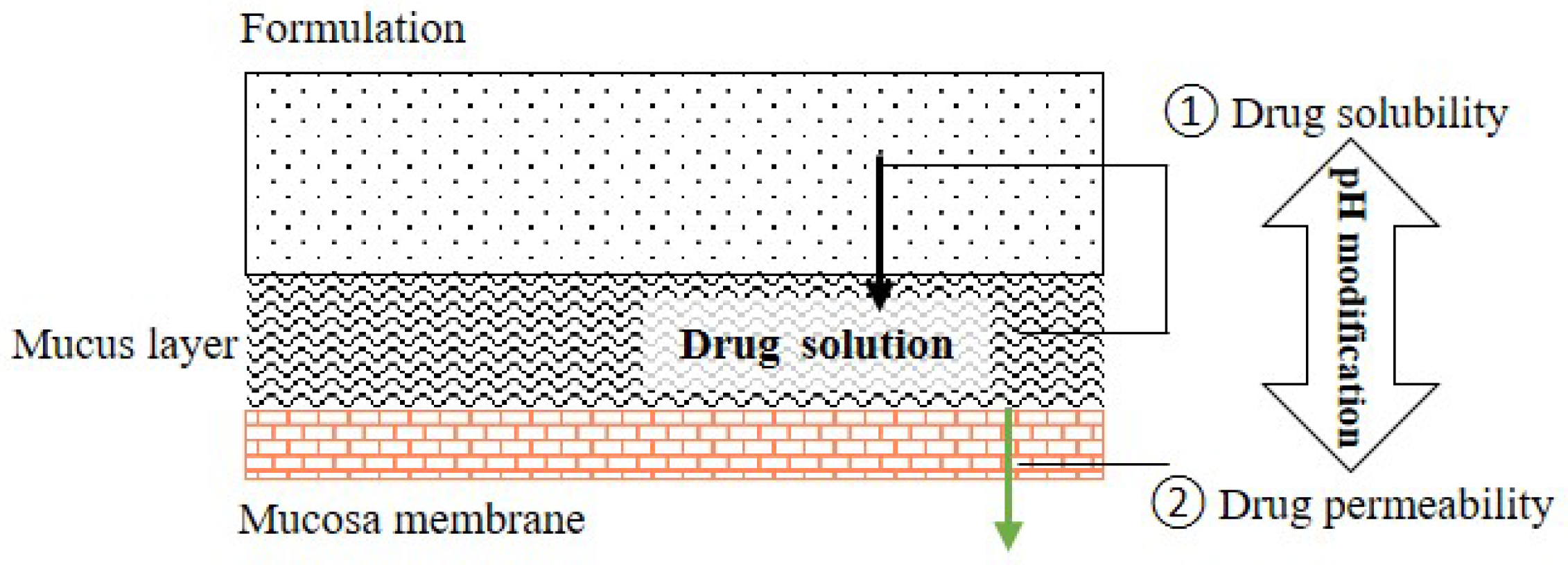
Many drug candidates are poorly water-soluble. Microenvironmental pH (pHM) modification in buccal/sublingual dosage forms has attracted increasing interest as a promising pharmaceutical strategy to enhance the oral mucosal absorption of drugs with pH-dependent solubility. Optimizing drug absorption at the oral mucosa using pHM modification is considered to be a compromise between drug solubility and drug lipophilicity (Log D)/permeation. To create a desired pHM around formulations during the dissolution process, a suitable amount of pH modifiers should be added in the formulations, and the appropriate methods of pHM measurement are required.
