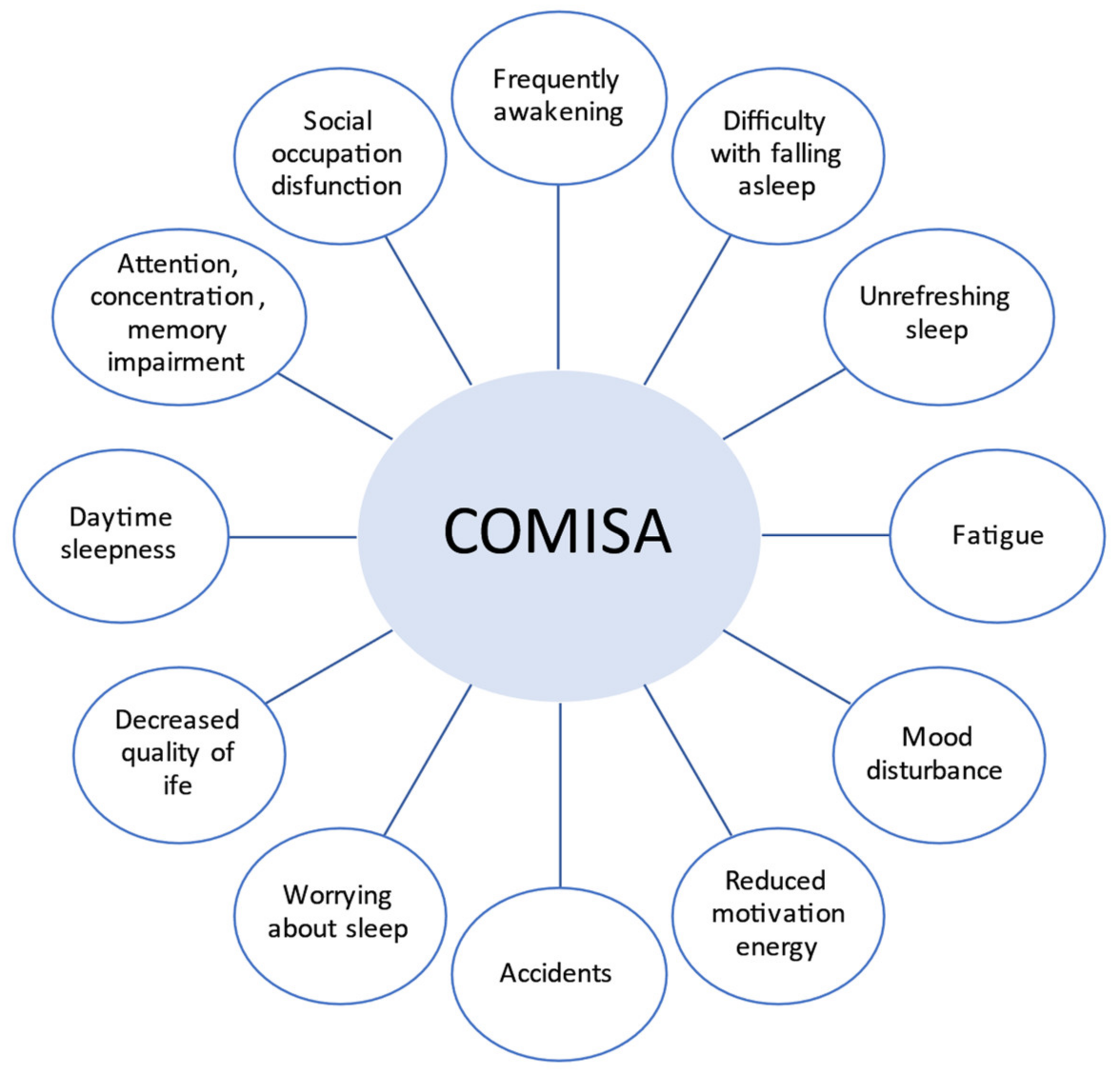
Obstructive sleep apnea (OSA) and insomnia are the two most common sleep disorders among the general population, and they may often coexist in patients with sleep-disordered breathing (SDB). The higher prevalence of insomnia symptoms in patients with OSA (40–60%) compared to that observed in the general population has thus led researchers to identify a new disorder named comorbid insomnia and OSA (COMISA), whose true burden has been so far largely underestimated. The combined treatment of COMISA patients with positive-airway pressure ventilation (PAP) with cognitive behavioral therapy for insomnia (CBTi) has shown a better patient outcome compared to that obtained with a single treatment. Furthermore, recent evidence has shown that an innovative patient-centered approach taking into consideration patient characteristics, treatment preferences and accessibility to treatment is recommended to optimize clinical management of COMISA patients. However, in this complex mosaic, many other sleep disorders may overlap with COMISA, so there is an urgent need for further research to fully understand the impact of these therapies on outcomes for OSA patients with comorbidity. In light of this need, the major sleep disorders comorbid with OSA and the recent advances in the management of these insomniac patients are discussed.
