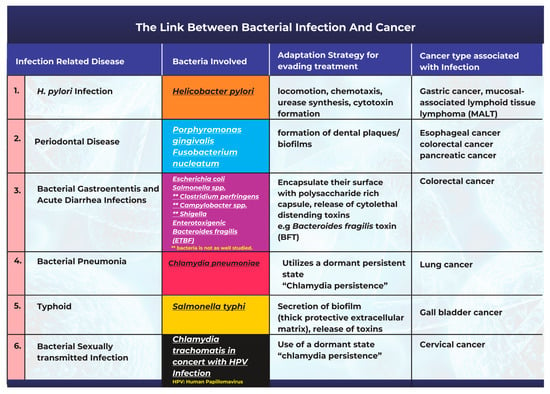
Several critical associations were found between bacterial infections and cancer, of which some are causative: Porphyromonas gingivalis and Fusobacterium nucleatum are associated with periodontal disease, Salmonella spp., Clostridium perfringens, Escherichia coli, Campylobacter spp., and Shigella are associated with gastroenteritis. Helicobacter pylori infection is implicated in the etiology of gastric cancer, and persistent Chlamydia infections present a risk factor for the development of cervical carcinoma, especially in patients with the human papillomavirus (HPV) coinfection. Salmonella typhi infections are linked with gallbladder cancer, Chlamydia pneumoniae infection is implicated in lung cancer, etc.
1. Introduction
Cancer is a disabling, challenging, and frightening disease that can affect any body part [
1]. The global cancer epidemic remains a public health concern, as cancer is established as the second foremost cause of death in the United States, with close to 2 million new cases and a little over 600,000 deaths expected to occur in 2022 [
2]. Mortality from lung cancer remains the most common type of cancer-related death, accounting for approximately 350 deaths daily [
2]. The public health burden associated with these high numbers has fueled massive research efforts to uncover the preventable causes of cancer [
3]. In a series of excellent reviews published recently, expert analysts reflect on the fact that the global burden of cancer is growing, especially in the most vulnerable sociodemographic populations, and that significant global effort is required not only to reduce the incidence of cancer but also to provide more equally distributed cancer control [
4,
5,
6].
Cancer results from a series of genetic and epigenetic changes that disrupt regular cell growth, control, and survival. A wide range of intrinsic and extrinsic factors influence these changes. Intrinsic factors may include genetic mutations, random errors in DNA replication, immune and inflammatory responses along with other modifiable factors, including aging; external factors may include diet type, smoking/tobacco use, radiation, and infectious organisms [
7].
Infectious pathogens such as bacteria and viruses are modifiable causes of cancer, accounting for 20% of all human tumors [
8,
9]. Pathogens associated with cancer can exhibit mechanisms that include persistent infection, evasion of the immune response, chronic inflammation leading to continued cell proliferation, and an increased risk of oncogenic transformation, even in immune-competent individuals [
10].
The human body is home to many microbes that form complex ecological habitats and influence the physiology of human health and disease, the totality of which may be summarized as the human microbiome [
11,
12]. The most effective way to describe the human microbiome is as a complex collection of microorganisms found in different body parts, including the skin, the oral cavity and saliva, the respiratory system, the reproductive tract, and the gastrointestinal system. These microorganisms include bacteria, eukaryotes, archaea, fungi, and viruses [
12,
13]. Since the population of bacteria in the microbiome vastly outnumbers that of other microorganisms, researchers sometimes simply refer to the microbiome as bacteria [
13]. According to Curtis and Sperandio, there are 100 trillion bacteria in the human body, with 500–1000 different bacterial species living mostly (but not exclusively) in the gut [
14]. The resulting interactions are beneficial to our homeostasis and well-being [
15].
Commensal bacteria colonize the host shortly after birth, forming at first a small community that progressively transforms into a diversified ecosystem. Over time, the host-bacterial associations develop into a mutually beneficial relationship [
14,
16]. The gut, for instance, provides nutrients to resident bacteria, which in turn assists food digestion, the absorption of nutrients, and the metabolism of indigestible substrates. This coexistence can also help to modulate immune system activity, maintain the intestinal architecture, and prevent the colonization of pathogenic microorganisms [
14,
16]. Despite this, an imbalance in host-bacterial interactions (dysbiosis) can change the physiological equilibrium in the host cells. This discrepancy can facilitate the progression of many conditions including inflammatory bowel disease, malnutrition, obesity, diabetes, and cancer [
15,
17].
