2. Exposure
Humans are constantly exposed to metal ions/salts; allergy to metals is the most prevalent contact allergy in developed societies. More information on the oral, cutaneous, and inhalational bioavailability of metals in humans under different dosing regimens and levels is needed for precise risk assessments. Studies with large numbers of sensitized and non-sensitized individuals, different dosing regimens and dose levels are urgently required.
Cutaneous and inhalation exposure: Metal sensitization may cause dermatological disorders. In the Canary Islands, from 1568 patients that underwent PTs, most contact dermatitis patients were older than 40 years, and the main allergen eliciting positive reactions was Ni (36.5%) [
7]. Similarly, in the group of 546 patch tested patients, the most common metal allergen in Lithuania was Ni, and women were more often sensitized [
8]. In a group of 1919 children, 6% had an allergic reaction to cobalt (Co). ACD triggered by Co should be suspected with dermatitis in a diffused generalized distribution, trunk, or face [
9].
Presumably due to their daily exposure to cosmetic products and jewelry, the urine Ni level was significantly higher in females than males on average. Similar occurrence was found in participants who used penetrating jewelry such as earrings and piercings (regardless of gender), compared to subjects not using such jewelry [
10].
It was found that potassium dichromate, both in petrolatum and aqua can penetrate the skin, which is important for potential human exposure [
11].
Occupational skin diseases appear or exacerbate regarding work and are the second most common type of occupational disease in the world. Nine welding workers had erythematous papules/patches and itching in various areas of the body. The Ni dust was in constant contact with exposed skin, and Ni level exceeded the norm. In two workers, occupational allergic contact dermatitis (OACD) to Ni was confirmed based on a PT [
12]. OACD was most frequent in construction workers (45%), the mainly involved area was hands, and the most frequent allergen was chromium (Cr) in cement [
13]. It was found that precious metal refinery workers are exposed to non-platinum group metals: lead (Pb), Co, Ni, copper (Cu), arsenic (As) and silver (Ag), with exceeded occupational limits of the South African [
14]. The occupational metal ions released at the workplace might entail legal ramifications regarding insurance law.
Oral exposure: Ni-rich food is an excellent source of exposure, mainly breakfast cereals, soy products, chocolate spreads and legumes. It demonstrates an evolution in potential risk to human health to Ni exposure due to the shift towards a more plant-based diet [
15,
16,
17,
18,
19,
20]. Ni-allergic contact mucositis (Ni-ACM) is a disorder where Ni-containing food can impact previously sensitized patients and can be diagnosed by a Ni oral mucosa PT (omPT) [
21]. Celiac disease patients on a gluten-free diet with positive Ni-omPT displayed a recurrence of gastrointestinal and extraintestinal symptoms, although serological and histological remission has been reached. Relief of symptoms appeared after a gluten-free-low-Ni diet [
22]. Irritable bowel syndrome-like disorders are also present in endometriosis. In women with a positive Ni-omTP, a low-Ni diet affected gastrointestinal, extra-intestinal, and gynecological symptoms reduction [
23]. An association has also been found between gastroesophageal reflux disease and a low-Ni diet by improving symptoms [
24]. Ulcerative colitis (UC) patients often had significant Ni or palladium (Pd) hypersensitivities confirmed by a PT. All subjects had metallic dental implants, implying that exposure to Ni is possible involvement in UC pathogenesis [
25].
IgE-mediated reactivity to lipid transfer proteins (LTP) is a group of highly conserved proteins mainly found in fruits. They represent the leading cause of primary food allergy in adults in Mediterranean countries. The prevalence of systemic Ni allergy syndrome (SNAS) in the LTP allergic population is clinically relevant [
26]. SNAS and Ni-ACD are very common among overweight/obese patients. Ni exposure leads to abnormal production/release of growth hormone (GH). In addition, Ni-allergic patients show GH-insulin-like growth factor 1 (IGF1) axis impairment, probably by increasing the inflammation in the pituitary gland [
27].
Releasing metals from items: Exposure to metals and their sensitization potential is extremely difficult to assess. The exact composition of the objects we encounter is often unknown, and the composition is not uniform, making diagnosis difficult, e.g., the impact of Ni in tattoo inks is unclear. A positive PT is not sufficient to verify the reaction following tattooing. Epidemiologic case–control studies with regular biopsies of healthy and inflamed tattoos and PTs would facilitate comprehending the role of Ni in tattoo ink allergies [
28].
