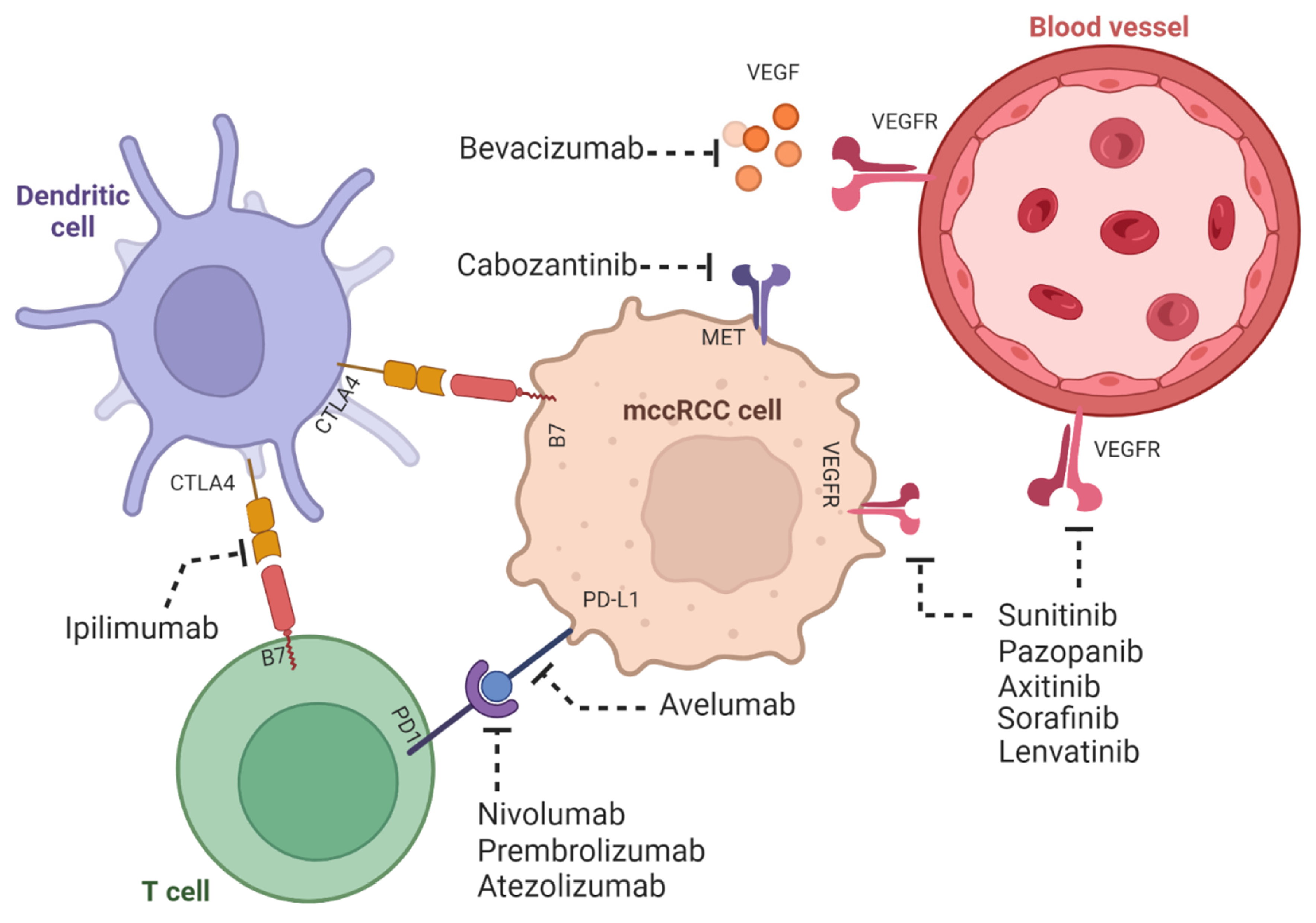
3. Combination Therapies
4. Adoptive Cell Therapy
This entry is adapted from the peer-reviewed paper 10.3390/ijms24097946
References
- Massari, F.; Di Nunno, V.; Cubelli, M.; Santoni, M.; Fiorentino, M.; Montironi, R.; Cheng, L.; Lopez-Beltran, A.; Battelli, N.; Ardizzoni, A. Immune checkpoint inhibitors for metastatic renal cell carcinoma: A systematic review and meta-analysis. Immunotherapy 2019, 11, 543–558.