3. The Link between Bacterial Infection and the Onset of Cancer
Bacteria and bacterial infections can act as potential carcinogens and tumor promoters [
18]. The production of bacterial toxins, enzymes, and oncogenic peptides can all significantly contribute to tumor development by promoting inflammation, interfering with cell cycle control, and disrupting cell signaling pathways [
18,
19]. Other studies have also corroborated the fact that microbiota-mediated infection stimulates cancer cell proliferation by targeting host cell DNA, altering the immune system, and promoting epithelial-to-mesenchymal transition [
17]. A description of the most frequently studied cases highlighting the link between bacterial infections and cancer is summarized in
Figure 1.
Figure 1. An illustration of the links between common bacterial infections and cancer.
3.1. Helicobacter pylori Infection and Gastric Cancer
One of the most well-known and researched connections associating cancer with a bacterial origin is the link between
Helicobacter pylori infection and gastric cancer [
8,
20,
21].
H. pylori has been extensively studied in this context with comprehensive epidemiological data supporting the existence of its causal relationship with carcinogenesis [
20,
22].
H. pylori is a gram-negative spiral-shaped bacterium that lives in a neutral pH niche between the stomach mucus layer and the gastric epithelium [
23,
24,
25]. Studies have opined that there are two potential explanations for the association between
H. pylori and gastric cancer. The first of these is that
H. pylori infection causes persistent gastric mucosal inflammation, resulting in atrophy and eventual intestinal metaplasia; the second is that
H. pylori can create, alter, or release bacterial virulence factors that play a significant role in cancer progression [
20,
23,
25]. Studies have also shown that
H. pylori infection contributes to an increase in the bacteria populations from the Proteobacteria, Spirochaetes, and Acidobacteria phyla, alongside a decline in the abundance of Bacteroidetes, Actinobacteria, and Firmicutes [
26].
H. pylori infection promotes persistent inflammation of the gastric mucosa and facilitates the progression of both mucosal-associated lymphoid tissue lymphoma and gastric cancer [
27,
28].
3.2. Periodontal Disease Caused by Bacterial Infections Can Promote Tumorigenesis
Fusobacterium nucleatum is an anaerobic, gram-negative, disease-causing bacterium in the oral cavity [
39]. Studies have suggested that dysbiosis of the oral microbiome allows
F. nucleatum to become an opportunistic bacterium that can cause gum disease and human cancers [
38,
39]. A research study revealed that the abundance of
F. nucleatum in the tissues of patients with esophageal squamous carcinoma was linked to shorter patient survival times [
39].
Porphyromonas gingivalis is a gram-negative bacterium that is an apparent pathogen in periodontal diseases and other systemic conditions [
40]. In 2011, a detailed study found that the concentration of
P. gingivalis was higher in cancer cells than in normal mouth tissues. T
Causes and incidence: Periodontal disease is a well-established and common oral condition in the human population [
47]. Periodontal diseases are associated with several risk factors: smoking habits, poor oral hygiene, medication regimens, age, heredity, and stress [
47]. These factors can hasten the dysbiosis of the oral microbiome and the multiplication of pathogenic bacteria, which drive disease progression.
Adaptation strategies for survival and the evasion of treatment: One major mechanism related to the persistence and adaptability observed in oral pathogenic bacteria is their ability to form dental plaques or biofilms (
Figure 1). These structures make them resistant to mechanical stress or antibiotic treatment [
47,
48]. The plaque biofilm acts as a protective barrier by isolating them from harmful agents and maintaining distinct phenotypic characteristics that promote their survival. Once the niche is established, the bacteria can release toxins such as lipopolysaccharide (LPS) and produce proinflammatory cytokines that promote chronic inflammation in periodontal tissues [
49].
3.3. Bacterial Pathogenesis in the Onset of Gastroenteritis, Acute Diarrhea, and Colon Cancer
Bacterial gastroenteritis is a kind of inflammation in the stomach and small intestine caused by a bacterial infection. In affected patients, the disease is often accompanied by severe diarrhea [
50]. Although gastroenteritis can be caused by viruses, fungi, or parasites, most cases are caused by bacterial pathogens [
50]. Bacteria associated with gastroenteritis include
Escherichia coli,
Salmonella spp.,
Clostridium perfringens,
Campylobacter spp., and
Shigella [
50].
Salmonella and
E. coli are the most frequently studied regarding their potential role in carcinogenesis.
Salmonella is an intracellular infection that affects a variety of animals and humans. The results of a
Salmonella infection can range significantly from a moderate, self-limiting gastroenteritis to a severe and potentially fatal systemic infection [
51].
Salmonella enterica serovar Enteritidis has been implicated in several gastroenteritis outbreaks linked to contaminated food [
52,
53].
