Wound healing (WH) is a complex multistep process in which a failure could lead to a chronic wound (CW). CW is a major health problem and includes leg venous ulcers, diabetic foot ulcers, and pressure ulcers. CW is difficult to treat and affects vulnerable and pluripathological patients. On the other hand, excessive scarring leads to keloids and hypertrophic scars causing disfiguration and sometimes itchiness and pain. Treatment of WH includes the cleaning and careful handling of injured tissue, early treatment and prevention of infection, and promotion of healing. Treatment of underlying conditions and the use of special dressings promote healing.
- chronic wound
- electromagnetic fields
- hypertrophic scar
- keloid
- laser
- physical therapies
- photobiomodulation
- photodynamic therapy
- radiofrequency
- ultrasound therapy
- wound healing
1. Introduction
2. General Approach to Wounds
2.1. Epidemiology
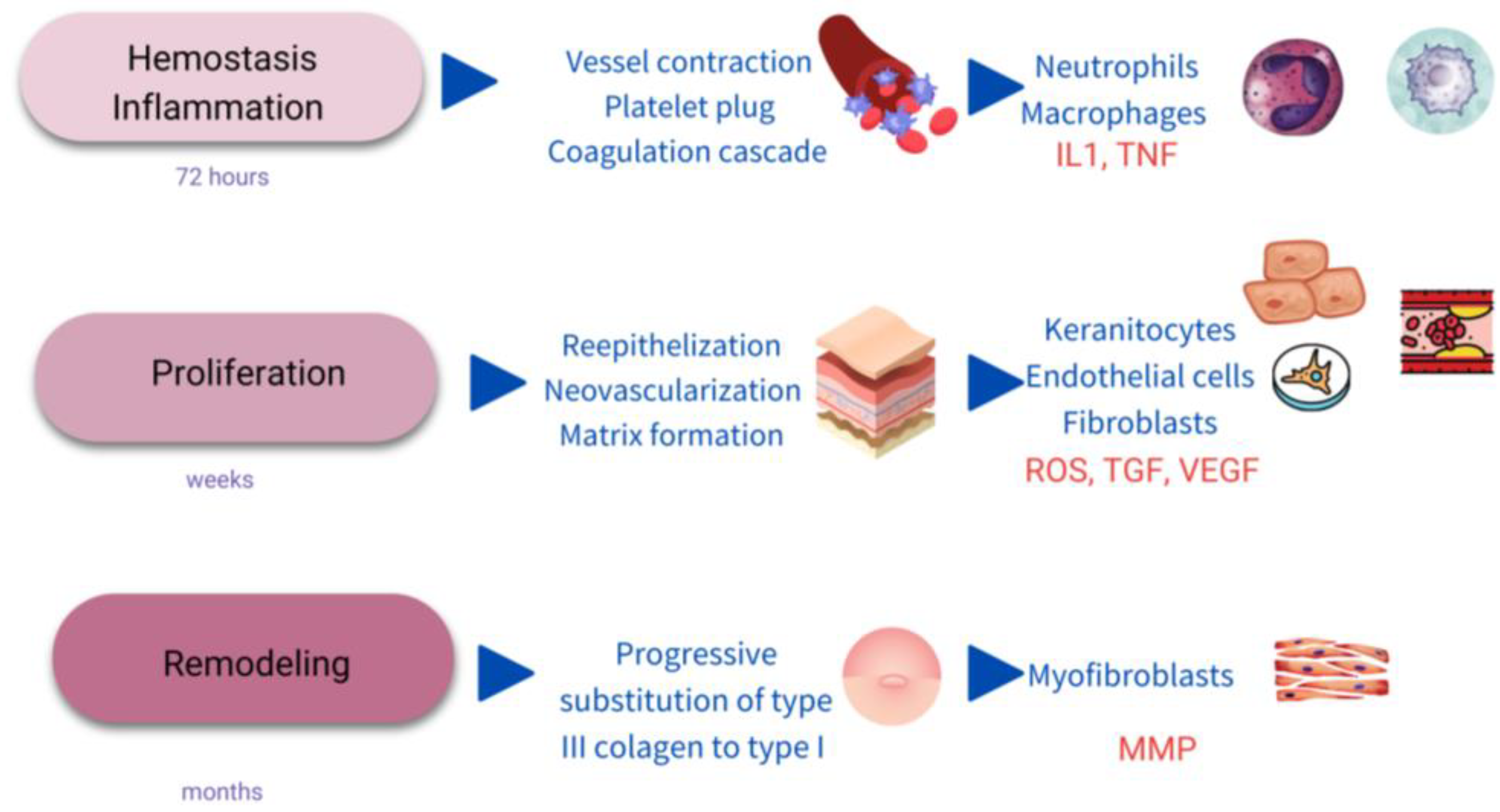
2.2. Process and Stages of Wound Healing