- microenvironmental pH modification
- buccal/sublingual dosage form
- solubility
1. Introduction
2. Concept of Microenvironmental pH (pHM) Modification in the Buccal/Sublingual Dosage Forms
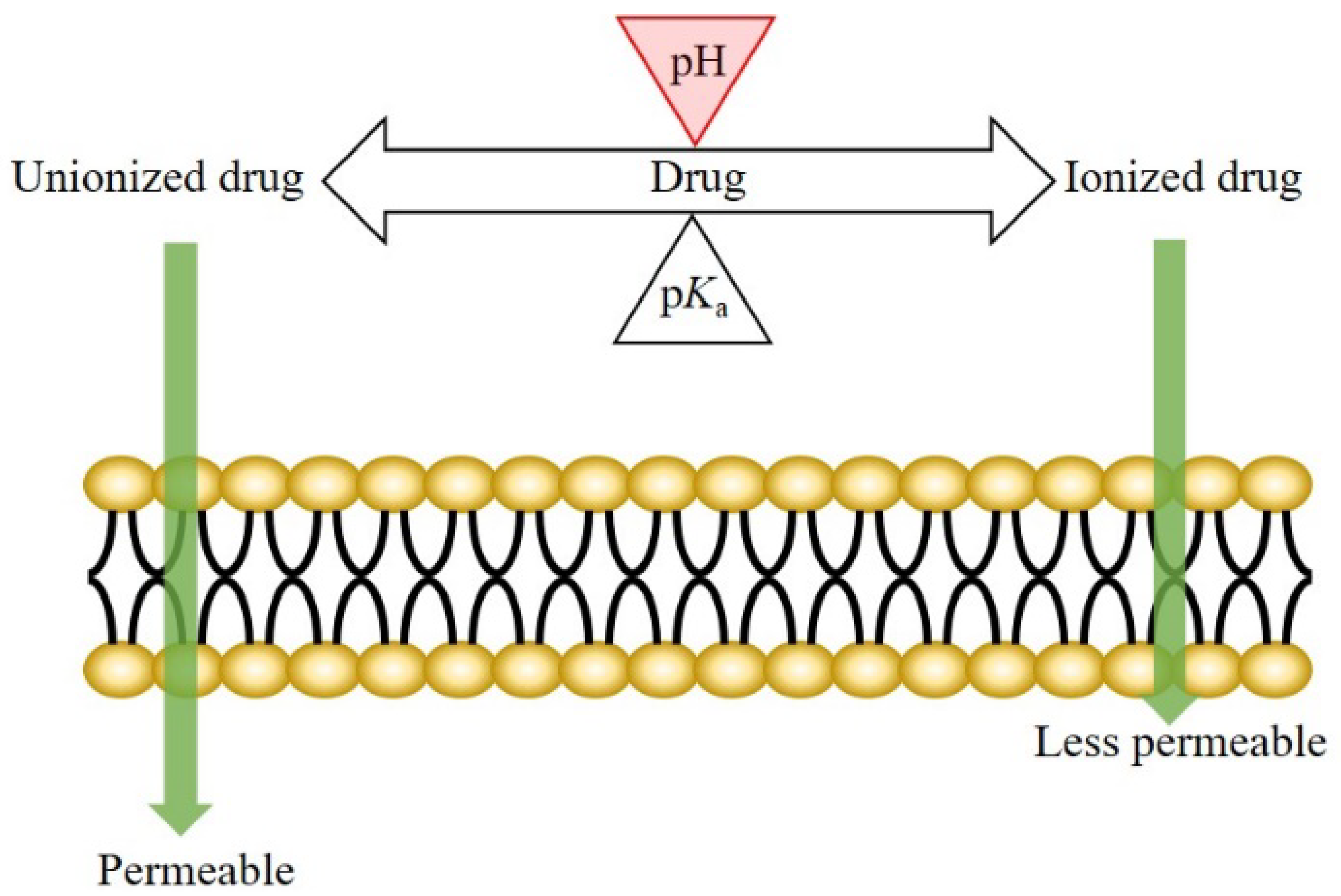
2.1. Theory: pH-Dependent Dissolution and Permeation
2.2. pHmax Concept
2.3. Microenvironmental pH Modification in Buccal/Sublingual Dosage Forms
3. Properties of Saliva Associated with pH Modification
The main functions of saliva are to maintain oral health and help to build and maintain the health of hard and soft tissues. Approximately 99% of saliva is water, and the other 1% consists of a variety of electrolytes and proteins [30][31]. Regarding buccal/sublingual drug delivery, saliva provides a water-rich environment that facilitates in the drug dissolution and release from buccal/sublingual formulations before the drugs permeate through the membrane of oral mucosa [32]. To achieve a successful pHM modification in buccal/sublingual formulations, some properties of saliva should be taken into consideration during the formulation design.
