The annual incidence of pancreatic cancer has increased worldwide, with 495,773 new cases reported in 2020 [
1]. Pancreatic cancer is projected to be the second leading cause of cancer-related death for both men and women in the United States by 2030 [
2]. Pancreatic ductal adenocarcinoma (PDAC), the most common type of pancreatic cancer, has the most dismal prognosis among all solid tumors, with a 5-year survival rate of approximately 10% [
3,
4]. Due to its aggressive biology, lack of distinctive clinical symptoms, and lack of reliable biomarkers for early detection and diagnosis, most patients with PDAC present with locally advanced or metastatic disease, which is not suitable for a potentially curative surgical resection [
5]. In addition, PDAC is resistant to conventional treatment modalities, including chemotherapy and radiotherapy, and it has limited response to the modern targeted therapies and immunotherapies; therefore, the prognosis and survival for patients with PDAC have not significantly changed over the years [
6]. The histological subtypes and precursors of PDACs are associated with distinctive genetic alterations, histomorphological features, and different prognoses [
7]. The lack of effective treatment and grim prognosis results from our poor understanding of the complicated and multifactorial nature of PDAC biology, the immunosuppressive tumor microenvironment (TME), and the molecular genetic heterogeneity among primary tumor cells and among metastasis-initiating cells [
8]. In recent years, significant progress has been made in profiling the molecular alterations and classification of PDAC, but these findings are yet to be translated into early diagnosis and effective therapy. Therefore, a better understanding of the histological, genetic and molecular heterogeneities; the aggressive biology and the immunosuppressive TME; and the development of predictive and prognostic markers are important in the development of effective personalized therapies.
2. Histology and Morphologic Heterogeneity of PDAC
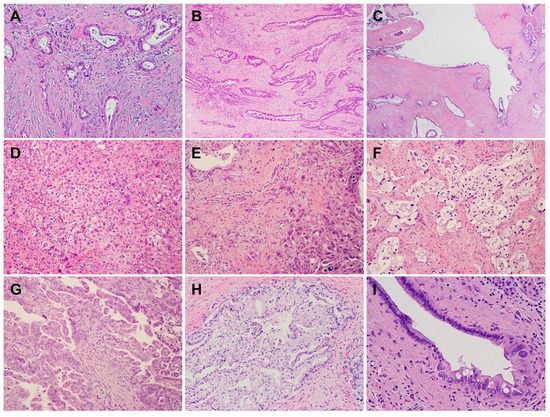
PDACs are a heterogeneous group of malignant pancreatic epithelial neoplasms. Conventional PDACs are characterized by dense desmoplastic stroma intermixed with angulated glands, small nests of malignant epithelial cells and/or single tumor cells (
Figure 1A). PDACs often show a spectrum of differentiation ranging from well-differentiated to poorly differentiated adenocarcinomas within the same tumor and show significant inter- and intra-tumoral heterogeneity in histomorphological patterns, such as complex interconnecting tumoral glands embedded in desmoplastic stroma (
Figure 1B), a large duct type (
Figure 1C), poorly differentiated carcinoma with eosinophilic or clear cells (
Figure 1D–F), complex intraluminal micropapillae formation (
Figure 1G), cribriform histology with foamy cells (
Figure 1H), and the pagetoid involvement of pancreatic duct/intraductal carcinoma (
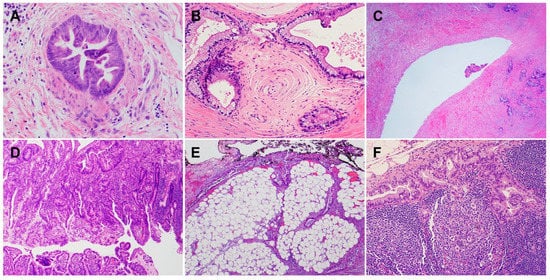
Figure 1I). Aggressive histological features, such as lymphovascular invasion, tumor invasion into peripancreatic soft tissue, large vessels and adjacent organ(s)/structure(s), perineural invasion, the involvement of resection margins, and lymph node metastasis, are frequently present in resected PDAC specimens (
Figure 2A–F). The presence of these aggressive histological features is associated with an increased risk of post-operative tumor recurrence/distant metastasis and poor survival in PDAC patients [
9,
10,
11,
12].