- Motzer, R.J.; Escudier, B.; McDermott, D.F.; George, S.; Hammers, H.; Srinivas, S.; Tykodi, S.; Sosman, J.; Procopio, G.; Plimac, E.; et al. Nivolumab versus everolimus in advanced renal-cell carcinoma. N. Engl. J. Med. 2015, 373, 1803–1813.
- Motzer, R.J.; Tannir, N.M.; McDermott, D.F.; Frontera, O.A.; Melichar, B.; Choueiri, T.; Plimack, E.; Barthélémy, P.; Porta, C.; George, S.; et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N. Engl. J. Med. 2018, 378, 1277–1290.
- Brown, L.C.; Zhu, J.; Desai, K.; Kinsey, E.; Kao, C.; Lee, Y.H.; Pabla, S.; Labriola, M.K.; Tran, J.; Dragnev, K.H.; et al. Evaluation of tumor microenvironment and biomarkers of immune checkpoint inhibitor response in metastatic renal cell carcinoma. J. Immunother. Cancer 2022, 10, e005249.
- Villarroel-Espindola, F.; Yu, X.; Datar, I.; Mani, N.; Sanmamed, M.; Velcheti, V.; Syrigos, K.; Toki, M.; Zhao, H.; Chen, L.; et al. Spatially resolved and quantitative analysis of VISTA/PD-1H as a novel immunotherapy target in human non-small cell lung cancer. Clin. Cancer Res. 2018, 24, 1562–1573.
- Chen, X.; Shao, Q.; Hao, S.; Zhao, Z.; Wang, Y. TIM-3 expression and its role in hepatocellular carcinoma. J. Hematol. Oncol. 2018, 11, 126.
- Guo, Z.; Wang, X.; Cheng, D.; Xia, Z.; Luan, M. LAG3 expression in clear cell renal cell carcinoma: A predictor of unfavorable clinical outcome. Mol. Med. Rep. 2018, 17, 354–360.
- Chen, X.; Lu, P.H.; Liu, L.; Fang, Z.M.; Duan, W.; Liu, Z.L.; Wang, C.Y.; Zhou, P.; Yu, X.F.; He, W.T. TIGIT negatively regulates inflammation by altering macrophage phenotype. Immunobiology 2016, 221, 48–55.
- Lu, Y.; Aimetti, A.A.; Langer, R.; Gu, Z. Bioresponsive materials. Nat. Rev. Mater. 2016, 2, 16075.
- Cheng, Y.; Wang, C.; Wang, H.; Zhang, Z.; Yang, X.; Dong, Y.; Ma, L.; Luo, J. Combination of an autophagy inhibitor with immunoadjuvants and an anti-PD-L1 antibody in multifunctional nanoparticles for enhanced breast cancer immunotherapy. BMC Med. 2022, 28, 411.
- Suo, A.; Qian, J.; Zhang, Y.; Liu, R.; Xu, W.; Wang, H. Comb-like amphiphilic polypeptide-based copolymer nanomicelles for co-delivery of doxorubicin and P-gp siRNA into MCF-7 cells. Mater. Sci. Eng. C Mater. Biol. Appl. 2016, 62, 564–573.
- Bhattarai, S.R.; Muthuswamy, E.; Wani, A.; Brichacek, M.; Castañeda, A.L.; Brock, S.L. Nanotechnology-mediated therapies for combating cancer: Perspectives on nanomedicine from the region. Adv. Drug Deliv. Rev. 2019, 138, 190–204.
- Gao, J.; Hou, B.; Zhu, Q.; Jiang, X.; Zou, Z.; Li, X.; Xu, T.; Zheng, M.; Chen, Y.H.; Xu, Z.; et al. Engineering biorthogonal POLY-PROTAC nanoparticles for tumor-specific protein degradation and precise cancer therapy. Nat. Commun. 2022, 13, 4318–4332.
- Lee, J.Y.; Termsarasab, U.; Park, J.H.; Lee, S.Y.; Ko, S.H.; Shim, J.S.; Chung, S.J.; Cho, H.J.; Kim, D.D. Dual CD44 and folate receptor-targeted nanoparticles for cancer diagnosis and anticancer drug delivery. J. Control. Release 2016, 236, 38–46.