3.1. pH and Buffer Capacity of Saliva
3.2. Secretion Rate of Saliva and Thickness of Salivary Film
4. Drug Candidate and pH Modifier for Buccal/Sublingual Dosage Forms
4.1. Drug Candidate
4.2. pH Modifier
5. Methods for Microenvironmental pH Measurement
5.1. pH Electrode Approach
5.2. Computer-Enhanced Color Images Method
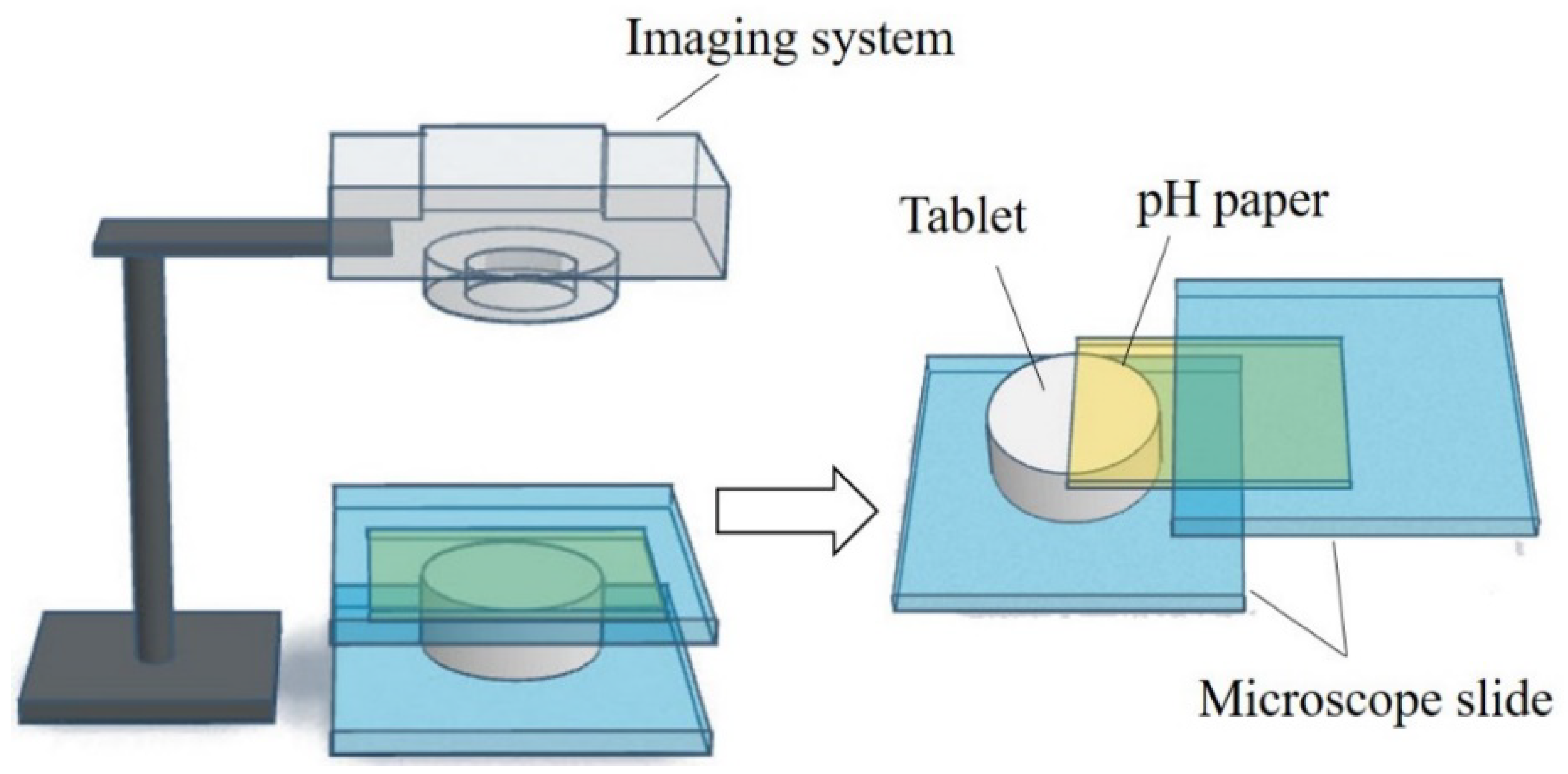
5.3. UV/Vis Imaging Method
6. Microenvironmental pH (pHM) Modification Methods
6.1. Microenvironmental pH Modification Using Acidifying/Alkalizing Agents
6.2. Microenvironmental pH Modification Using Buffering Agents
6.3. Microenvironmental pH Modification Using Effervescence
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics15020637
References
- Macedo, A.S.; Castro, P.M.; Roque, L.; Thomé, N.G.; Reis, C.P.; Pintado, M.E.; Fonte, P. Novel and Revisited Approaches in Nanoparticle Systems for Buccal Drug Delivery. J. Control. Release 2020, 320, 125–141.