Figure 1. Pancreatic ductal adenocarcinomas (PDACs) with various histomorphological patterns (hematoxylin and eosin stain). (A) Moderately differentiated PDAC with extensive desmoplastic stroma; (B) moderately differentiated PDAC with interconnecting complex glands embedded in desmoplastic stroma; (C) large duct variant of PDAC; (D) poorly differentiated PDAC; (E) poorly differentiated PDAC intermixed with moderately differentiated areas; (F) clear cell variant of PDAC; (G) moderately differentiated PDAC showing extensive, complex intra-luminal micropapillary formation; (H) cribriform histology with foamy cells; (I) pagetoid involvement of pancreatic duct by PDAC (intra-ductal carcinoma).
Figure 2. The common histological features associated with aggressive clinical outcomes for pancreatic cancer patients (hematoxylin and eosin stain). (A) Tumor invasion into muscular vessels; (B) perineural invasion; (C) tumor invasion into the wall of superior mesenteric vein; (D) PDAC invasion through the muscularis propria of the duodenum and involves the mucosal surface; (E) PDAC invades into the peripancreatic and retroperitoneal soft tissue and involves the uncinate margin (marked by black ink); (F) metastatic PDAC in a regional lymph node.
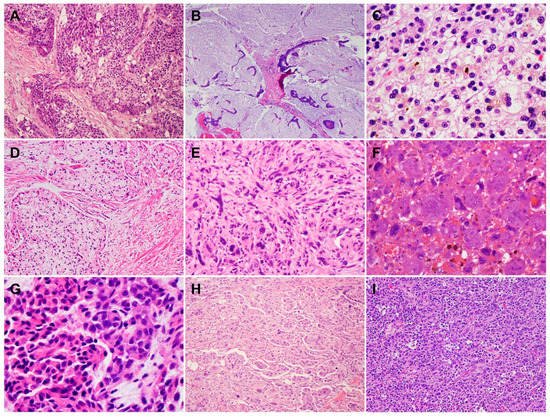
In addition to conventional PDAC, there are nine histological subtypes of PDAC according to the World Health Organization (WHO) classification, which further highlight the morphologic heterogeneity of PDAC [
13]. The subtypes of PDAC are adenosquamous carcinoma (ASC)/squamous cell carcinoma (SCC), colloid carcinoma, hepatoid carcinoma, signet ring cell (poorly cohesive cell) carcinoma, undifferentiated carcinoma, undifferentiated carcinoma with osteoclast-like giant cells, medullary carcinoma, micropapillary carcinoma, and undifferentiated carcinoma with rhabdoid cells (rhabdoid carcinoma) (
Figure 3A–I). While some PDAC subtypes share a similar molecular pathogenesis, biological and clinical behavior, and prognosis to conventional PDAC, these subtypes are characterized by specific histomorphological and clinical features, and some have a different molecular profile, genetic alterations, and prognosis. For example, colloid carcinoma typically arises in association with an intestinal type of intraductal papillary mucinous neoplasm (IPMN) and has a better prognosis than conventional PDAC [
14,
15,
16,
17]. On the other hand, ASC and undifferentiated carcinomas have worse prognoses than conventional PDAC [
13,
15,
18]. Medullary carcinoma is more frequently associated with a high level of microsatellite instability, which may predict better responses to immunotherapy [
19,
20], and often with the wild-type
KRAS gene [
21,
22,
23].
Figure 3. Histological subtypes of pancreatic ductal adenocarcinoma (hematoxylin and eosin stain): (A) Adenosquamous carcinoma; (B) colloid carcinoma; (C) hepatoid carcinoma with bile lakes; (D) signet-ring cell carcinoma; (E) undifferentiated carcinoma; (F) undifferentiated carcinoma with osteoclast-like giant cells; (G) undifferentiated carcinoma with rhabdoid cells (rhabdoid carcinoma); (H) micropapillary carcinoma; (I) medullary carcinoma.
