Psychotic episodes represent one of the most complex manifestations of various mental illnesses, and these encompass a wide variety of clinical manifestations that together lead to high morbidity in the general population. Various mental illnesses are associated with psychotic episodes; in addition, their incidence and prevalence rates have been widely described in the general population, their correct identification and treatment is a challenge for health professionals in relation to pregnancy. In pregnant women, psychotic episodes can be the consequence of the manifestation of a previous psychiatric illness or may begin during the pregnancy itself, placing not only the mother, but also the fetus at risk during the psychotic episode.
1. Introduction and Psychosis during Pregnancy
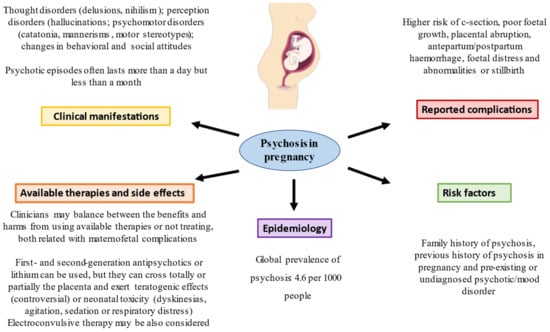
Psychosis refers to a disorder in which the person suffers a loss of perception with respect to reality, where he or she cannot distinguish what is real from what is unreal. Psychosis has a wide spectrum of manifestations of different psychiatric illnesses, including delusions and visual, tactile or auditory hallucinations. The current DSM-V classification includes a section where entities that cover the broad spectrum of schizophrenia are grouped together with other psychotic disorders (e.g., short psychotic disorder lasting less than 1 month, psychosis induced by toxic substances), but without clarifying all the possible diagnostic possibilities [
1]. One of the most relevant systematic reviews in regard to demonstrating the epidemiology of psychosis worldwide is based on the meta-analysis by Moreno-Kustner et al. [
2], who evaluated 73 different articles and established that the global prevalence of psychotic episodes or psychosis in the population overall is 4.6 per 1000 people. In Spain, the data available by the Ministry of Health indicate that affective psychosis or bipolar disorder (which includes mania, hypomania, manic depression and cyclothymia) has a prevalence of 7.2 cases per 1000 inhabitants, being more frequent in women than in men (9.6‰ in women, 4.8‰ in men). On the other hand, in the broad spectrum of schizophrenia, it affects approximately 4.5 men out of every 1000 and 2.9 women out of every 1000, including disorders such as schizophrenia and schizotypal, delusional and schizoaffective disorders. In turn, there are two groups of psychoses, namely, unspecified psychoses, which range from acute psychotic episodes to reactive or puerperal psychoses and affect 1.9 out of 1000 people; and organic psychoses or acute confusional syndrome, which are much more difficult to quantify and whose prevalence rises beginning at 65 years, generally affecting 30 per 1000 people. The latter may be underdiagnosed since the confusional syndrome is usually the consequence of an organic disease and, in many cases, it is not considered [
3].
The perinatal period encompasses both pregnancy and the subsequent 12 months. Throughout pregnancy, women may suffer from different psychiatric disorders, such as major depression, schizophrenia, bipolar disorder or maternal blues, postpartum depression and anxiety (which includes social phobia), as well as eating disorders, obsessive-compulsive disorder, posttraumatic stress disorder, panic attacks and puerperal psychosis [
4]. During this period, there are a great variety of psychiatric emergencies that have to be considered given the repercussions that they can have on the fetus and the mother. Even so, we must mention that the prevalence of psychosis is very low during pregnancy, although its implications in the fetus are important. For instance, it has been reported that women who suffered a psychotic episode in pregnancy had an increased risk of multiple adverse obstetric and neonatal outcomes, such as cesarean delivery, poor fetal growth, placental abruption, antepartum/postpartum hemorrhage, fetal distress and abnormalities or stillbirth [
5]. Among the main risk factors for suffering psychosis in pregnancy, having a family history of psychosis, previous history of psychosis in pregnancy and pre-existing or undiagnosed psychotic/mood disorder, such as schizophrenia or bipolar disorder, are considered [
6,
7]. The pathophysiological basis of psychosis in pregnancy is not completely understood. Changes in certain neurotransmitters, such as dopamine, acetylcholine, gamma aminobutyric acid (GABA) or glutamate, appear to be the main identified mechanisms in the brain [
8]. However, these alterations seems not be the cause per se, but a response to a genetic and environmental background, which ultimately leads to neurotransmitter dysregulation in specific regions of the brain [
9].