- Madhav, N.V.S.; Shakya, A.K.; Shakya, P.; Singh, K. Orotransmucosal Drug Delivery Systems: A Review. J. Control. Release 2009, 140, 2–11.
- Lam, J.K.W.; Xu, Y.; Worsley, A.; Wong, I.C.K. Oral Transmucosal Drug Delivery for Pediatric Use. Adv. Drug Deliv. Rev. 2014, 73, 50–62.
- Zhang, H.; Zhang, J.; Streisand, J.B. Oral Mucosal Drug Delivery. Clin. Pharmacokinet. 2002, 41, 661–680.
- Loftsson, T.; Brewster, M.E. Pharmaceutical Applications of Cyclodextrins: Basic Science and Product Development. J. Pharm. Pharmacol. 2010, 62, 1607–1621.
- Taniguchi, C.; Kawabata, Y.; Wada, K.; Yamada, S.; Onoue, S. Microenvironmental PH-Modification to Improve Dissolution Behavior and Oral Absorption for Drugs with PH-Dependent Solubility. Expert Opin. Drug Deliv. 2014, 11, 505–516.
- Yang, M.; He, S.; Fan, Y.; Wang, Y.; Ge, Z.; Shan, L.; Gong, W.; Huang, X.; Tong, Y.; Gao, C. Microenvironmental PH-Modified Solid Dispersions to Enhance the Dissolution and Bioavailability of Poorly Water-Soluble Weakly Basic GT0918, a Developing Anti-Prostate Cancer Drug: Preparation, Characterization and Evaluation in Vivo. Int. J. Pharm. 2014, 475, 97–109.
- Badawy, S.I.F.; Hussain, M.A. Microenvironmental PH Modulation in Solid Dosage Forms. J. Pharm. Sci. 2007, 96, 948–959.
- Doherty, C.; York, P. Microenvironmental PH Control of Drug Dissolution. Int. J. Pharm. 1989, 50, 223–232.
- Younes, N.F.; El Assasy, A.E.-H.I.; Makhlouf, A.I.A. Microenvironmental PH-Modified Amisulpride-Labrasol Matrix Tablets: Development, Optimization and in Vivo Pharmacokinetic Study. Drug Deliv. Transl. Res. 2020, 11, 103–117.
- Onoue, S.; Inoue, R.; Taniguchi, C.; Kawabata, Y.; Yamashita, K.; Wada, K.; Yamauchi, Y.; Yamada, S. Improved Dissolution and Pharmacokinetic Behavior of Dipyridamole Formulation with Microenvironmental PH-Modifier under Hypochlorhydria. Int. J. Pharm. 2012, 426, 61–66.
- Mitra, A.; Kesisoglou, F.; Beauchamp, M.; Zhu, W.; Chiti, F.; Wu, Y. Using Absorption Simulation and Gastric PH Modulated Dog Model for Formulation Development To Overcome Achlorhydria Effect. Mol. Pharm. 2011, 8, 2216–2223.
- Koziolek, M.; Grimm, M.; Becker, D.; Iordanov, V.; Zou, H.; Shimizu, J.; Wanke, C.; Garbacz, G.; Weitschies, W. Investigation of PH and Temperature Profiles in the GI Tract of Fasted Human Subjects Using the Intellicap® System. J. Pharm. Sci. 2015, 104, 2855–2863.
- Baliga, S.; Muglikar, S.; Kale, R. Salivary PH: A Diagnostic Biomarker. J. Indian Soc. Periodontol. 2013, 17, 461–465.
- Ciolino, L.A.; McCauley, H.A.; Fraser, D.B.; Wolnik, K.A. The Relative Buffering Capacities of Saliva and Moist Snuff: Implications for Nicotine Absorption. J. Anal. Toxicol. 2001, 25, 15–25.
- Proctor, G.B. The Physiology of Salivary Secretion. Periodontology 2000 2016, 70, 11–25.
- Dawes, C. Physiological Factors Affecting Salivary Flow Rate, Oral Sugar Clearance, and the Sensation of Dry Mouth in Man. J. Dent. Res. 1987, 66, 648–653.