3. Genetic Alterations and Molecular Subtypes of PDAC
PDAC is characterized by a handful of inherited (germline) and recurring somatic mutations. The first whole exome sequencing of human PDAC samples was reported in 2008 by Jones et al. [
24]. In that study, 20,661 protein-coding genes in 24 PDAC samples were sequenced, and more than 1500 somatic mutations in 1007 genes were identified. This study was followed by several landmark, large-scale whole exome sequencing and comprehensive molecular profiling of human PDAC samples, which provided us with the in-depth understanding of the heterogeneous molecular landscapes of PDAC [
25,
26,
27]. These studies identified four “mountains” (the genes mutated at the greatest frequency): oncogenic mutations of
Kirsten rat sarcoma (KRAS), loss-of-function mutations and/or deletions of the
TP53 tumor suppressor genes,
mothers against decapentaplegic homolog 4 (SMAD4), and
the cyclin dependent kinase inhibitor 2A (CDKN2A) [
24]. The data from genetically engineered mouse models have shown that these mutations play an essential role in the development and/or progression of PDAC [
24,
28,
29]. In addition to the four “mountains”, a large number of less common “hills” (genes mutated at low frequencies) have been detected in PDACs. For example, amplifications of other less frequent oncogenes such as
CMYC (on chromosome 8q),
MYB (chromosome 6q),
AIB1/NCOA3 (chromosome 20q),
EGFR (chromosome 7p), and
GATA6, as well as recurrent chromosomal amplifications, have also been identified [
7]. One or more somatic/germline mutations of the genes involved in DNA damage repair (DDR), such as
BRCA2, BRCA1,
PALB2,
ATM,
CHEK2,
RAD51C, and
RAD51D mutations, may be detected in 10–20% of PDAC patients [
30,
31,
32,
33]. These less common genetic alterations may represent valuable targets or serve as predictive biomarkers for PDAC patients. For example, defects in DDR pathway in PDACs represent a unique subset of patients who may benefit from platinum-based chemotherapy (e.g., cisplatin) or the newly approved poly (ADP-ribose) polymerase (PARP) inhibitors such as olaparib [
34,
35].
Multiple studies have reported on the molecular subtypes of PDAC based on the whole exome sequencing data and/or integrated analyses of the genomic, transcriptomic, proteomic, and epigenetic profiles of human PDAC samples [
36,
37,
38,
39]. Collisson et al. reported three molecular subtypes of PDAC: the classical, quasi-mesenchymal (QM), and exocrine-like based on the analysis of 27 microdissected PDAC samples [
38]. The classical subtype showed a higher expression of adhesion-associated and epithelial genes and a higher expression of
KRAS and
GATA6, an essential gene for pancreatic development and PDAC progression, compared with the QM subtype. The QM subtype was found to have a high expression of mesenchyme-associated genes. The exocrine-like subtype showed the relatively high expression of tumor cell-derived digestive enzyme genes. These molecular subtypes were found to be significantly correlated with patient survival in that the QM subtype had the worst survival. They also demonstrated that PDAC cell lines of the QM subtype were more sensitive to gemcitabine, whereas the classical subtype cell lines were more sensitive to erlotinib (an
EGFR antagonist) [
38]. Using non-negative matrix factorization to digitally dissect the tumor and stromal gene signature of primary and metastatic PDAC, Moffitt et al. identified two tumor-specific subtypes: the basal-like subtype, which is molecularly similar to the basal-like carcinoma of breast and bladder, and the classical subtype, and two stromal subtypes: normal and activated. The basal-like subtype had a worse prognosis but a superior response to adjuvant therapy compared with the classical subtype [
39]. Via RNA sequencing, they showed that the
KRASG12D mutation was significantly overrepresented in the basal-like subtype,
KRASG12V was isolated to the classical subtype, and
SMAD4 expression was significantly higher in the classical subtype compared with the basal-like subtype, which is consistent with the observation that SMAD4 loss confers a more aggressive tumor behavior [
39]. The normal stroma showed the relatively high expression of known markers for pancreatic stellate cells (desmin, smooth muscle actin, and vimentin), whereas the activated stroma was characterized by a gene set associated with macrophages (integrin
ITGAM and the chemokine ligands
CCL13 and
CCL18) and other genes that are reported to promote tumor progression (
SPARC,
WNT2,
WNT5A,
MMP9, and
MMP11) [
39,
40]. Patients with the classical subtype and activated stroma had worse survival compared with those with the classical subtype and normal stroma. Stromal subtypes were not associated with survival in patients with basal-like subtype PDAC [
39]. Moffitt’s classification of PDACs into basal-like and classical subtypes was validated by Puleo et al., who classified PDACs into five subtypes: pure basal-like, stroma-activated, desmoplastic, pure classical, and immune classical based on features of cancer cells and the tumor microenvironment [
41]. Thus, targeting the tumor-promoting genes in activated stroma may represent a potential strategy for PDAC patients.