- sleep disorder breathing
- COMISA
- clinical management
1. Introduction
2. Clinical Features and Relationships
2.1. Insomnia and Sleep Apnea
| A Chronic Insomnia Disorder Diagnosis Would Apply Only When: |
| The insomnia symptoms show some independence in their onset or variation over time from the other symptoms of the co-occurring sleep disorder. When insomnia symptoms persist despite marked symptom improvement of the co-occurring sleep disorder following adequate treatment. A chronic insomnia disorder diagnosis would not apply when effective treatment of the coincident sleep disorder resolves the insomnia symptoms. |
2.2. Patients Phenotypes
This entry is adapted from the peer-reviewed paper 10.3390/ijerph18179248
References
- Smith, S.; Sullivan, K.; Hopkins, W.; Douglas, J. Frequency of insomnia report in patients with obstructive sleep apnoea hypopnea syndrome (OSAHS). Sleep Med. 2004, 5, 449–456.
- Ohayon, M. Epidemiological Overview of sleep Disorders in the General Population. Sleep Med. Res. 2011, 2, 1–9.
- Wickwire, E.M.; Collop, N.A. Insomnia and sleep-related breathing disorders. Chest 2010, 137, 1449–1463.
- Bjornsdottir, E.; Janson, C.; Sigurdsson, F.; Gehrman, P.; Perlis, M.; Juliusson, S.; Arnardottir, E.S.; Kuna, S.T.; Pack, A.I.; Gislason, T. Symptoms of insomnia among patients with obstructive sleep apnea before and after two years of positive air way pressure treatment. Sleep 2013, 36, 1901–1909.
- Nguyen, X.; Chaskalovic, J.; Rakotonanahary, D.; Fleurya, B. Insomnia symptoms and CPAP compliance in OSAS patients: A descriptive study using Data Mining methods. Sleep Med. 2010, 11, 777–784.
- Williams, J.; Roth, A.; Vatthauer, K.; McCrae, C.S. Cognitive Behavioral Treatment of Insomnia. Chest 2013, 143, 554–565.
- Krakov, B.; Melendrez, D.; Ferreira, E.; Clark, J.; Warner, T.D.; Sisley, B.; Sklar, D. Prevalence of insomnia symptoms in patients with sleep-disordered breathing. Chest 2001, 120, 1923–1929.
- Tasbakan, M.S.; Gunduz, C.; Pirildar, S.; Basoglu, O.K. Quality of life in obstructive sleep apnea is related to female gender and comorbid insomnia. Sleep Breath. 2018, 22, 1013–1020.
- Lichstein, K.L.; Justin Thomas, S.; Woosley, J.A.; Geyer, J.D. Co-occurring insomnia and obstructive sleep apnea. Sleep Med. 2013, 14, 824–829.
- Sateia, M. (Ed.) The International Classification of Sleep Disorders, 3rd ed.; American Academy of Sleep Medicine: Darien, CT, USA, 2014; pp. 13–18.