- Dokoumetzidis, A.; Macheras, P. A Century of Dissolution Research: From Noyes and Whitney to the Biopharmaceutics Classification System. Int. J. Pharm. 2006, 321, 1–11.
- Avdeef, A. Solubility of Sparingly-Soluble Ionizable Drugs. Adv. Drug Deliv. Rev. 2007, 59, 568–590.
- Bassi, P.; Kaur, G. PH Modulation: A Mechanism to Obtain PH-Independent Drug Release. Expert Opin. Drug Deliv. 2010, 7, 845–857.
- Pather, S.I.; Rathbone, M.J.; Şenel, S. Current Status and the Future of Buccal Drug Delivery Systems. Expert Opin. Drug Deliv. 2008, 5, 531–542.
- Mashru, R.; Sutariya, V.; Sankalia, M.; Sankalia, J. Transbuccal Delivery of Lamotrigine across Porcine Buccal Mucosa: In Vitro Determination of Routes of Buccal Transport. J. Pharm. Pharm. Sci. 2005, 8, 54–62.
- Birudaraj, R.a.j.; Berner, B.; Shen, S.; Li, X. Buccal Permeation of Buspirone: Mechanistic Studies on Transport Pathways. J. Pharm. Sci. 2005, 94, 70–78.
- Nielsen, H.M.; Rassing, M.R. Nicotine Permeability across the Buccal TR146 Cell Culture Model and Porcine Buccal Mucosa in Vitro: Effect of PH and Concentration. Eur. J. Pharm. Sci. 2002, 16, 151–157.
- Thomae, A.V.; Wunderli-Allenspach, H.; Krämer, S.D. Permeation of Aromatic Carboxylic Acids across Lipid Bilayers: The PH-Partition Hypothesis Revisited. Biophys. J. 2005, 89, 1802–1811.
- Shore, P.A.; Brodie, B.B.; Hogben, C.A.M. The Gastric Secretion of Drugs: A Ph Partition Hypothesis. J. Pharmacol. Exp. Ther. 1957, 119, 361–369.
- Wang, Y.; Zuo, Z.; Chen, X.; Tomlinson, B.; Chow, M.S.S. Improving Sublingual Delivery of Weak Base Compounds Using PHmax Concept: Application to Propranolol. Eur. J. Pharm. Sci. 2010, 39, 272–278.
- Meng-Lund, E.; Jacobsen, J.; Andersen, M.B.; Jespersen, M.L.; Karlsson, J.-J.; Garmer, M.; Jørgensen, E.B.; Holm, R. Conscious and Anaesthetised Göttingen Mini-Pigs as an in-Vivo Model for Buccal Absorption—PH-Dependent Absorption of Metoprolol from Bioadhesive Tablets. Drug Dev. Ind. Pharm. 2014, 40, 604–610.
- Holm, R.; Meng-Lund, E.; Andersen, M.B.; Jespersen, M.L.; Karlsson, J.-J.; Garmer, M.; Jørgensen, E.B.; Jacobsen, J. In Vitro, Ex Vivo and in Vivo Examination of Buccal Absorption of Metoprolol with Varying PH in TR146 Cell Culture, Porcine Buccal Mucosa and Göttingen Minipigs. Eur. J. Pharm. Sci. 2013, 49, 117–124.
- Dodds, M.; Roland, S.; Edgar, M.; Thornhill, M. Saliva A Review of Its Role in Maintaining Oral Health and Preventing Dental Disease. BDJ Team 2015, 2, 15123.
- de Almeida, P.D.V.; Grégio, A.M.T.; Machado, M.A.; de Lima, A.A.S.; Azevedo, L.R. Saliva Composition and Functions: A Comprehensive Review. J. Contemp. Dent. Pract. 2008, 9, 72–80.
- Patel, V.F.; Liu, F.; Brown, M.B. Advances in Oral Transmucosal Drug Delivery. J. Control. Release 2011, 153, 106–116.
- Aframian, D.; Davidowitz, T.; Benoliel, R. The Distribution of Oral Mucosal PH Values in Healthy Saliva Secretors. Oral Dis. 2006, 12, 420–423.
- Tenovuo, J. Salivary Parameters of Relevance for Assessing Caries Activity in Individuals and Populations. Community Dent. Oral Epidemiol. 1997, 25, 82–86.
- Lazarchik, D.A.; Filler, S.J. Effects of Gastroesophageal Reflux on the Oral Cavity. Am. J. Med. 1997, 103, 107S–113S.