E. coli is a gram-negative bacterium, ubiquitous in nature, that is found in the human gut microbiome [
57]. Several studies have found that patients with colorectal cancer have higher levels of colon mucosa-associated
E. coli colonization than those found in healthy individuals [
57,
58]. Pathogenic
E. coli strains have been shown to produce toxins (
Figure 1) such as cyclomodulin, cytotoxic necrosis factor (CNF), circulation inhibitory factor (Cif), colibactin, and cytolethal distending toxins (CDT). By disrupting the cell cycle and/or promoting DNA damage, these toxins can affect cell differentiation, apoptosis, and cell proliferation [
57,
59,
60].
Enterotoxigenic
Bacteroides fragilis (ETBF) is another common bacterium associated with acute diarrhea infections [
61].
Bacteroides fragilis (
B. fragilis) is an obligate anaerobic gram-negative bacillus bacterium [
62] that makes up 0.1% of the normal flora of the colon [
25]. However, ETBF levels are elevated in CRC patients’ feces and colonic mucosal tissues [
25]. According to the “alpha-bug” theory, a critical pathogenic species, such as (ETBF), remodels the microbiota to promote CRC, most probably through an IL-17 and Th17-mediated inflammatory response [
63].
3.4. Chlamydia pneumoniae Infection and Lung Cancer
Chlamydia pneumoniae (Cpn) is an obligate intracellular bacterium that causes various respiratory diseases in humans, including pneumonia [
70]. Chronic obstructive pulmonary disease, asthma, and lung cancer may result from repeated or prolonged exposure to
Chlamydia antigens [
71].
Previous research has found serological evidence of a link between
Chlamydia pneumoniae infection and lung cancer [
72]. A report also reviewed previous epidemiological studies on the link between
C. pneumoniae and lung cancer. It concluded that earlier investigations supported a causative relationship between
C. pneumoniae infection and lung cancer [
73]. Correspondingly, a group of researchers conducted a meta-analysis on 12 published articles that studied the link between
C. pneumoniae infection and lung cancer. The study concluded that
C. pneumoniae infection is correlated with an elevated risk of lung cancer, implying that a higher serological titer may be an efficient predictor of lung cancer risk [
74].
3.5. Salmonella typhi Infections and Gallbladder Cancer
Salmonella typhi is a gram-negative, rod-shaped, flagellated bacterium that is well documented as being responsible for typhoid infections [
78,
79,
80]. After infection,
S. typhi invades the gallbladder, causing persistent infection in susceptible carriers that serve as a reservoir for the spread of the disease; this persistent chronic infection has also been linked to cancer [
79,
81]. The ability of the pathogen to survive and persist for an extended time in the gallbladders of patients after infection creates a suitable environment for its tumor-promoting effect [
81]. It has also been reported that
S. typhi produces typhoid toxins and carcinogenic toxins such as nitroso-chemical compounds. These compounds play a crucial role in the progression of cancer [
80].
Causes and incidence: Infection by
S. typhi is usually acquired through the ingestion of food or water contaminated with the feces of a person carrying the organism [
78].
Salmonella typhi is suspected to be responsible for approximately 22 million cases of typhoid fever, slightly more than 5 million cases of paratyphoid fever, and approximately 200,000 deaths worldwide each year [
79].
Adaptation strategies for survival and the evasion of treatment: Through the secretion of biofilm,
S. typhi appears to survive and become well adapted to thrive in the gallbladder. Biofilm formation (
Figure 1) is a pathological adaptive response that allows the bacteria to aggregate, adhere to surfaces, and develop antimicrobial resistance through the utilization of a thick protective extracellular matrix [
79,
85].
3.6. Bacterial Infection and Cervical Cancer
Chlamydia trachomatis is a gram-negative bacterium and a prevalent cause of curable sexually-transmitted bacterial infections (STIs) worldwide [
86]. The infection presents as urethritis in men and endocervicitis in women [
87]. Persistent
Chlamydia infections have also been identified as a risk factor for developing cervical carcinoma [
87], especially in patients with the human papillomavirus (HPV) coinfection [
86,
88].
The association between
C. trachomatis and cervical cancer is usually seen in the presence of HPV infections [
86]. Since HPV infections have long been implicated in the etiology of cervical cancer [
90], it is difficult to directly classify the bacterial infection as solely causative, even though it contributes significantly to an increased incidence.
4. Mechanism of Cancer Development after Bacterial Infection
The onset of carcinogenesis after exposure to bacterial infection occurs over an extended period and depends on a wide range of factors such as host susceptibility, genetic background, and suitable environmental conditions [
91].