Furthermore, the release of metal from objects is not easy to estimate. The gold standard for Ni release assessment is EN1811 test, which has reproducibility limitations [
29]. The proposed alternative dimethylglyoxime (DMG) spot test has high specificity but low sensitivity, which undermines its usability, especially when Ni release is low. It was proven that Cu ions could have a masking effect, resulting in an inaccurate reading of the DMG spot test to Ni [
30]. The Ni release from everyday products is widespread and often above the DMG test limits. It might be potentially dangerous for Ni-sensitive subjects [
31]. Metal parts of laptops and mouses release Ni [
32]. Micro-needling made from stainless steel repeatedly puncturing the skin may release Ni [
33]. Ni and Co is released in allergology-relevant amounts from beauty tools [
34] and metal hairdressers’ tools [
35,
36]. The European Union established a limit of 0.2 μg/cm
2/week Ni release for the items by the Directive in 2004 [
37]. The excessive Ni release from earrings was found in more than 15% of tested earrings [
38,
39], also Cr and Co were released [
40]. Ni release depends on the solution pH; at pH 4, the release is the greatest, which is essential for the stainless-steel crown in dentistry [
41].
Types of metal that can sensitize: Ni is not the only metal that can sensitize, together with Cr and Co are the most common metals that cause allergic reactions. A patient had itchy erythema confined to the bilateral antihelix. A mono-positive PT revealed gold (Au) hypersensitivity, also the headphones he was using contained Au-plated metal parts. After stopping using them, there was no recurrence of symptoms [
42]. Iron (Fe) can be a relevant sensitizer, especially in complicated knee arthroscopy [
43]. Aluminum (Al) salts are adjuvants found in many vaccines. Although rare, patients have reported cutaneous reactions, including ongoing pruritic subcutaneous nodules at the injection site. In most cases, delayed reactions are not contraindications to further vaccine administration. However, it should be evaluated case-by-case basis offering alternative Al-free vaccines [
44,
45]. Allergy from contact exposure to Al, e.g., topical medicaments and deodorants might be more common than thought (7 case reports) [
46,
47]. Sunscreens containing Al might lead to ACD in pediatric patients [
48]. Unfortunately, Al-PT is only positive when there is a strong Al-allergy [
49].
3. Diagnostics
Patch tests (PTs): PTs are the gold standard for the diagnosis of allergic hypersensitivity [
50]. It is known that PT readings on day seven (D7) may show additional positive reactions. Metal allergens and older age were predictive for late positive reactions. Within the tested allergens, without D7 readings, on average, 12% of sensitizations would have been missed [
51,
52]. Long-lasting allergic PT reactions (LLAPTR) are positive PT reactions lasting more than two weeks. A 90-year-old dental patient had a positive PT on D2 and D4 for platinum (Pt), Pd, and indium (In), but for Au the test was negative until D45 [
53].
Ideally, the PTs should be performed while the patient is not taking biologics. Unfortunately, this is not always possible, so clinicians need to assess the risks and benefits of testing during therapy [
54]. The precision of PTs after dupilumab is under consideration. Reactions may stay positive (with no dampening effect), change to negative (false-negative reactions), or become newly positive after its administration, indicating that patient-specific factors should be taken into consideration [
55,
56,
57]. Secukinumab (anti-IL-17 mAb) showed no significant reduction in Ni-PT in patients with ACD (with confirmed Ni allergy before) [
58].
When hypersensitivity to metal implant is suspected, the PT should be done for confirmation. Additionally, the identification of implant compositions should be accomplished before potential removal. The patient underwent a skin grafting that was covered with a tattoo. An allergic reaction to anchors or tattoo inks was suspected. The DMG spot test result was negative for metal devices. Finally, an inductively coupled plasma-mass spectrometry analysis revealed the release of Ni from the anchor [
59].
Ag is widely used topically because of its anti-microbial properties. It should be considered to include Ag as an extension of PTs of dermatitis in subjects with skin ulcers since it is not present in some of the commercial series. Hereby, a greater number of cases of ACD to Ag could be identified earlier [
60].
Ni allergen is present in different PT lines, e.g., ICDRG baseline, European or Swedish baseline, but it occurs as Ni sulfate 200 μg/cm
2 in TRUE Test, or Ni sulfate 2.5% petrolatum (pet.) and 5% pet. The reactions vary, and most positive reactions were found in 5% pet., TRUE Test and 2.5% pet. shown similar responses [
61].
