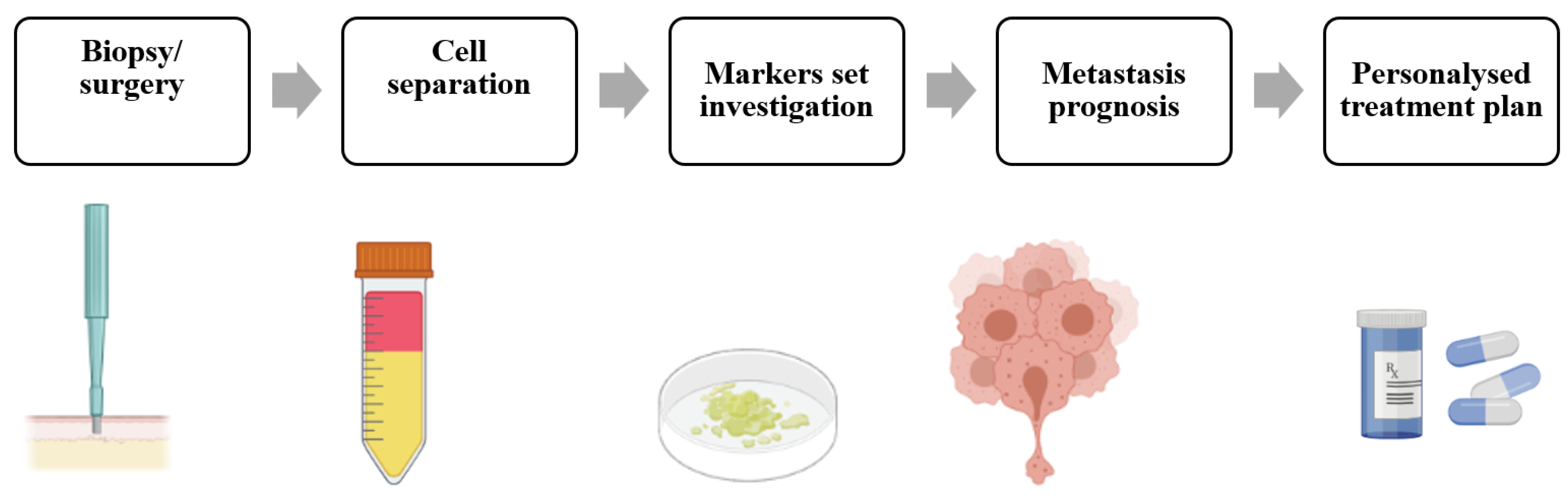
The major cause (more than 90%) of all cancer-related deaths is metastasis, thus its prediction can critically affect the survival rate. Metastases are predicted by lymph-node status, tumor size, histopathology and genetic testing. The identification of new potential prognostic factors will be an important source of risk information for the practicing oncologist, potentially leading to enhanced patient care through the proactive optimization of treatment strategies. Mechanobiology, as a branch of biomechanics and/or a branch of biology, has reached a mature stage mainly because of the significant technological and methodological advances at the cellular, subcellular, and molecular levels and the need to disclose the mechanical basis of biology. The application of mechanobiology to medicine (mechanomedicine) may help advance human health and improve diagnostics, treatment, and therapeutics of cancer.
- cancer
- metastasis
- endocytosis
- mechanobiology
- mechanomedicine
- tumor cell softness/deformability
- extracellular matrix stiffness
- fluid shear stress
- cytoskeletal/intermediate filament stress
- extracellular vesicles
1. A Need for Identification of New Potential Prognostic Markers
2. Tumor Biomarkers
3. Mechanobiology of Metastasis
This entry is adapted from the peer-reviewed paper 10.3390/ijms24054773
References
- Yang, J.; Weinberg, R.A. Epithelial-Mesenchymal Transition: At the Crossroads of Development and Tumor Metastasis. Dev. Cell 2008, 14, 818–829.