2.3. Chronic Wounds
2.4. General Management of Chronic Wounds
2.5. General Prevention of Scarring
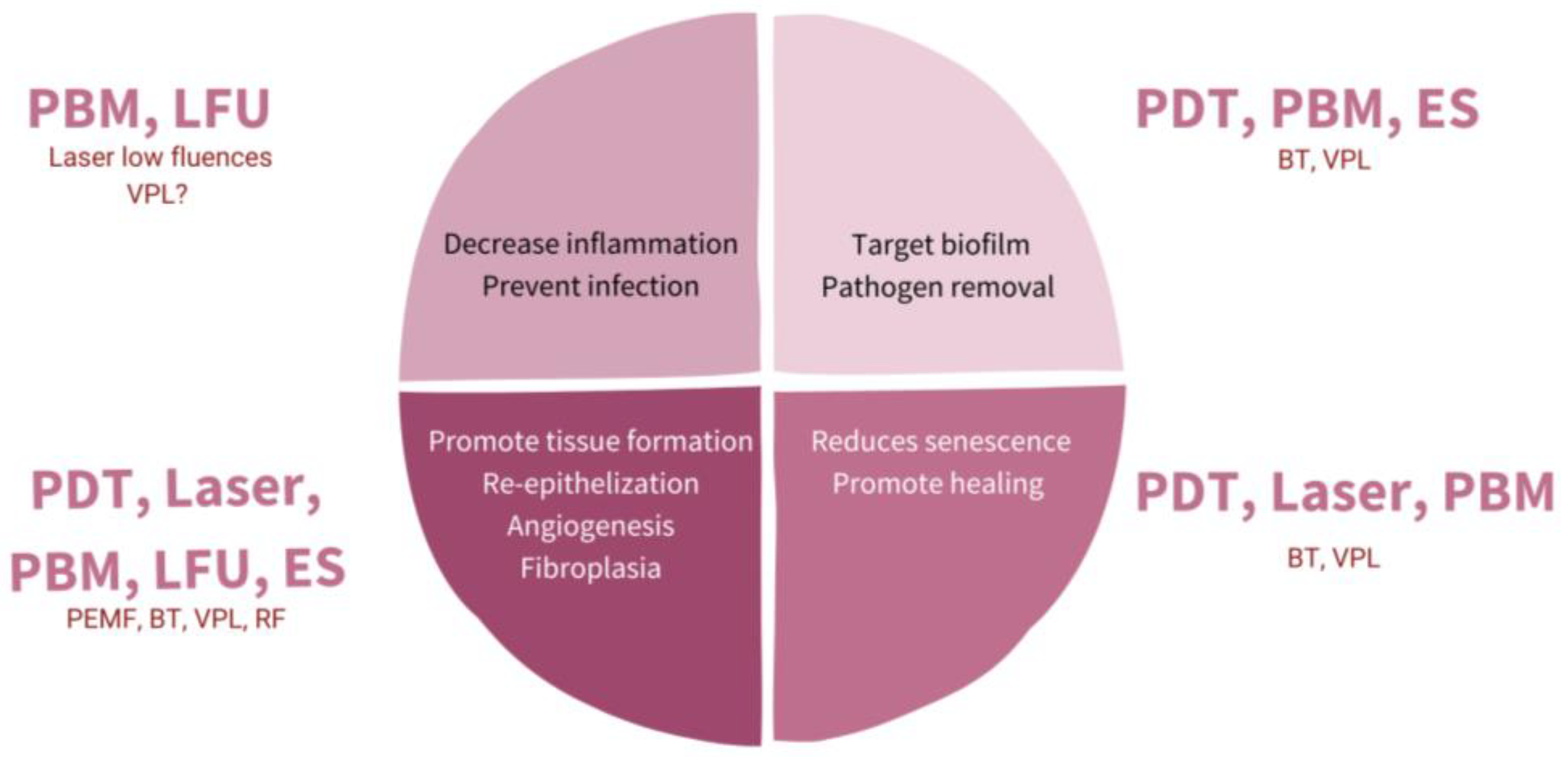
3. The Role of Physical Therapies in Hard-To-Heal Chronic Wounds
Principles and Basis
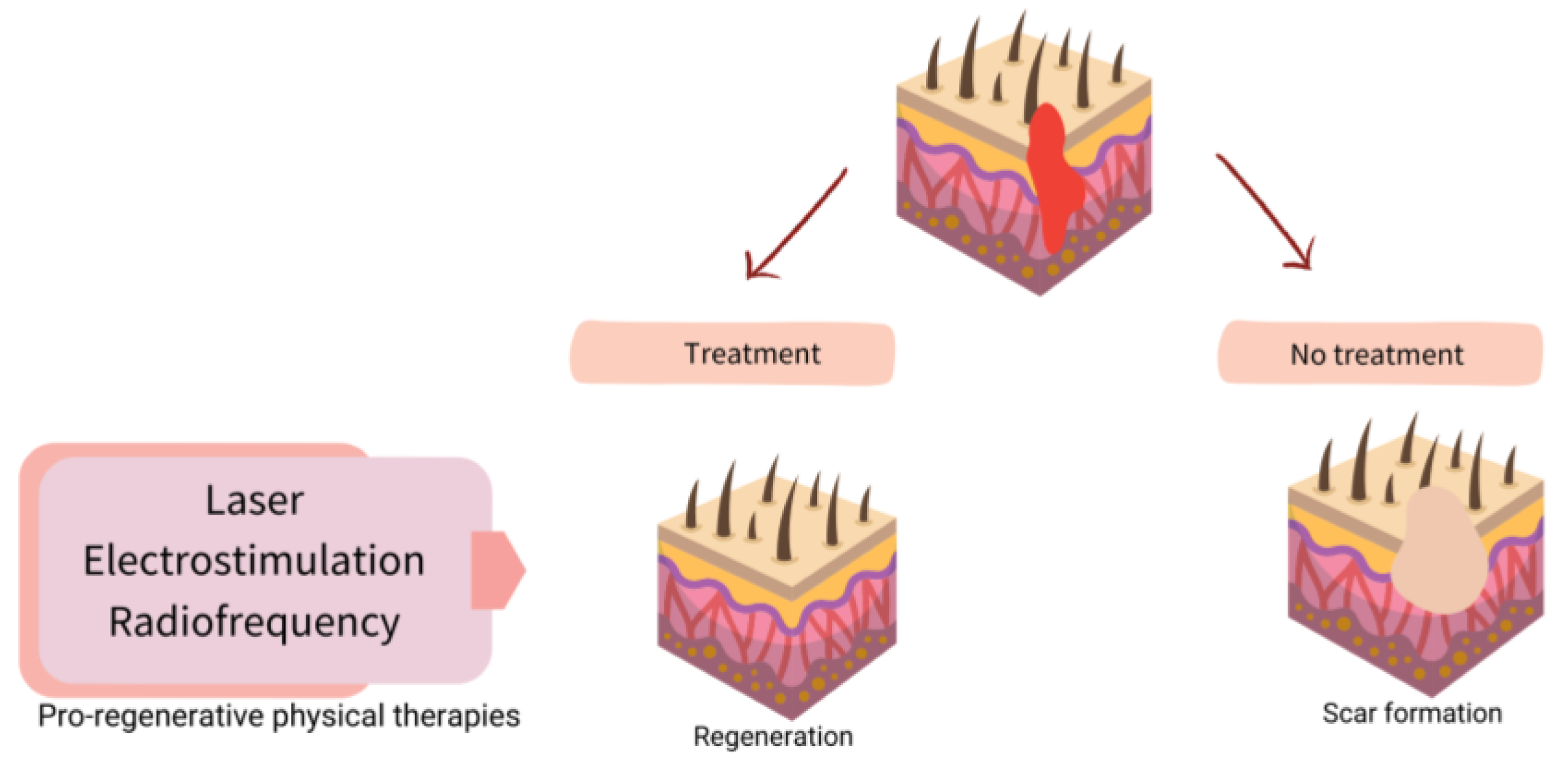
4. Physical Therapies in Assisted Healing and Scar Prevention
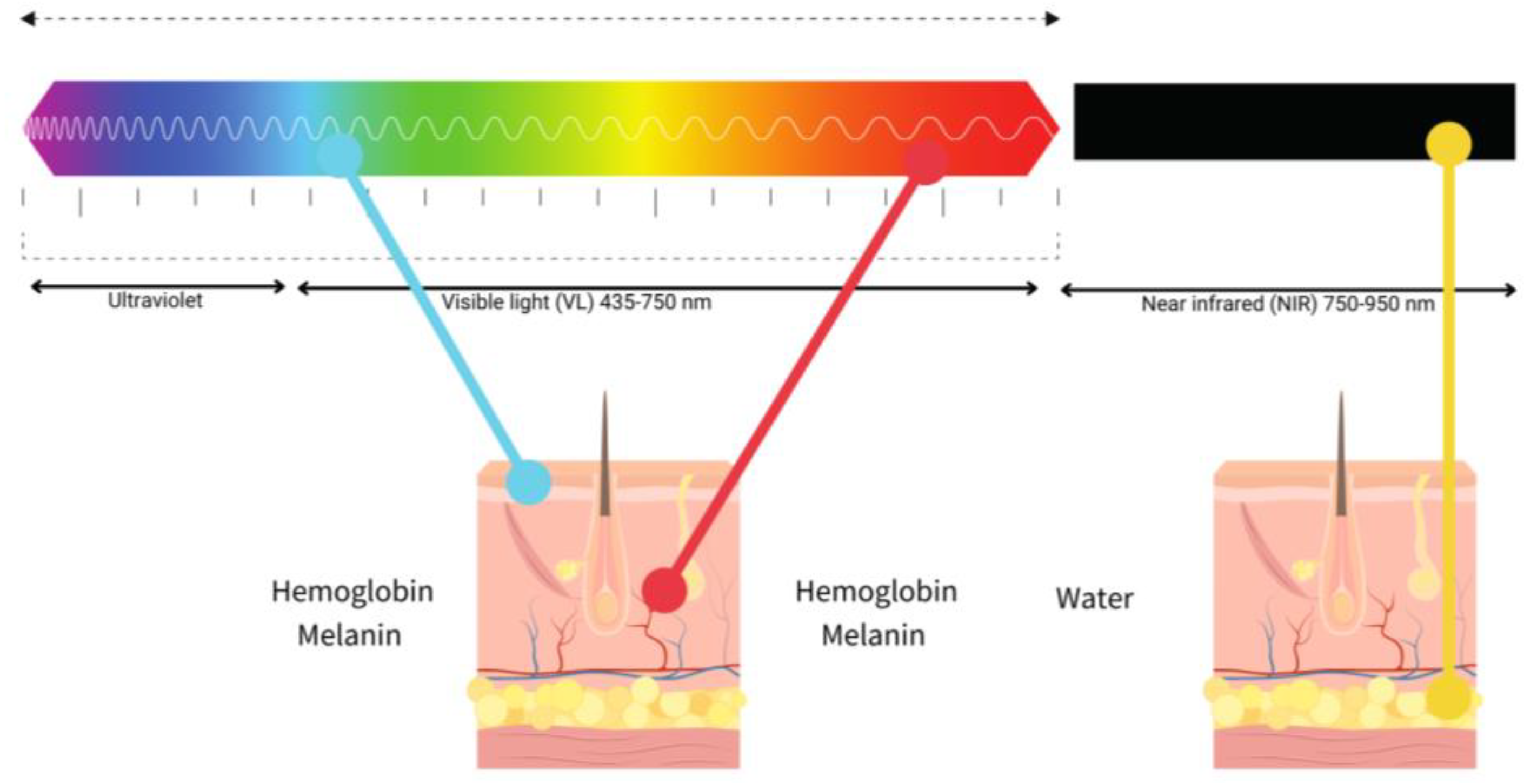
4.1. Laser
4.2. Photobiomodulation (Low-Level Light Therapy-LLLT)
4.3. Photodynamic Therapy
4.4. Electrical Stimulation
4.5. Others
4.5.1. Ultrasound Therapy
4.5.2. Electromagnetic Fields
4.5.3. Biophotonic Therapy
4.5.4. Visible Polarized Light
4.5.5. Radiofrequency
This entry is adapted from the peer-reviewed paper 10.3390/ijms24087487
References
- Gupta, S.; Andersen, C.; Black, J.; Fife, C.; Lantis, J.I.; Niezgoda, J.; Snyder, R.; Sumpio, B.; Tettelbach, W.; Treadwell, T.; et al. Management of Chronic Wounds: Diagnosis, Preparation, Treatment, and Follow-Up. Wounds Compend. Clin. Res. Pract. 2017, 29, S19–S36.