In vitro tests: The in vitro lymphocyte proliferation test (LPT) can be an additional method in case the skin is not the primary organ of exposure. The classical LPT uses tritiated thymidine, so a radioactive-free LPT test with carboxyfluorescein succinimidyl ester (CFSE) was proposed, which furthermore can distinguish T cell subsets and assess the released cytokines [
62,
63]. However, the read-out method can affect the sensitivity of the LPT; it was confirmed that ELISA or flow cytometry provides the best detection of sensitization in the context of allergies [
64]. In the culture of PBMC performed by LPT, the metal-reactive (Cr, Ni, and Co) T helper lymphocytes (Th cells) with high CD45RO expression and co-expression of cutaneous lymphocyte-associated antigen (CLA) and C-C Motif Chemokine Receptor 6 (CCR6) were identified. Th cells identified individuals with a positive Ni-PT with 100% sensitivity and 92% specificity [
65].
Other tests: Urine Ni concentration is an effective predictor of Ni exposure but not of an allergy. The urine Ni concentrations were not statistically different in allergic patients with Ni-positive PT compared to negative controls. However, the urine level of Ni correlated with lifestyle [
10].
4. Mechanisms and Biomarkers
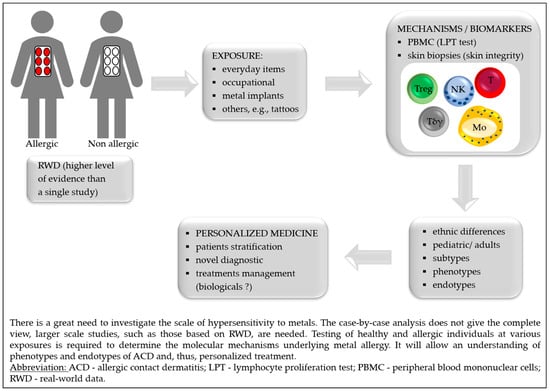
The discovery of the molecular mechanisms by which contact allergens cause skin sensitization has a potential implication for treatment decisions. The biomarkers might facilitate the diagnosis of metal hypersensitivities and enable patient stratification for potential treatment strategies [
66]. Key advances in the understanding of metal allergy mechanisms and biomarkers are presented in
Table 1.
Table 1. Key advances in metal allergy mechanisms and biomarkers.
|
Outcomes
|
Exposition to Metal
|
Ref.
|
|
↑ metal-specific CD154+ CD4+ Tmem
(overexpression of TRAV9-2 and CDR3 histidine)
|
Allergic and non-allergic subjects stimulated with Ni,
Co or Pd (PBMC)
|
[67,68]
|
|
↑ IL-5
|
Ni-allergic patients (PBMC)
|
[69]
|
|
Ni-allergy patients, differentiation between independent Ni or cross-reactivity of Ni/Pd allergy (PBMC)
|
[71]
|
|
Cross reactivity between Ni/Cr and Pd
|
Sensitization with Ni or Cr, challenge with Pd
(mice model)
|
[70]
|
|
Skin barrier defects: ↓ terminal differentiation—FLG, FLG2, LOR, LCEs, tight junction—CLDN1/CLDN8, lipid metabolism—FA2H, FABP7
|
Biopsies from healthy subjects after Ni-topical application
|
[73]
|
|
Cellular infiltrates: ↑ CD3+ T,
CD11c+ myeloid DC, DC-LAMP+ mature DC,
MBP+ eosinophils, FOXP3+ Treg
|
|
↑ M1, mast cells, neutrophils, NK,
CD4+ Tmem, CD8+ T
|
Biopsies from Ni-allergic patients
|
[74]
|
|
↓ M2, resting mast cells, Tγδ, Treg
|
|
↓ SBSN
|
Ni-allergic patients (serum)
|
[75]
|
|
↑ Sema3A (activates MAPK and TNF-α)
|
Ni-induced allergy (mouse ear tissue)
|
[76]
|
|
↑ TSLP in keratinocytes
and TNF-α in epithelium
|
OLPs metal-allergy patients
|
[77]
|
|
↑ IL-6, CXCL8, CCL2, CCL5, and CCL20
|
RHS exposure to Ni and Streptococcus mitis exposure
|
[78]
|
|
Lipid profile: ↑ cholesterol, DAG, MAG
|
Non-allergic skin exposed to Co
|
[79]
|
|
Lipid profile: ↑ DAG
|
Non-allergic skin exposed to Cr
|
|
Lipid profile: ↓ DAG and MAG
|
Non-allergic skin exposed to Ni
|
|
LC emigration of the epidermis
(in an IL-10 but not IL-1B dependent way)
|
RHS exposure to Ti
|
[80]
|
Abbreviations: ↑ = increase; ↓ = decrease; + = positive; CCL = C-C motif ligand; CD = cluster of differentiation; CDR3 = complementarity determining region 3; CLDN = claudin; Co = cobalt; Cr = chromium; CXCL = C-X-C motif chemokine ligand; DC = dendritic cell; FA2H = fatty acid 2-hydroxylase; FABP7 = fatty acid binding protein 7, brain; FLG = filaggrin; FOXP3 = forkhead box P3; IL = interleukin; LAMP = lysosomal associated membrane glycoprotein; LCEs = late cornified envelope proteins; LOR = loricrin; M1/M2 = proinflammatory/anti-inflammatory macrophages; MAG/DAG = mono/diacylglycerols; MAPK = mitogen-activated protein kinases; MBP = myelin basic protein; Ni = nickel; NK = natural killer cells; OLP = oral lichen planus; PBMC = peripheral blood mononuclear cells; Pd = palladium; RHS = reconstructed human skin; SBNS = suprabasin; Sema3A = semaphorin; Tmem = memory lymphocytes T; TNF-α = tumor necrosis factor-alpha; TRAV9-2 = α-chain V-segment; TSLP = thymic stromal lymphopoietin; Tγδ = T gamma-delta cells.