- Janssen, H.C.J.P.; Venekamp, L.N.; Peeters, G.A.M.; Pijpers, A.; Pevernagie, D.A.A. Management of insomnia in sleep disorder breathing. Eur. Respir. Rev. 2019, 28, 190080.
- Bahr, K.; Camara, R.J.A.; Gouveris, H.; Tuin, I. Current treatment of comorbid insomnia and obstructive sleep apnea with CBTI and PAP-therapy: A systematic review. Front. Neurol. 2018, 9, 804.
- Guilleminault, C.; Eldridge, F.L.; Dement, W.C. Insomnia with sleep apnea: A new syndrome. Science 1973, 181, 856–858.
- Luyster, F.S.; Buysse, D.J.; Strollo, P.J. Comorbid insomnia and obstructive sleep apnea: Challenges for clinical practice and research. J. Clin. Sleep Med. 2010, 6, 196–204.
- Ong, J.C.; Crawford, M.R. Insomnia and obstructive sleep apnea. Sleep Med. Clin. 2013, 8, 389–398.
- Mundt, J.; Eisenschenk, S.; Robinson, M. Severity and likelihood of chronic pain in individuals with obstructive sleep apnea and insomnia. J. Pain 2017, 18, 573.
- Krell, S.B.; Kapur, V.K. Insomnia complaints in patients evaluated for obstructive sleep apnea. Sleep Breath. 2005, 9, 104–110.
- Lin, C.-L.; Liu, T.C.; Chung, C.H.; Chen, W.C. Association between sleep disorders (SD) and hypertension in Taiwan: A nationwide population-based retrospective cohort study. J. Hum. Hypertens. 2017, 31, 220–224.
- Vozoris, N.T. Sleep apnea-plus: Prevalence, risk factors, and association with cardiovascular disease using United States population-level data. Sleep Med. 2012, 13, 637–644.
- Meira e Cruz, M.; Seixas, L.; Santos, A.; Garrido, J.; Lopes, Y.; Paolombini, L.; Gozal, D.; Galtieri, R.; Sales, C. Cardiovascular and metabolic risk in patients with suspected comorbid insomnia and obstructive sleep apnea (COMISA). Sleep 2021, 44, A189–A190.
- Gupta, M.A.; Knapp, K. Cardiovascular and Psychiatric Morbidity in Obstructive Sleep Apnea (OSA) with Insomnia (Sleep Apnea Plus) versus Obstructive Sleep Apnea without Insomnia: A Case-Control Study from Nationally Representative US sample. PLoS ONE 2014, 9, e90021.
- Cho, Y.W.; Kim, K.T.; Moon, H.J.; Korostyshevskiy, V.R.; Motamedi, G.K.; Yang, K.I. Comorbid insomnia with obstructive sleep apnea: Clinical characteristics and risk factors. J. Clin. Sleep Med. 2018, 14, 409–417.
- Lang, C.J.; Appleton, S.L.; Vakulin, A.; McEvoy, R.D.; Witter, G.A.; Martin, S.A.; Catcheside, P.G.; Antic, N.A.; Lack, L.; Adams, R.J. Comorbid OSA and insomnia increases depression prevalence and severity in men. Respirology 2017, 22, 1407–1415.