- Sleeman, J.P.; Nazarenko, I.; Thiele, W. Do All Roads Lead to Rome? Routes to Metastasis Development. Int. J. Cancer 2011, 128, 2511–2526.
- Cairns, R.A.; Khokha, R.; Hill, R.P. Molecular Mechanisms of Tumor Invasion and Metastasis: An Integrated View. Curr. Mol. Med. 2003, 3, 659–671.
- Weigelt, B.; Peterse, J.L.; van ’t Veer, L.J. Breast Cancer Metastasis: Markers and Models. Nat. Rev. Cancer 2005, 5, 591–602.
- Riihimaki, M.; Thomsen, H.; Hemminki, A.; Sundquist, K.; Hemminki, K.; Riihimäki, M.; Thomsen, H.; Hemminki, A.; Sundquist, K.; Hemminki, K.; et al. Comparison of Survival of Patients with Metastases from Known versus Unknown Primaries: Survival in Metastatic Cancer. BMC Cancer 2013, 13, 36.
- Lynch, J.A.; Venne, V.; Berse, B. Genetic Tests to Identify Risk for Breast Cancer. Semin. Oncol. Nurs. 2015, 31, 100–107.
- Vaidyanathan, K.; Vasudevan, D.M. Organ Specific Tumor Markers: What’s New? Indian J Clin Biochem 2012, 27, 110–120.
- Gurcan, M.N.; Boucheron, L.E.; Can, A.; Madabhushi, A.; Rajpoot, N.M.; Yener, B. Histopathological Image Analysis: A Review. IEEE Rev. Biomed. Eng. 2009, 2, 147–171.
- Wei, J.W.; Tafe, L.J.; Linnik, Y.A.; Vaickus, L.J.; Tomita, N.; Hassanpour, S. Pathologist-Level Classification of Histologic Patterns on Resected Lung Adenocarcinoma Slides with Deep Neural Networks. Sci. Rep. 2019, 9, 3358.
- Lang, E.V.; Berbaum, K.S.; Lutgendorf, S.K. Large-Core Breast Biopsy: Abnormal Salivary Cortisol Profiles Associated with Uncertainty of Diagnosis. Radiology 2009, 250, 631–637.
- Yankaskas, C.L.; Thompson, K.N.; Paul, C.D.; Vitolo, M.I.; Mistriotis, P.; Mahendra, A.; Bajpai, V.K.; Shea, D.J.; Manto, K.M.; Chai, A.C.; et al. A Microfluidic Assay for the Quantification of the Metastatic Propensity of Breast Cancer Specimens. Nat. Biomed. Eng. 2019, 3, 452–465.
- Murugan, A.K. MTOR: Role in Cancer, Metastasis and Drug Resistance. Semin. Cancer Biol. 2019, 59, 92–111.
- Wu, L.; Qu, X. Cancer Biomarker Detection: Recent Achievements and Challenges. Chem. Soc. Rev. 2015, 44, 2963–2997.
- Narayan Bhatt, A.; Farooque, A.; Verma, A. Cancer Biomarkers-Current Perspectives Role of Tumor Microenvironment in Treatment of Lymphoma and Myeloma View Project Metabolic Signaling Approaches for Anticancer Drug Target Discovery View Project. Artic. Indian J. Med. Res. 2010, 132, 129–149.
- Wang, F.; Fang, Q.; Ge, Z.; Yu, N.; Xu, S.; Fan, X. Common BRCA1 and BRCA2 Mutations in Breast Cancer Families: A Meta-Analysis from Systematic Review. Mol. Biol. Rep. 2012, 39, 2109–2118.
- De, P.; Mukhopadhyay, M.J. Study of the Chromosomal Abnormalities and Associated Complex Karyotypes in Hematological Cancer in the Population of West Bengal: A Prospective Observational Study. Indian J. Med. Paediatr. Oncol. 2021, 42, 261–267.