- Wang, P.H.; Huang, B.S.; Horng, H.C.; Yeh, C.C.; Chen, Y.J. Wound healing. J. Chin. Med. Assoc. 2018, 81, 94–101.
- Rodrigues, M.; Kosaric, N.; Bonham, C.A.; Gurtner, G.C. Wound Healing: A Cellular Perspective. Physiol. Rev. 2019, 99, 665–706.
- Veith, A.P.; Henderson, K.; Spencer, A.; Sligar, A.D.; Baker, A.B. Therapeutic strategies for enhancing angiogenesis in wound healing. Adv. Drug Deliv. Rev. 2019, 146, 97–125.
- Monavarian, M.; Kader, S.; Moeinzadeh, S.; Jabbari, E. Regenerative Scar-Free Skin Wound Healing. Tissue Eng. Part B Rev. 2019, 25, 294–311.
- Bai, Q.; Han, K.; Dong, K.; Zheng, C.; Zhang, Y.; Long, Q.; Lu, T. Potential Applications of Nanomaterials and Technology for Diabetic Wound Healing. Int. J. Nanomed. 2020, 15, 9717–9743.
- Palmieri, B.; Vadalà, M.; Laurino, C. Electromedical devices in wound healing management: A narrative review. J. Wound Care 2020, 29, 408–418.
- Lu, W.-S.; Zheng, X.-D.; Yao, X.-H.; Zhang, L.-F. Clinical and epidemiological analysis of keloids in Chinese patients. Arch. Dermatol. Res. 2015, 307, 109–114.
- Berman, B.; Maderal, A.; Raphael, B. Keloids and Hypertrophic Scars: Pathophysiology, Classification, and Treatment. Dermatol. Surg. 2017, 43, S3–S18.
- He, Y.; Deng, Z.; Alghamdi, M.; Lu, L.; Fear, M.W.; He, L. From genetics to epigenetics: New insights into keloid scarring. Cell Prolif. 2017, 50, e12326.
- Huang, C.; Ogawa, R. Systemic factors that shape cutaneous pathological scarring. FASEB J. 2020, 34, 13171–13184.
- Huang, C.; Ogawa, R. Keloidal pathophysiology: Current notions. Scars Burn. Health 2021, 7.
- Bowers, S.; Franco, E. Chronic Wounds: Evaluation and Management. Am. Fam. Physician 2020, 101, 159–166.
- Gottrup, F. A specialized wound-healing center concept: Importance of a multidisciplinary department structure and surgical treatment facilities in the treatment of chronic wounds. Am. J. Surg. 2004, 187, S38–S43.
- Fife, C.E.; Carter, M.J. Wound Care Outcomes and Associated Cost among Patients Treated in US Outpatient Wound Centers: Data from the US Wound Registry. Wounds A Compend. Clin. Res. Pract. 2012, 24, 10–17.
- Gurtner, G.C.; Werner, S.; Barrandon, Y.; Longaker, M.T. Wound repair and regeneration. Nature 2008, 453, 314–321.
- Wilcox, J.R.; Carter, M.J.; Covington, S. Frequency of debridements and time to heal: A retrospective cohort study of 312 744 wounds. JAMA Dermatol. 2013, 149, 1050–1058.