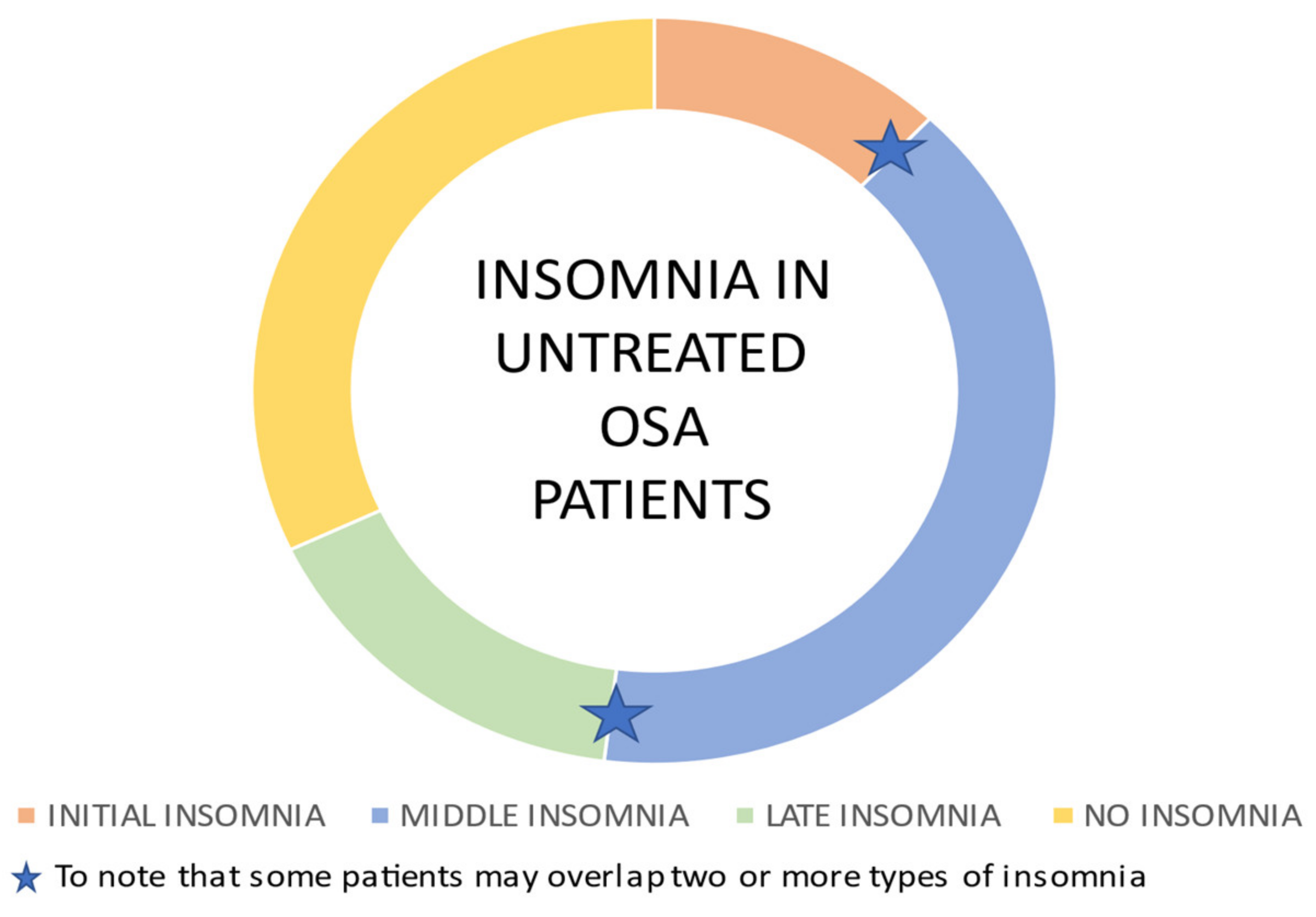
- Chung, K.F. Insomnia subtypes and their relationships to daytime sleepiness in patients with obstructive sleep apnea. Respiration 2005, 72, 460–465.
- Sivertsen, B.; Bjornsdòttir, E.; Øverland, S.; Bjorvtan, B.; Salo, P. The joint contribution of insomnia and obstructive sleep apnea on sickness absence. J. Sleep Res. 2013, 22, 223–230.
- Bjornsdottir, E.; Keenan, T.B.; Eysteinsdottir, B.; Arnardottir, E.S.; Janson, C.; Gislason, T.; Sigurdsson, J.F.; Kuna, S.T.; Pack, A.I.; Benediktsdottir, B. Quality of life among untreated sleep apnea patients compared to the general population and changes after treatment with positive air way pressure. J. Sleep Res. 2015, 24, 328–338.
- Saaresranta, T.; Hedner, J.; Bonsignore, M.R.; Riha, R.L.; McNicholas, W.T.; Penzel, T.; Anttalainen, U.; Kvamme, J.A.; Pretl, M.; Sliwinski, P. Clinical phenotypes and comorbidity in European sleep apnoea patients. PLoS ONE 2016, 11, e0163439.