- Wang, C.; Bai, F.; Zhang, L.Z.; Scott, A.; Li, E.; Pei, X.H. Estrogen Promotes Estrogen Receptor Negative BRCA1-Deficient Tumor Initiation and Progression. Breast Cancer Res. 2018, 20, 74.
- Huang, J.; Duran, A.; Reina-Campos, M.; Valencia, T.; Castilla, E.A.; Müller, T.D.; Tschöp, M.H.; Moscat, J.; Diaz-Meco, M.T. Adipocyte P62/SQSTM1 Suppresses Tumorigenesis through Opposite Regulations of Metabolism in Adipose Tissue and Tumor. Cancer Cell 2018, 33, 770–784.e6.
- Szablewski, L. Glucose Transporters as Markers of Diagnosis and Prognosis in Cancer Diseases. Oncol. Rev. 2022, 16, 561.
- Pouliquen, D.; Boissard, A.; Coqueret, O.; Guette, C. Biomarkers of Tumor Invasiveness in Proteomics (Review). Int. J. Oncol. 2020, 57, 409–432.
- Wilt, T.J.; Scardino, P.T.; Carlsson, S.V.; Basch, E. Prostate-Specific Antigen Screening in Prostate Cancer: Perspectives on the Evidence. J. Natl. Cancer Inst. 2014, 106, 10.
- Brufsky, A.M.; Mayer, M.; Rugo, H.S.; Kaufman, P.A.; Tan-Chiu, E.; Tripathy, D.; Tudor, I.C.; Wang, L.I.; Brammer, M.G.; Shing, M.; et al. Central Nervous System Metastases in Patients with HER2-Positive Metastatic Breast Cancer: Incidence, Treatment, and Survival in Patients from RegistHER. Clin. Cancer Res. 2011, 17, 4834–4843.
- Kuba, S.; Ishida, M.; Nakamura, Y.; Yamanouchi, K.; Minami, S.; Taguchi, K.; Eguchi, S.; Ohno, S. Treatment and Prognosis of Breast Cancer Patients with Brain Metastases According to Intrinsic Subtype. Jpn. J. Clin. Oncol. 2014, 44, 1025–1031.
- Molinie, N.; Rubtsova, S.N.; Fokin, A.; Visweshwaran, S.P.; Rocques, N.; Polesskaya, A.; Schnitzler, A.; Vacher, S.; Denisov, E.V.; Tashireva, L.A.; et al. Cortical Branched Actin Determines Cell Cycle Progression. Cell Res. 2019, 29, 432–445.
- Geiger, T.; Cox, J.; Mann, M. Proteomic Changes Resulting from Gene Copy Number Variations in Cancer Cells. PLoS Genet. 2010, 6, e1001090.
- Guck, J.; Schinkinger, S.; Lincoln, B.; Wottawah, F.; Ebert, S.; Romeyke, M.; Lenz, D.; Erickson, H.M.; Ananthakrishnan, R.; Mitchell, D.; et al. Optical Deformability as an Inherent Cell Marker for Testing Malignant Transformation and Metastatic Competence. Biophys. J. 2005, 88, 3689–3698.
- Qi, D.; Gill, N.K.; Santiskulvong, C.; Sifuentes, J.; Dorigo, O.; Rao, J.; Taylor-Harding, B.; Wiedemeyer, W.R.; Rowat, A.C. Screening Cell Mechanotype by Parallel Microfiltration. Sci. Rep. 2015, 5, 17595.
- Byun, S.; Son, S.; Amodei, D.; Cermak, N.; Shaw, J.; Kang, J.H.; Hecht, V.C.; Winslow, M.M.; Jacks, T.; Mallick, P.; et al. Characterizing Deformability and Surface Friction of Cancer Cells. Proc. Natl. Acad. Sci. USA 2013, 110, 7580–7585.