2. Treatment of Psychotic Episodes during Pregnancy
One of the most complex issues in the clinical management of a pregnant woman with a psychotic episode relies on the treatment of choice. There are multiple variables that must be considered, such as the prior diagnosis or new onset of a mental illness, medication previously used, trimester of pregnancy and risk of teratogenicity. We cannot forget that the information currently available to recommend a specific treatment in these cases is limited by the complexity of conducting randomized clinical trials due to the moral complexity of conducting pharmacological studies in pregnant patients. Despite this, one of the most relevant reviews to show the use of antipsychotics in pregnant women is the study by Toh et al. with 585,615 pregnant patients, of whom 4224 received treatment with second-generation antipsychotics and 548 received first-generation antipsychotics [
19]. There are several relevant studies that address the teratogenic risks and perinatal complications associated with the use of antipsychotics. For example, one of the first meta-analyses carried out by Altshuler et al. [
20] evaluated up to four studies that included 2591 pregnant women exposed to phenothiazines and showed that there was a slight increase in the risk of congenital anomalies in addition to postpartum complications such as respiratory depression or extrapyramidal symptoms when exposed to antipsychotic treatment in the first trimester; however, it should be noted that the included studies were difficult to evaluate. Along these lines, McKenna et al. [
21] evaluated 151 pregnant women exposed to different types of antipsychotic drugs, such as olanzapine, risperidone and quetiapine; they found that the rate of congenital malformations was not higher than that of the control group of pregnant women not exposed to antipsychotics. In agreement with the previous results, Huybrechts et al. evaluated more than 1.3 million pregnant women, with 9258 having received antipsychotic treatment and 733 of the 9258 women receiving it during the first trimester; in addition, they studied the teratogenic repercussion after the use of typical antipsychotics versus atypical or non-use. Their results showed that there was no significant increase in the development of congenital problems in women medicated with these types of drugs compared to nonmedicated women, as far as the first trimester of pregnancy is concerned [
22]. Regarding antipsychotic drugs, an increase in neonatal toxicity has been observed in the form of dyskinesias, agitation, sedation or respiratory distress due to the passage of different drugs through the placenta. The rate of placental passage from mother to fetus is important in drugs such as olanzapine (72%) or haloperidol (66%), in addition to other drugs such as risperidone (49%), which can limit the therapeutic arsenal in these patients [
23].
On the other hand, the standard treatment of patients with bipolar disorder is based on the use of lithium, which completely crosses the placenta, highlighting how the risk of teratogenicity can be up to double compared to that among healthy controls, mainly those with cardiac conditions, such as Ebstein’s malformation, alterations in the right ventricle, coarctation of the aorta and mitral atresia; in addition to the fact that at birth, the adverse effects of lithium generate apnea, bradycardia and seizures, among other adverse effects [
24,
25,
26]. It should be mentioned that in these patients, the treatment of choice is based on the use of first-generation antipsychotics such as haloperidol, with the use of second-generation antipsychotics such as risperidone, quetiapine or olanzapine according to different authors [
27,
28]. In patients with bipolar disorder who do not respond to previous therapies, lithium could be used according to different guidelines, despite the possible adverse and teratogenic effects described [
29]. Finally, we must mention that if all these measures are ineffective, there is the possibility of using electronconvulsive therapy, which is usually safe for both the mother and fetus and is effective, demonstrating partial remission rates in up to 70% of patients with bipolar disorder [
30]. Therefore, given the complexity of the treatment in these patients, the general recommendations are usually based on evaluating the suspension of treatment if the underlying disease presents minimal symptoms or using the minimum possible dose to avoid polypharmacy, as well as informing the patient and relatives of the disease, the current situation and how to carry out more rigorous control. Despite this, treating or not treating these episodes and/or mental illnesses should be studied individually, where the benefit/risk ratio can be assessed. This is because it is difficult to be certain of the impact that these drugs may have during pregnancy since in clinical trials with human drugs, for ethical and legal reasons, the safety and well-being of people prevails before the development of science and society. Overall, epidemiological data, risk factors, clinical manifestations, complications and therapeutic approaches in psychosis in pregnancy are summarized in
Figure 1.