- Bardow, A.; Moe, D.; Nyvad, B.; Nauntofte, B. The Buffer Capacity and Buffer Systems of Human Whole Saliva Measured without Loss of CO2. Arch. Oral Biol. 2000, 45, 1–12.
- Pedersen, A.M.L.; Sørensen, C.E.; Proctor, G.B.; Carpenter, G.H.; Ekström, J. Salivary Secretion in Health and Disease. J. Oral Rehabil. 2018, 45, 730–746.
- Pijpe, J.; Kalk, W.W.I.; Bootsma, H.; Spijkervet, F.K.L.; Kallenberg, C.G.M.; Vissink, A. Progression of Salivary Gland Dysfunction in Patients with Sjögren’s Syndrome. Ann. Rheum. Dis. 2007, 66, 107–112.
- Xiang, J.; Fang, X.; Li, X. Transbuccal Delivery of 2′,3′-Dideoxycytidine: In Vitro Permeation Study and Histological Investigation. Int. J. Pharm. 2002, 231, 57–66.
- Deneer, V.H.M.; Drese, G.B.; Roemelé, P.E.H.; Verhoef, J.C.; Lie-A-Huen, L.; Kingma, J.H.; Brouwers, J.R.B.J.; Junginger, H.E. Buccal Transport of Flecainide and Sotalol: Effect of a Bile Salt and Ionization State. Int. J. Pharm. 2002, 241, 127–134.
- Easa, N.; Alany, R.G.; Carew, M.; Vangala, A. A Review of Non-Invasive Insulin Delivery Systems for Diabetes Therapy in Clinical Trials over the Past Decade. Drug Discov. Today 2019, 24, 440–451.
- Morales, J.O.; Brayden, D.J. Buccal Delivery of Small Molecules and Biologics: Of Mucoadhesive Polymers, Films, and Nanoparticles. Curr. Opin. Pharmacol. 2017, 36, 22–28.
- Heinemann, L.; Jacques, Y. Oral Insulin and Buccal Insulin: A Critical Reappraisal. J. Diabetes Sci. Technol. 2009, 3, 568–584.
- Zamora, W.J.; Curutchet, C.; Campanera, J.M.; Luque, F.J. Prediction of PH-Dependent Hydrophobic Profiles of Small Molecules from Miertus–Scrocco–Tomasi Continuum Solvation Calculations. J. Phys. Chem. B 2017, 121, 9868–9880.
- Zamora, W.J.; Campanera, J.M.; Luque, F.J. Development of a Structure-Based, PH-Dependent Lipophilicity Scale of Amino Acids from Continuum Solvation Calculations. J. Phys. Chem. Lett. 2019, 10, 883–889.
- Xing, L.; Glen, R.C. Novel Methods for the Prediction of LogP, PKa, and LogD. J. Chem. Inf. Comput. Sci. 2002, 42, 796–805.
- Iwanaga, K.; Kato, S.; Miyazaki, M.; Kakemi, M. Enhancing the Intestinal Absorption of Poorly Water-Soluble Weak-Acidic Compound by Controlling Local PH. Drug Dev. Ind. Pharm. 2013, 39, 1887–1894.
- Henderson—Hasselbalch Equation. In Manual of Pharmacologic Calculations: With Computer Programs; Tallarida, R.J.; Murray, R.B. (Eds.) Springer: New York, NY, USA, 1987; pp. 74–75. ISBN 978-1-4612-4974-0.
- The United States. Pharmacopeial Convention Excipients: USP and NF Excipients, Listed by Functional Category. In United States Pharmacopeia and National Formulary; The United States Pharmacopeial Convention: North Bethesda, MD, USA, 2016; p. 7490.
- Food and Drug Administration. FDA-Inactive Ingredient Search for Approved Drug Products Search. Available online: https://www.accessdata.fda.gov/scripts/cder/iig/index.cfm (accessed on 1 October 2022).
- Elagamy, H.I.; Essa, E.A.; Nouh, A.; El Maghraby, G.M. Development and Evaluation of Rapidly Dissolving Buccal Films of Naftopidil: In Vitro and in Vivo Evaluation. Drug Dev. Ind. Pharm. 2019, 45, 1695–1706.
- Zhang, C.; Liu, Y.; Li, W.; Gao, P.; Xiang, D.; Ren, X.; Liu, D. Mucoadhesive Buccal Film Containing Ornidazole and Dexamethasone for Oral Ulcers: In Vitro and in Vivo Studies. Pharm. Dev. Technol. 2019, 24, 118–126.