5. Implants
Metal sensitivity may be a rare cause of prosthetic joint failure or loosening. An implant allergy is diagnosed by a PT, and implant removal is crucial to both diagnosis confirmation and treatment. The revisions are not such a problem because hypoallergenic implants may relieve symptoms. In 2013, an outline was presented for diagnosing metal hypersensitivity caused by an implant: confirmation of eruption overlying the implant (chronic dermatitis can begin weeks to months after implant use), diagnosis by positive PT, and symptoms resolution after the implant removal [
84]. However, to date, there are no guidelines in this regard. The latest evidence suggests that there is a link between (implants) metal, in particular Ni allergy, and autoimmunity that may lead to similar clinical outcomes. An explanation of their potential mechanisms will support a more successful and safer treatment [
85]. Advances on hypersensitivity to medical implants, including unusual symptoms are presented in
Table 2.
Table 2. Advances on hypersensitivity to medical implants, including unusual symptoms.
|
Metal that Caused Hypersensitivity/Implant Type
|
Symptoms
|
Ref.
|
|
Multiple metals/orthopedic implants: hip, knee shoulder joint
|
Different; the most common—delayed wound healing
and/or recurrent wound issues after the implantation,
joint failure or loosening
|
[86,92,93,98,106]
|
|
Ni/endovascular implants (stents)
|
In-stent restenosis or prominent eczematous reaction overlying
the endovascular implant, eosinophilia
|
[102,107]
|
|
Co, Ni/drug-eluting stents
|
Pruritic rash with hypereosinophilia
|
[108]
|
|
Au and Pd/dental implant
|
Oral lichenoid contact lesion (OLCLs)
|
[103]
|
|
Ti/dental implants
|
Rash, urticaria, pruritus, redness, dermatitis and facial eczema, pain, hyperaemia of soft tissues, swelling in submental and labial sulcus, gingival hyperplasia acne-like facial inflammation
|
[105]
|
|
Ni/metal anchors
|
Erythematous and vesicular lesions around the grafted tattoo skin, but the tattoo was not affected (placed with clips or anchors)
|
[59]
|
|
Ni/stainless-steel skull pins
|
Erythema on sites of the head where the skull pins inserted
|
[109]
|
|
Ti/cervical implant
|
Persistent refractory neck pain; subsequently, after eight years,
a planter rush
|
[110]
|
|
Ti/metal clips for cholecystectomy
|
Right upper quadrant pain, diarrhea, and nausea
|
[111]
|
|
Low-grade fever, nausea, vomiting, joint pain,
bloody diarrhea
|
[112]
|
|
Co, Ni, Hg/metal clips for cholecystectomy
|
Myalgia, joint pain and tenderness, mental fogginess, mild forgetfulness, irritable bowel syndrome, stomach cramps,
dry skin and hair, hair loss
|
[113]
|
|
Cu/intrauterine device
|
Cutaneous eruption
|
[114]
|
|
Multiple-metals/dental implant
|
Palmoplantar pustulosis (PPP) and periodontitis
|
[104,115]
|
|
Au/dental implants
|
Oral lesions with characteristic Wickham’s striae
|
[116]
|
|
Ti/temporary tissue expander
|
Well-demarcated, erythematous plaque over the left breast reconstructive breast surgery
|
[117]
|
Abbreviations: Au = gold; Co = cobalt; Cu = copper, Hg = mercury; Ni = nickel; Pd = palladium; Ti = titanium.