- Azevedo, M.-M.; Lisboa, C.; Cobrado, L.; Pina-Vaz, C.; Rodrigues, A.G. Hard-to-heal wounds, biofilm and wound healing: An intricate interrelationship. Br. J. Nurs. 2020, 29, S6–S13.
- Sun, F.; Qu, F.; Ling, Y.; Mao, P.; Xia, P.; Chen, H.; Zhou, D. Biofilm-associated infections: Antibiotic resistance and novel therapeutic strategies. Futur. Microbiol. 2013, 8, 877–886.
- Pastar, I.; Stojadinovic, O.; Yin, N.C.; Ramirez, H.; Nusbaum, A.G.; Sawaya, A.; Patel, S.B.; Khalid, L.; Isseroff, R.R.; Tomic-Canic, M. Epithelialization in Wound Healing: A Comprehensive Review. Adv. Wound Care 2014, 3, 445–464.
- Huang, C.; Akaishi, S.; Hyakusoku, H.; Ogawa, R. Are keloid and hypertrophic scar different forms of the same disorder? A fibroproliferative skin disorder hypothesis based on keloid findings. Int. Wound J. 2014, 11, 517–522.
- Kauvar, A.N.B.; Kubicki, S.L.; Suggs, A.K.; Friedman, P.M. Laser Therapy of Traumatic and Surgical Scars and an Algorithm for Their Treatment. Lasers Surg. Med. 2020, 52, 125–136.
- Altemir, A.; Boixeda, P. Laser Treatment of Burn Scars. Actas Dermosifiliogr. 2022, 113, T938–T944.
- Clementoni, M.T.; Pedrelli, V.; Zaccaria, G.; Pontini, P.; Motta, L.R.; Azzopardi, E.A. New Developments for Fractional CO2 Resurfacing for Skin Rejuvenation and Scar Reduction. Facial Plast. Surg. Clin. N. Am. 2020, 28, 17–28.
- Azzam, O.A.; Bassiouny, D.A.; El-Hawary, M.S.; El Maadawi, Z.M.; Sobhi, R.M.; El-Mesidy, M.S. Treatment of hypertrophic scars and keloids by fractional carbon dioxide laser: A clinical, histological, and immunohistochemical study. Lasers Med. Sci. 2016, 31, 9–18.
- Yang, Q.; Ma, Y.; Zhu, R.; Huang, G.; Guan, M.; Avram, M.M.; Lu, Z. The effect of flashlamp pulsed dye laser on the expression of connective tissue growth factor in keloids. Lasers Surg. Med. 2012, 44, 377–383.
- Zhibo, X.; Miaobo, Z. Molecular mechanism of pulsed-dye laser in treatment of keloids: An in vitro study. Adv. Skin Wound Care 2010, 23, 29–33.
- Lv, K.; Xia, Z.; Chinese Consensus Panel on the Prevention and Treatment of Scars. Chinese expert consensus on clinical prevention and treatment of scar+. Burn. Trauma 2018, 6, 27.
- Sobanko, J.F.; Vachiramon, V.; Rattanaumpawan, P.; Miller, C.J. Early postoperative single treatment ablative fractional lasing of Mohs micrographic surgery facial scars: A split-scar, evaluator-blinded study. Lasers Surg. Med. 2015, 47, 1–5.
- Shin, H.W.; Suk, S.; Chae, S.W.; Yoon, K.C.; Kim, J. Early postoperative treatment of mastectomy scars using a fractional carbon dioxide laser: A randomized, controlled, split-scar, blinded study. Arch. Plast. Surg. 2021, 48, 347–352.
- Lee, S.H.; Zheng, Z.; Roh, M.R. Early Postoperative Treatment of Surgical Scars Using a Fractional Carbon Dioxide Laser: A Split-Scar, Evaluator-Blinded Study. Dermatol. Surg. 2013, 39, 1190–1196.
- Kim, D.H.; Ryu, H.J.; Choi, J.E.; Ahn, H.H.; Kye, Y.C.; Seo, S.H. A Comparison of the Scar Prevention Effect between Carbon Dioxide Fractional Laser and Pulsed Dye Laser in Surgical Scars. Dermatol. Surg. 2014, 40, 973–978.