- Nafee, N.A.; Ismail, F.A.; Boraie, N.A.; Mortada, L.M. Mucoadhesive Delivery Systems. I. Evaluation of Mucoadhesive Polymers for Buccal Tablet Formulation. Drug Dev. Ind. Pharm. 2004, 30, 985–993.
- Patel, V.M.; Prajapati, B.G.; Patel, H.V.; Patel, K.M. Mucoadhesive Bilayer Tablets of Propranolol Hydrochloride. AAPS PharmSciTech 2007, 8, E203–E208.
- Mohamad, S.A.; Abdelkader, H.; Elrehany, M.; Mansour, H.F. Vitamin B12 Buccoadhesive Tablets: Auspicious Non-Invasive Substitute for Intra Muscular Injection: Formulation, in Vitro and in Vivo Appraisal. Drug Dev. Ind. Pharm. 2019, 45, 244–251.
- Nafee, N.A.; Ismail, F.A.; Boraie, N.A.; Mortada, L.M. Mucoadhesive Buccal Patches of Miconazole Nitrate: In Vitro/in Vivo Performance and Effect of Ageing. Int. J. Pharm. 2003, 264, 1–14.
- Chen, G.; Bunt, C.; Wen, J. Mucoadhesive Polymers-Based Film as a Carrier System for Sublingual Delivery of Glutathione. J. Pharm. Pharmacol. 2015, 67, 26–34.
- Durfee, S.; Messina, J.; Khankari, R. Fentanyl Effervescent Buccal Tablets. Am. J. Drug Deliv. 2006, 4, 1–5.
- He, S.; Østergaard, J.; Ashna, M.; Nielsen, C.U.; Jacobsen, J.; Mu, H. Microenvironmental PH Modifying Films for Buccal Delivery of Saquinavir: Effects of Organic Acids on PH and Drug Release in Vitro. Int. J. Pharm. 2020, 585, 119567.
- Fouad, S.A.; Shamma, R.N.; Basalious, E.B.; El-Nabarawi, M.A.; Tayel, S.A. Novel Instantly-Soluble Transmucosal Matrix (ISTM) Using Dual Mechanism Solubilizer for Sublingual and Nasal Delivery of Dapoxetine Hydrochloride: In-Vitro/in-Vivo Evaluation. Int. J. Pharm. 2016, 505, 212–222.
- Aldawsari, H.M.; Badr-Eldin, S.M. Enhanced Pharmacokinetic Performance of Dapoxetine Hydrochloride via the Formulation of Instantly-Dissolving Buccal Films with Acidic PH Modifier and Hydrophilic Cyclodextrin: Factorial Analysis, in Vitro and in Vivo Assessment. J. Adv. Res. 2020, 24, 281–290.
- Avdeef, A.; Berger, C.M. PH-Metric Solubility.: 3. Dissolution Titration Template Method for Solubility Determination. Eur. J. Pharm. Sci. 2001, 14, 281–291.
- Zur, M.; Gasparini, M.; Wolk, O.; Amidon, G.L.; Dahan, A. The Low/High BCS Permeability Class Boundary: Physicochemical Comparison of Metoprolol and Labetalol. Mol. Pharm. 2014, 11, 1707–1714.
- Advankar, A.; Maheshwari, R.; Tambe, V.; Todke, P.; Raval, N.; Kapoor, D.; Tekade, R.K. Chapter 13—Specialized Tablets: Ancient History to Modern Developments. In Drug Delivery Systems; Tekade, R.K., Ed.; Academic Press: Cambridge, MA, USA, 2019; pp. 615–664. ISBN 978-0-12-814487-9.
- Darwish, M.; Tempero, K.; Jiang, J.G.; Simonson, P.G. Relative Bioavailability of Fentanyl Following Various Dosing Regimens of Fentanyl Buccal Tablet in Healthy Japanese Volunteers. Arch. Drug Inf. 2008, 1, 56–62.
- Freye, E. A New Transmucosal Drug Delivery System for Patients with Breakthrough Cancer Pain: The Fentanyl Effervescent Buccal Tablet. Available online: https://www.dovepress.com/a-new-transmucosal-drug-delivery-system-for-patients-with-breakthrough-peer-reviewed-article-JPR (accessed on 30 September 2020).