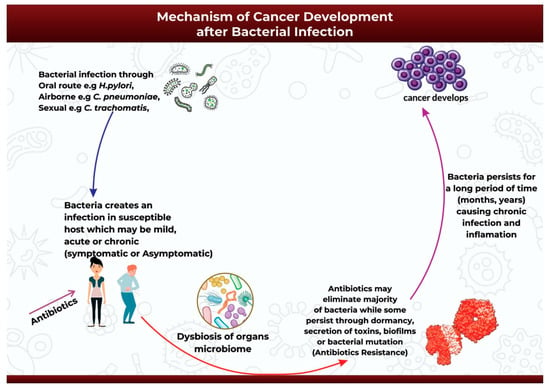
After the successful infection of the host either through oral, airborne, or sexually-transmitted routes (
Figure 2), the infection may start as mild, acute, or chronic and may be symptomatic or asymptomatic [
92]. Antibiotics might be introduced at this point to help ease the infection [
92]. The initial infection and subsequent antibiotic use may then initiate bacterial dysbiosis in the microbiome of the infected organ, in this case promoting the bloom of opportunistic and pathogenic bacteria species [
93,
94,
95]. Antibiotic use may completely eradicate the infection in some cases, or it may be ineffective against the application of alternative survival strategies by the bacteria to facilitate its continued existence over extended periods of time (
Figure 2). Pathogenic bacteria can survive and persist in the host environment through dormancy, secretion of cyotethal toxins, the formation of protective biofilms, or mutations to form antibiotic resistant strains [
17,
18]. This adaptive technique enables bacteria to promote persistent chronic inflammation or chronic infection, and ultimately carcinogenesis [
17] (
Figure 2).
Figure 2. An illustration of the mechanism of cancer development after bacterial infection.
5. Bacterial Infections during Cancer Treatment
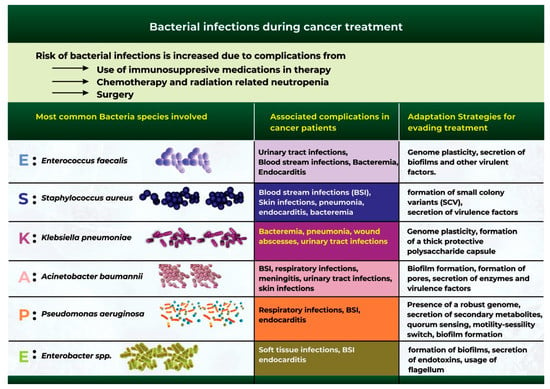
Bacterial infection is one of the most common complications during cancer treatment [
96]. Although cancer mortality rates have continued to decline in recent years, bacterial infections remain a significant cause of infection-related mortality in patients [
97]. Cancer patients are at a high risk of bacterial infection due to surgical complications, chemotherapy and radiotherapy-related neutropenia, and the use of immunosuppressive drugs during cancer treatment [
97,
98].
Extensive studies have identified a group of six bacterial microbes otherwise classified as the “ESKAPE” pathogens, which are at the forefront of bacterial infection and antibiotic resistance during cancer treatment (
Figure 3) [
104,
105]. These organisms include
Acinetobacter baumannii,
Staphylococcus aureus,
Enterococcus faecalis,
Klebsiella pneumoniae,
Pseudomonas aeruginosa, and
Enterobacter spp. [
104,
105].
Figure 3. The most common bacterial species that cause bacterial infections during cancer therapy.
6. Antibiotic Use and Antimicrobial Resistance in Cancer Patients
Antibiotics are secondary metabolites produced by microorganisms, higher animals, and plants, and they have antipathogenic effects that can interfere with the growth of other living cells [
125]. Antibiotics are increasingly being used to treat cancers, often because of their pro-apoptotic, antiproliferative, and antimetastatic potentials [
125]. Since infections are also common in cancer patients, it is essential to use antibiotics to prevent and treat bacterial infections [
98].
A major limitation of antibiotic use is the causation of dysbiosis due to the elimination of beneficial bacterial groups, such as Lactobacillus and Bifidobacterium, in addition to the pathogenic bacteria [
125]. A further limitation is the ability of pathogenic bacteria to evade killing and induce antibiotic resistance [
104].
It is also worth noting that the microbiome plays a crucial role in the development of antibiotic resistance [
126,
127]. Microbiota dysbiosis induced by antibiotic treatment contributes to the development of resistance that is often due to increased numbers of opportunistic bacteria secreting high levels of antimicrobial resistance genes [
128,
129].
Antibiotic resistance in cancer patients often correlates with increased susceptibility to infections that eventually reduce the patient’s survival time; it also poses a significant threat to the accomplishments achieved in cancer treatment, and it highlights the importance of monitoring cancer patients and protecting them against antibiotic resistance [
104].
This entry is adapted from the peer-reviewed paper 10.3390/ijms24043110