- Cho, Y.W.; Kim, K.T.; Moon, H.J.; Yang, K.I. Is cormobid insomnia in obstructive sleep apnea linked to heart disease? Sleep Med. 2017, 40 (Suppl. 1), 259.
- Subramanian, S.; Guntupalli, B.; Murugan, T.; Bopparaiu, S.; Chanamolu, S.; Casturi, L.; Surani, S. Gender and ethnic differences in prevalence of self-reported insomnia among patients with obstructive sleep apnea. Sleep Breath. 2011, 15, 711–715.
- Shepertycky, M.R.; Banno, K.; Kryger, M.H. Differences between men and women in the clinical presentation of patients diagnosed with obstructive sleep apnea syndrome. Sleep 2005, 28, 309–314.
- Stelzer, G.; Garcia, E.; Schorr, F.; Barea, L.M.; Barros, H.T. Prevalence of chronic insomnia in patients with obstructive sleep apnea. Braz. J. Psychiatry 2020.
- Hagen, C.; Patel, A.; McCall, W.V. Prevalence of insomnia symptoms in sleep laboratory patients with and without sleep apnea. Psychiatry Res. 2009, 170, 276–277.
- Beneto, A.; Gomez-Siurana, E.; Rubio-Sanchez, P. Comorbidity between sleep apnea and insomnia. Sleep Med. Rev. 2009, 13, 287–293.
- Lichstein, K.L.; Riedel, B.W.; Lester, K.W.; Aguillard, R.N. Occult sleep apnea in a recruited sample of older adults with insomnia. J. Consult. Clin. Psychol. 1999, 67, 405–410.
- McCall, W.V.; Kimball, J.; Boggs, N.; Lasater, B.; D’Agostino, R.B., Jr.; Rosenquist, P.B. Prevalence and prediction of primary sleep disorders in a clinical trial of depressed patients with insomnia. J. Clin. Sleep Med. 2009, 5, 454–458.
- Cronlein, T.; Geisler, P.; Langguth, B.; Eichhammer, P.; Jara, C.; Pieh, C.; Zulley, J.; Hajak, G. Polysomnography reveals unexpectedly high rates of organic sleep disorders in patients with prediagnosed primary insomnia. Sleep Breath. 2012, 16, 1097–1103.
- Gooneratne, N.S.; Gehrman, P.R.; Nkwuo, J.E.; Bellamy, S.L.; Schutte-Rodin, S.; Dinges, D.F.; Pack, A.I. Consequences of comorbid insomnia symptoms and sleep-related breathing disorder in elderly subjects. Arch. Intern. Med. 2006, 166, 1732–1738.
- Bhaskar, S.; Hemavathy, D.; Prasad, S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J. Fam. Med. Prim. Care 2016, 5, 780–784.
- Ong, J.C.; Gress, J.L.; San Pedro-Salcedo, M.G.; Manber, P. Frequency and predictors of obstructive sleep apnea among individuals with major depressive disorder and insomnia. J. Psychosom. Res. 2009, 67, 135–141.
- Kinugawa, K.; Doulazmi, M.; Sebban, C.; Schumm, S.; Mariani, J.; Nguyen-Michel, V.-H. Sleep apnea in elderly adults with chronic insomnia. J. Am. Geriatr. Soc. 2012, 60, 2366–2368.
- Castillo, J.; Goparaju, B.; Bianchi, M.T. Sleep-wake misperception in sleep apnea patients undergoing diagnostic versus titration polysomnography. J. Psychosom. Res. 2014, 76, 361–367.
- Zhang, Y.; Ren, R.; Lei, F.; Xhou, J.; Wing, Y.K.; Sanford, L.D.; Tang, X. Worldwide and regional prevalence rates of co-occurrence of insomnia and insomnia symptoms with obstructive sleep apnea: A systematic review and meta-analysis. Sleep Med. Rev. 2019, 45, 1–17.
