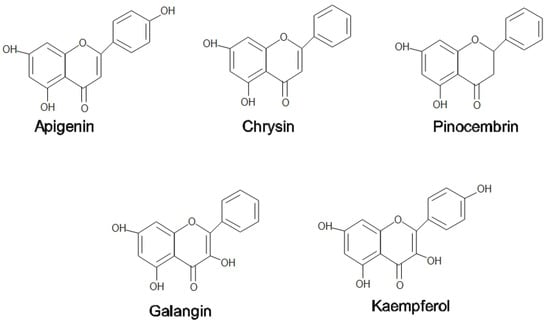
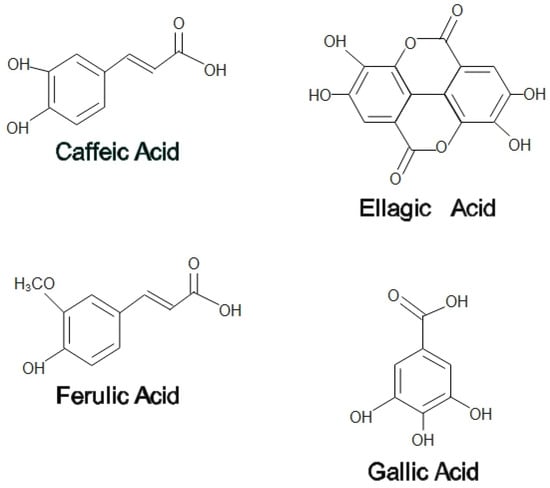
Honey and propolis have recently become the key target of attention for treating certain diseases and promoting overall health and well-being. A high content of flavonoids and phenolic acids found in both honey and propolis contributes to the antioxidant properties to scavenge free radicals. Honey and propolis also exhibited antibacterial effects where they act in two ways, namely the production of hydrogen peroxide (H2O2) and gluconic acids following the enzymatic activities of glucose oxidase, which exerts oxidative damage on the bacteria. Additionally, the anti-inflammatory effects of honey and propolis are mainly by reducing proinflammatory factors such as interleukins and tumor necrosis factor alpha (TNF-α). Their effects on pain were discovered through modulation at a peripheral nociceptive neuron or binding to an opioid receptor in the higher center. The aforementioned properties of honey have been reported to possess potential therapeutic topical application on the exterior parts of the eyes, particularly in treating conjunctivitis, keratitis, blepharitis, and corneal injury. In contrast, most of the medicinal values of propolis are beneficial in the internal ocular area, such as the retina, optic nerve, and uvea.
- honey
- propolis
- natural product
- antioxidants
- anti-inflammatory
- antimicrobial
- ocular disease
1. Introduction
2. Medicinal Properties of Honey
2.1. Antioxidant
2.2. Antibacterial
2.3. Anti-Inflammatory
2.4. Anti-Nociceptive
3. Medicinal Properties of Propolis
3.1. Antioxidants
3.2. Antibacterial
3.3. Anti-Inflammatory
3. Anti-Inflammatory
3.4. Anti-Nociceptive
The analgesic effect of propolis has been studied extensively in several animal models. In a tail flick experiment, a water extract of Anatolian green propolis produced a strong analgesic effect. Supplementation of this propolis to the toothpaste formulations has been shown to have analgesic activity and could be used as a component in treating periodontal disease [115].
4. Medicinal Values of Honey-Related Products on Ocular Diseases
4.1. Conjunctivitis
4.2. Keratitis
In a rabbit model of Pseudomonas-induced keratitis, topical Tualang honey 30% displayed similar results to topical gentamicin and a combination of both in terms of clinical and antimicrobial effects. Clinically, all three treatments (Tualang honey, gentamicin, and mixed of both) improved conjunctival hyperemia though no apparent effects on corneal edema. Slit lamp examination score, a collective score of corneal infiltrates, corneal ulcer, hypopyon, and corneal perforation, were almost similar. Additionally, the Tualang honey and gentami
4.3. Blepharitis
A preclinical study on the cyclodextrin-complexed MGO Manuka honey microemulsion (MHME) has shown to be effective in inhibiting bacterial growth in blepharitis. The in vitro study found that S. aureus and S. epidermidis growth were suppressed at doses of 400 mg/kg and 550 mg/kg of MGO. Subsequent instillation of either diluted MGO MHME or saline control in rabbit eyes revealed the safety and tolerability of the MHME. During this in vivo phase, no significant immediate or cumulative harmful effects were identified upon the evaluation of tear film osmolarity, lipid layer grade, tear evaporation rate, fluorescein staining, phenol red thread, corneal opacity, conjunctival hyperemia and iris appearance grades [144]. Therefore, MHME was further tested on human subjects in the form of eye cream for periocular application for a two-weeks duration. The MHME eye cream caused no significant changes in clinical (visual acuity, eyelid irritation, ocular surface characteristics) and impression cytology evaluation (matrix metalloproteinase-9, IL-6, and MUC5AC) [145], implying the safety and tolerability of MHME eye cream in the clinical study despite transient ocular stinging, which disappeared after water irrigation.
4.4. Corneal Injury
Proliferation is one of the primary steps in wound healing to repopulate the injured area [148]. In a study by Ker-woon et al. (2014), Acacia honey (AH), which is a monofloral honey yielded by Apis mellifera honeybees, has been studied for its proliferative capacity on corneal epithelial cells (CEC). AH enhanced the proliferation of CEC while preserving its normal histological features and cell cycle, accompanied by increased DNA content and cell nuclei [149]. In subsequent in vitro corneal abrasion models, AH accelerated the wound closure, likely attributed to the additional ATP supply of AH. Moreover, AH upregulated both genes and proteins expression of cytokeratin-3, a cluster of differentiation 44 (CD44), and fibronectin [150]. Fibronectin and CD44 expressions were enhanced during the initial and middle phases of the experiment, respectively. This is in accordance with the function of fibronectin in the early phase of wound healing as a temporary extracellular matrix to aid cellular migration [151]. Similarly, CD44 aids the migratory phase by providing adhesive durability for cell-to-cell and cell-to-matrix interactions [150].
4.5. Dry Eye
Optimel Manuka+ Dry Eye drops (Optimel) is an MGH containing a proprietary mix of 16% Leptospermum spp. (manuka) honey and other Australian and New Zealand honey, which have been approved to treat chronic dry eye conditions and blepharitis [162]. A study was carried out to investigate the effects of Optimel eye drop on contact lens-related dry eye by comparing two ways of treatment. One group received the Optimel eye drop for two weeks, followed by another two weeks of conventional lubricant (Systane Ultra), while the other group received the reverse pattern of the treatment. Following Optimel eye drop treatment, dry eye symptoms were significantly alleviated. However, the overall signs of dry eyes seemed to have no significant difference, probably due to the limited time of treatment. However, a majority of the subjects reported good compliance with Optimel eye drop treatment, indicating its safety in reducing dry eye symptoms in contact lens wearers [162].

5. Medicinal Values of Propolis on Ocular Diseases
Propolis is a natural product that has valuable pharmacological and pharmaceutical properties. With more than 300 biologically active components, propolis has thus far been shown to be effective in treating various ocular diseases in animal and in vitro models [16]. Its efficacy in ocular diseases is likely attributable to its antiglaucoma, antiangiogenic, antioxidant, anti-inflammatory, wound healing agent, and neuroprotective properties [16,17,18,170].
This entry is adapted from the peer-reviewed paper 10.3390/ph15111419