- Paszek, M.J.; Zahir, N.; Johnson, K.R.; Lakins, J.N.; Rozenberg, G.I.; Gefen, A.; Reinhart-King, C.A.; Margulies, S.S.; Dembo, M.; Boettiger, D.; et al. Tensional Homeostasis and the Malignant Phenotype. Cancer Cell 2005, 8, 241–254.
- Guck, J.; Ananthakrishnan, R.; Mahmood, H.; Moon, T.J.; Cunningham, C.C.; Käs, J. The Optical Stretcher: A Novel Laser Tool to Micromanipulate Cells. Biophys. J. 2001, 81, 767.
- Gossett, D.R.; Tse, H.T.K.; Lee, S.A.; Ying, Y.; Lindgren, A.G.; Yang, O.O.; Rao, J.; Clark, A.T.; Di Carlo, D. Hydrodynamic Stretching of Single Cells for Large Population Mechanical Phenotyping. Proc. Natl. Acad. Sci. USA 2012, 109, 7630–7635.
- Lekka, M.; Laidler, P.; Gil, D.; Lekki, J.; Stachura, Z.; Hrynkiewicz, A.Z. Elasticity of Normal and Cancerous Human Bladder Cells Studied by Scanning Force Microscopy. Eur. Biophys. J. 1999, 28, 312–316.
- Mak, M.; Spill, F.; Kamm, R.D.; Zaman, M.H. Single-Cell Migration in Complex Microenvironments: Mechanics and Signaling Dynamics. J. Biomech. Eng. 2016, 138, 021004.
- Pachenari, M.; Seyedpour, S.M.; Janmaleki, M.; Shayan, S.B.; Taranejoo, S.; Hosseinkhani, H. Mechanical Properties of Cancer Cytoskeleton Depend on Actin Filaments to Microtubules Content: Investigating Different Grades of Colon Cancer Cell Lines. J. Biomech. 2014, 47, 373–379.
- Ketene, A.N.; Schmelz, E.M.; Roberts, P.C.; Agah, M. The Effects of Cancer Progression on the Viscoelasticity of Ovarian Cell Cytoskeleton Structures. Nanomedicine 2012, 8, 93–102.
- Ochalek, T.; Nordt, F.J.; Tullberg, K.; Burger, M.M. Correlation between Cell Deformability and Metastatic Potential in B16-F1 Melanoma Cell Variants. Cancer Res. 1988, 48, 5124–5128.
- Kramer, N.; Walzl, A.; Unger, C.; Rosner, M.; Krupitza, G.; Hengstschläger, M.; Dolznig, H. In Vitro Cell Migration and Invasion Assays. Mutat. Res.—Rev. Mutat. Res. 2013, 752, 10–24.
- Paul, C.D.; Mistriotis, P.; Konstantopoulos, K. Cancer Cell Motility: Lessons from Migration in Confined Spaces. Nat. Rev. Cancer 2017, 17, 131–140.
- Van Golen, K.L.; Wu, Z.F.; Xiao, X.T.; Bao, L.W.; Merajver, S.D. RhoC GTPase, a Novel Transforming Oncogene for Human Mammary Epithelial Cells That Partially Recapitulates the Inflammatory Breast Cancer Phenotype. Cancer Res. 2000, 60, 5832–5838.
- Lin, M.; DiVito, M.M.; Merajver, S.D.; Boyanapalli, M.; van Golen, K.L. Regulation of Pancreatic Cancer Cell Migration and Invasion by RhoC GTPase and Caveolin-1. Mol. Cancer 2005, 4, 21.
- Shelby, J.P.; White, J.; Ganesan, K.; Rathod, P.K.; Chiu, D.T. A Microfluidic Model for Single-Cell Capillary Obstruction by Plasmodium Falciparum-Infected Erythrocytes. Proc. Natl. Acad. Sci. USA 2003, 100, 14618–14622.