Figure 1. A summary of the main data of psychosis in pregnancy.
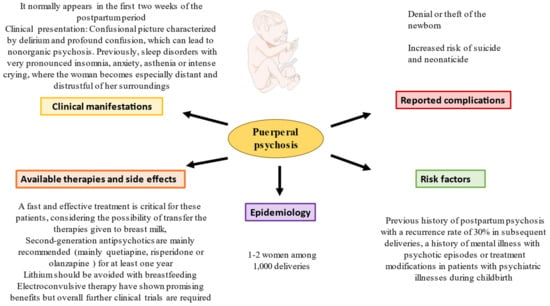
3. Puerperal Psychosis Treatment
As with the treatment of psychotic episodes during pregnancy, in the puerperium period, many aspects must be considered, such as the transfer of different antipsychotics to breast milk and that the rapidity of the presentation of the picture of puerperal psychosis entails applying a fast and effective treatment, given the prognostic implications associated with the psychosis in terms of self-aggression and the hetero-aggressiveness of the patient towards the newborn. Therefore, it should be considered an emergency in psychiatry and promptly addressed. It should also be noted that the treatment of puerperal psychosis, as well as psychosis during childbirth, lacks randomized clinical trials to evaluate the effective ones among different options, cases or small subgroups of patients [
40]. The first thing that must be considered is the safety of both the newborn and the mother; in addition, since the conditions are not present in most cases involving the safety of the newborn, the recommendation is to maintain vigilance in the interaction between the mother and newborn at hospital admission. Given the different possible manifestations of postpartum psychosis in cases in which agitation or psychosis predominates, the recommendation is to start therapy with second-generation antipsychotics, which are not passed at high quantities to breast milk and have lower rates of extrapyramidal effects and tardive dyskinesia than first-generation antipsychotics; quetiapine, risperidone or olanzapine is preferred, given the higher levels of clinical experience with these drugs since they are the ones that have been used the most in the different case reports [
41,
42,
43]. Subsequently, the recommendation is to maintain treatment with antipsychotics for at least one year and subsequently, evaluate these patients [
44]. In cases where patients have severe insomnia, the use of short-term benzodiazepines such as lorazepam in combination with second-generation antipsychotics is recommended [
45]. On the other hand, we must remember that a significant percentage of these patients have bipolar disorder, which is why mood stabilizers have an important relevance in these patients; in particular, lithium, which cannot be administered if the child is going to breastfeed, and valproic acid can be used in this case [
46,
47]. Finally, as in antepartum psychosis in refractory cases, electroconvulsive therapy can be used, as it has good results in different case reports. For example, Reed et al. evaluated the use of electroconvulsive therapy in 58 women with puerperal psychosis and showed improvement in up to 65% of cases [
48]. These results are in line with those observed by Rundgren et al., who observed a response rate of up to 87% in 185 women with postpartum psychosis [
49]. Finally, we must remember that socio-family support is important for follow up, in addition to the fact that the patient should be followed up after the postpartum period as well as if there are wishes for additional pregnancies given the possibility of recurrence of this entity [
50]. Collectively, epidemiological data, risk factors, clinical manifestations, complications and therapeutic approaches in puerperal psychosis are summarized in
Figure 2.
Figure 2. A summary of the main data of puerperal psychosis.
This entry is adapted from the peer-reviewed paper 10.3390/jcm12020656