- Liu, X.-J.; Liu, W.-H.; Fang, S.-W.; Zhou, X.-L.; Xu, J.-X.; Li, G.-S. Lasers and Intense Pulsed Light for the Treatment of Pathological Scars: A Network Meta-Analysis. Aesthetic Surg. J. 2022, 42, NP675–NP687.
- Brewin, M.P.; Lister, T.S. Prevention or treatment of hypertrophic burn scarring: A review of when and how to treat with the Pulsed Dye Laser. Burns 2014, 40, 797–804.
- Leszczynski, R.; da Silva, C.A.; Pinto, A.; Kuczynski, U.; da Silva, E.M. Laser therapy for treating hypertrophic and keloid scars. Cochrane Database Syst. Rev. 2022, 9, CD011642.
- Seago, M.; Shumaker, P.R.; Spring, L.K.; Alam, M.; Al-Niaimi, F.; Anderson, R.R.; Artzi, O.; Bayat, A.; Cassuto, D.; Chan, H.H.; et al. Laser Treatment of Traumatic Scars and Contractures: 2020 International Consensus Recommendations. Lasers Surg. Med. 2020, 52, 96–116.
- Mosca, R.C.; Ong, A.A.; Albasha, O.; Bass, K.; Arany, P. Photobiomodulation Therapy for Wound Care: A Potent, Noninvasive, Photoceutical Approach. Adv. Ski. Wound Care 2019, 32, 157–167.
- Calabrese, E.J.; Dhawan, G.; Kapoor, R.; Agathokleous, E.; Calabrese, V. Hormesis: Wound healing and fibroblasts. Pharmacol. Res. 2022, 184, 106449.
- Tatmatsu-Rocha, J.C.; Ferraresi, C.; Hamblin, M.R.; Maia, F.D.; do Nascimento, N.R.; Driusso, P.; Parizotto, N. Low-level laser therapy (904 nm) can increase collagen and reduce oxidative and nitrosative stress in diabetic wounded mouse skin. J. Photochem. Photobiol. B Biol. 2016, 164, 96–102.
- Sperandio, F.F.; Simões, A.; Corrêa, L.; Aranha, A.C.C.; Giudice, F.S.; Hamblin, M.R.; Sousa, S.C. Low-level laser irradiation promotes the proliferation and maturation of keratinocytes during epithelial wound repair. J. Biophotonics 2014, 8, 795–803.
- Calabrese, E.J.; Dhawan, G.; Kapoor, R.; Agathokleous, E.; Calabrese, V. Hormesis: Wound healing and keratinocytes. Pharmacol. Res. 2022, 183, 106393.
- Heiskanen, V.; Hamblin, M.R. Photobiomodulation: Lasers vs. light emitting diodes? Photochem. Photobiol. Sci. 2018, 17, 1003–1017.
- Vitse, J.; Bekara, F.; Byun, S.; Herlin, C.; Teot, L. A Double-Blind, Placebo-Controlled Randomized Evaluation of the Effect of Low-Level Laser Therapy on Venous Leg Ulcers. Int. J. Low. Extremity Wounds 2017, 16, 29–35.
- Taradaj, J.; Halski, T.; Kucharzewski, M.; Urbanek, T.; Halska, U.; Kucio, C. Effect of Laser Irradiation at Different Wavelengths (940, 808, and 658 nm) on Pressure Ulcer Healing: Results from a Clinical Study. Evid. Based Complement. Altern. Med. 2013, 2013, 960240.
- Barolet, D.; Boucher, A. Prophylactic low-level light therapy for the treatment of hypertrophic scars and keloids: A case series. Lasers Surg. Med. 2010, 42, 597–601.
- Morton, C.A.; Szeimies, R.M.; Basset-Seguin, N.; Calzavara-Pinton, P.; Gilaberte, Y.; Haedersdal, M.; Hofbauer, G.F.L.; Hunger, R.E.; Karrer, S.; Piaserico, S.; et al. European Dermatology Forum guidelines on topical photodynamic therapy 2019 Part 1: Treatment delivery and established indications—Actinic keratoses, Bowen’s disease and basal cell carcinomas. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 2225–2238.
- Rajendran, S.B.; Challen, K.; Wright, K.L.; Hardy, J.G. Electrical Stimulation to Enhance Wound Healing. J. Funct. Biomater. 2021, 12, 40.