- Lautscham, L.A.; Kämmerer, C.; Lange, J.R.; Kolb, T.; Mark, C.; Schilling, A.; Strissel, P.L.; Strick, R.; Gluth, C.; Rowat, A.C.; et al. Migration in Confined 3D Environments Is Determined by a Combination of Adhesiveness, Nuclear Volume, Contractility, and Cell Stiffness. Biophys. J. 2015, 109, 900–913.
- Mak, M.; Reinhart-King, C.A.; Erickson, D. Elucidating Mechanical Transition Effects of Invading Cancer Cells with a Subnucleus-Scaled Microfluidic Serial Dimensional Modulation Device. Lab Chip 2013, 13, 340–348.
- Albini, A.; Benelli, R. The Chemoinvasion Assay: A Method to Assess Tumor and Endothelial Cell Invasion and Its Modulation. Nat. Protoc. 2007, 2, 504–511.
- McEwan, R.N.; Kleinman, H.K.; Martin, G.R. A Rapid in Vitro Assay for Quantitating the Invasive Potential of Tumor Cells. Cancer Res. 1987, 47, 3239–3245.
- Justus, C.R.; Leffler, N.; Ruiz-Echevarria, M.; Yang, L.V. In Vitro Cell Migration and Invasion Assays. J. Vis. Exp. 2014, 88, 51046.
- Sieuwerts, A.M.; Klijn, J.G.M.; Foekens, J.A. Assessment of the Invasive Potential of Human Gynecological Tumor Cell Lines with the in Vitro Boyden Chamber Assay: Influences of the Ability of Cells to Migrate through the Filter Membrane. Clin. Exp. Metastasis 1997, 15, 53–62.
- Nyström, M.L.; Thomas, G.J.; Stone, M.; Mackenzie, I.C.; Hart, I.R.; Marshall, J.F. Development of a Quantitative Method to Analyse Tumour Cell Invasion in Organotypic Culture. J. Pathol. 2005, 205, 468–475.
- Ayala, I.; Baldassarre, M.; Caldieri, G.; Buccione, R. Invadopodia: A Guided Tour. Eur. J. Cell Biol. 2006, 85, 159–164.
- Artym, V.V.; Yamada, K.M.; Mueller, S.C. ECM Degradation Assays for Analyzing Local Cell Invasion. Methods Mol. Biol. 2009, 522, 211–219.
- Merkher, Y.; Horesh, Y.; Abramov, Z.; Shleifer, G.; Ben-Ishay, O.; Kluger, Y.; Weihs, D. Rapid Cancer Diagnosis and Early Prognosis of Metastatic Risk Based on Mechanical Invasiveness of Sampled Cells. Ann. Biomed. Eng. 2020, 48, 2846–2858.
- Merkher, Y.; Weihs, D. Proximity of Metastatic Cells Enhances Their Mechanobiological Invasiveness. Ann. Biomed. Eng. 2017, 45, 1399–1406.
- Merkher, Y.; Alvarez-Elizondo, M.B.; Weihs, D. Taxol Reduces Synergistic, Mechanobiological Invasiveness of Metastatic Cells. Converg. Sci. Phys. Oncol. 2017, 3, 044002.
- Merkher, Y.; Kontareva, E.; Melekhova, A.; Leonov, S. Abstract PO-042: Nanoparticles Imaging for Cancer Metastasis Diagnosis. Clin. Cancer Res. 2021, 27, PO-042.
- Merkher Yulia; Kontareva Elizaveta; Bogdan Elizaveta; Achkasov Konstantin; Grolman Joshua; Leonov Sergey Nanoparticle Cellular Endocytosis as Potential Prognostic Biomarker for Cancer Progression. FEBS Open Bio 2021, 11, 429–430.
- Li, Y.; Zhang, H.; Merkher, Y.; Chen, L.; Liu, N.; Leonov, S.; Chen, Y. Recent Advances in Therapeutic Strategies for Triple-Negative Breast Cancer. J. Hematol. Oncol. 2022, 15, 121.