- Chhipa, R.R.; Singh, A.K. Targeting mitochondrial metabolism in renal cell carcinoma. Clin. Transl. Med. 2018, 7, 6.
- Zhang, H.; Gao, P.; Fukuda, R.; Kumar, G.; Krishnamachary, B.; Zeller, K.I.; Dang, C.V.; Semenza, G.L. HIF-1 Inhibits Mitochondrial Biogenesis and Cellular Respiration in VHL-Deficient Renal Cell Carcinoma by Repression of C-MYC Activity. Cancer Cell 2007, 11, 407–420.
- Xu, W.; Yang, H.; Liu, Y.; Yang, Y.; Wang, P.; Kim, S.H.; Ito, S.; Yang, C.; Wang, P.; Xiao, M.T.; et al. Oncometabolite 2-hydroxyglutarate is a Potent Inhibitor of α-Ketoglutarate-Dependent Dioxygenases. Cancer Cell. 2015, 19, 17–30.
- Finke, J.H.; Rini, B.; Ireland, J.; Rayman, P.; Richmond, A.; Golshayan, A.; Wood, L.; Elson, P.; Garcia, J.; Dreicer, R.; et al. Sunitinib reverses type-1 immune suppression and decreases T-regulatory cells in renal cell carcinoma patients. Clin. Cancer Res. 2008, 14, 6674–6682.
- Rini, B.I.; Plimack, E.R.; Stus, V.; Gafanov, R.; Hawkins, R.; Nosov, D.; Pouliot, F.; Alekseev, B.; Soulières, D.; Melicha, B.; et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N. Engl. J. Med. 2019, 380, 1116–1127.
- Atkins, M.B.; McDermott, D.F.; Powles, T.; Motzer, R.J.; Rini, B.I.; Fong, L.; Joseph, R.W.; Pal, S.K.; Sznol, M.; Hainsworth, J.D.; et al. IMmotion150: A phase II trial in untreated metastatic renal cell carcinoma (mRCC) patients to assess the safety and efficacy of atezolizumab (atezo) in combination with bevacizumab (bev) or sunitinib (sun) compared to sun monotherapy. J. Clin. Oncol. 2017, 35 (Suppl. S15), 4505.
- Tannir, N.M.; Frontera, O.A.; Hammers, H.J.; Carducci, M.A.; McDermott, D.F.; Salman, P.; Escudier, B.; Beuselinck, B.; Amin, A.; Porta, C.; et al. Thirty-month follow-up of the phase III CheckMate 214 trial of first-line nivolumab + ipilimumab (N+I) or sunitinib (S) in patients (pts) with advanced renal cell carcinoma (aRCC). J. Clin. Oncol. 2019, 37, 547.
- Awad, M.M.; Govindan, R.; Balogh, K.N.; Spigel, D.R.; Garon, E.B.; Bushway, M.E.; Poran, A.; Sheen, J.H.; Kohler, V.; Esaulova, E.; et al. Personalized neoantigen vaccine NEO-PV-01 with chemotherapy and anti-PD-1 as first-line treatment for non-squamous non-small cell lung cancer. Cancer Cell 2022, 40, 1010–1026.e11.
- Wang, Y.; Buck, A.; Grimaud, M.; Culhane, A.C.; Kodangattil, S.; Razimbaud, C.; Bonal, D.M.; Nguyen, Q.D.; Zhu, Z.; Wei, K.; et al. Anti-CAIX BBζ CAR4/8 T cells exhibit superior efficacy in a ccRCC mouse model. Mol. Ther. Oncolytics 2021, 24, 385–399.
- de Campos, N.S.P.; de Oliveira Beserra, A.; Pereira, P.H.B.; Chaves, A.S.; Fonseca, F.L.A.; da Silva Medina, T.; Dos Santos, T.G.; Wang, Y.; Marasco, W.A.; Suarez, E.R. Immune Checkpoint Blockade via PD-L1 Potentiates More CD28-Based than 4-1BB-Based Anti-Carbonic Anhydrase IX Chimeric Antigen Receptor T Cells. Int. J. Mol. Sci. 2022, 23, 5448.