- Aleksandrowicz, H.; Owczarczyk-Saczonek, A.; Placek, W. Venous Leg Ulcers: Advanced Therapies and New Technologies. Biomedicines 2021, 9, 1569.
- Ud-Din, S.; Bayat, A. Electrical Stimulation and Cutaneous Wound Healing: A Review of Clinical Evidence. Healthcare 2014, 2, 445–467.
- Koel, G.; Houghton, P.E. Electrostimulation: Current Status, Strength of Evidence Guidelines, and Meta-Analysis. Adv. Wound Care 2014, 3, 118–126.
- Cullum, N.; Nelson, E.A.; Flemming, K.; Sheldon, T. Systematic reviews of wound care management: (5) beds; (6) compression; (7) laser therapy, therapeutic ultrasound, electrotherapy and electromagnetic therapy. Health Technol. Assess. 2001, 5, 9.
- Beheshti, A.; Shafigh, Y.; Parsa, H.; Zangivand, A.A. Comparison of High-Frequency and MIST Ultrasound Therapy for the Healing of Venous Leg Ulcers. Adv. Clin. Exp. Med. 2014, 23, 969–975.
- Cullum, N.; Liu, Z. Therapeutic ultrasound for venous leg ulcers. Cochrane Database Syst. Rev. 2017, 5, CD001180.
- Guerriero, F.; Botarelli, E.; Mele, G.; Polo, L.; Zoncu, D.; Renati, P.; Sgarlata, C.; Rollone, M.; Ricevuti, G.; Maurizi, N.; et al. Effectiveness of an Innovative Pulsed Electromagnetic Fields Stimulation in Healing of Untreatable Skin Ulcers in the Frail Elderly: Two Case Reports. Case Rep. Dermatol. Med. 2015, 2015, 576580.
- Kwan, R.L.; Wong, W.C.; Yip, S.L.; Chan, K.L.; Zheng, Y.P.; Cheing, G.L. Pulsed electromagnetic field therapy promotes healing and microcirculation of chronic diabetic foot ulcers: A pilot study. Adv. Skin Wound Care 2015, 28, 212–219.
- Romanelli, M.; Piaggesi, A.; Scapagnini, G.; Dini, V.; Janowska, A.; Iacopi, E.; Scarpa, C.; Fauverghe, S.; Bassetto, F.; EUREKA Study Group. Evaluation of fluorescence biomodulation in the real-life management of chronic wounds: The EUREKA trial. J. Wound Care 2018, 27, 744–753.
- Taha, M.M.; El-Nagar, M.M.; Elrefaey, B.H.; Elkholy, R.M.; Ali, O.I.; Alkhamees, N.; Felaya, E.-S.E.E.-S. Effect of Polarized Light Therapy (Bioptron) on Wound Healing and Microbiota in Diabetic Foot Ulcer: A Randomized Controlled Trial. Photobiomodulation Photomed. Laser Surg. 2022, 40, 792–799.
- M. Allam, N.; Eladl, H.M.; Eid, M.M. Polarized Light Therapy in the Treatment of Wounds: A Review. Int. J. Low Extrem. Wounds 2022, 15347346221113991.
- Feehan, J.; Burrows, S.P.; Cornelius, L.; Cook, A.M.; Mikkelsen, K.; Apostolopoulos, V.; Husaric, M.; Kiatos, D. Therapeutic applications of polarized light: Tissue healing and immunomodulatory effects. Maturitas 2018, 116, 11–17.
- Ekelem, C.; Thomas, L.; Van Hal, M.; Valdebran, M.; Lotfizadeh, A.; Mlynek, K.; Mesinkovska, N.A. Radiofrequency Therapy and Noncosmetic Cutaneous Conditions. Dermatol. Surg. 2019, 45, 908–930.
- Akbik, D.; Ghadiri, M.; Chrzanowski, W.; Rohanizadeh, R. Curcumin as a wound healing agent. Life Sci. 2014, 116, 1–7.
- Cucu, C.; Butacu, A.; Niculae, B.D.; Tiplica, G.S. Benefits of fractional radiofrequency treatment in patients with atrophic acne scars—Literature review. J. Cosmet. Dermatol. 2021, 20, 381–385.