The integrated genomic analysis of 456 PDAC samples by Bailey et al. identified 32 recurrent mutated genes in 10 pathways—
KRAS,
TGF-β,
WNT,
NOTCH,
ROBO/SLIT signaling,
G1/S transition,
SWI-SNF, chromatin modification, DNA repair, and RNA processing—and four molecular subtypes of PDACs—pancreatic progenitor, squamous, aberrantly differentiated endocrine exocrine (ADEX), and immunogenic [
36]. The pancreatic progenitor subtype (19%) was characterized by the transcriptional factors involved in early pancreatic development (
PDX1,
MNX1,
HNF1A,
HNF1B,
HNF4A,
HNF4G,
FOXA2,
FOXA3, and
HES1) and metabolic pathways such as fatty acid oxidation and drug metabolism [
42]. The squamous subtype (31%) was enriched with
TP53 and
KDM6A mutations, as well as the hypermethylation of genes governing pancreatic endodermal cell-fate determination (e.g.,
PDX1,
MNX1,
GATA6, and
HNF1B). The ADEX subtype (21%) showed the upregulation of genes that regulate networks involved in
KRAS activation. This subtype included two gene programs, with one focused on exocrine function (
NR5A2,
MIST1 and
RBPJL) and the other related to endocrine differentiation (
NEUROD1,
MODY,
INS and
NKX2–2). The immunogenic subtype (29%) contained a family of genes related to immune cell function including B cell signaling, Toll-like receptor signaling, antigen presentation, and the infiltration of CD8+ and CD4+ T cells, with the upregulation of the immune inhibitor PD-1 and cytotoxic T-lymphocyte-associated protein-4 (CTLA-4) [
36,
42]. These molecular subtypes correlated with histopathological features in that the squamous subtype represented ASC, progenitor and immunogenic represented colloid carcinomas and carcinomas arising from IPMN, and ADEX represented rare acinar cell carcinomas [
36]. Among these molecular subtypes, the squamous subtype had the worst survival, while the other three subtypes showed similar survival rates [
36]. Another integrated analysis of the mRNA, miRNA, lncRNA and DNA methylation profiling of 150 PDAC samples by the Cancer Genome Atlas Research Network identified two subtypes of PDACs: SNF-1 and SNF-2. The SNF-1 subtype represented most of the basal-like subtype in Moffitt’s classification, the squamous subtype in Bailey’s classification, and the QM subtype in Collison’s classification [
37].
More recently, Chan-Seng-Yue et al. performed whole genome and transcriptome analysis of purified tumor cells from 314 primary and metastatic PDAC patients to generate tumor-specific expression signatures [
43]. They classified PDACs into five molecular subtypes: basal-like A and B for the previously defined basal-like subtype, hybrid, and classical A and B for the previously defined previously defined classical subtype. The hybrid subtype was inconsistently classified by previous classification systems due to the presence of multiple expression signatures. Patients with basal-like A PDAC often present with advanced disease and show the worst response to gemcitabine-based chemotherapies and FOLFIRINOX. In contrast, patients with basal-like B and hybrid tumors often present with resectable disease. Therefore, the ability to distinguish the basal-like A, basal-like B, and hybrid subtypes from the group formerly classified as basal-like allows for the more accurate prediction of chemotherapy response. Classical A/B tumors were found to be associated with an increased frequency of
GATA6 amplification and complete SMAD4 loss, whereas basal-like A/B tumors showed the complete loss of
CDKN2A and a higher frequency of
TP53 mutations. At single-cell resolution, the authors also showed that basal-like and classical subtypes can co-exist in the same tumor, which highlighted the intra-tumoral molecular heterogeneity [
43].
The most recent molecular subclassification of PDACs was reported by Hwang et al. in 2022. Using the single-nucleus RNA sequencing and whole digital spatial transcriptome profiling of 43 primary PDAC samples (18 untreated and 25 treated), they identified three distinct subtypes: classical, squamoid–basaloid, and treatment-enriched. Their study uncovered that the neural-like progenitor (NRP) malignant cell program was enriched in residual carcinoma after chemoradiation therapy. The NRP cells were associated with treatment resistance and poor survival in PDAC patients via the regulation of genes involved in drug efflux, the negative regulation of cell death, and resistance to chemotherapy (e.g.,
ABCB1,
BCL2,
PDGFD and
SPP1), tumor–nerve crosstalk (e.g.,
SEMA3E,
RELN and
SEMA5A), and metastasis (
NFIB) [
44].
These molecular classifications of PDAC provide rich and comprehensive datasets to better understand pancreatic tumorigenesis, genetic/molecular landscapes, intra- and inter-tumoral heterogeneity, tumor progression, and drug resistance. More importantly, the molecular subtyping of PDAC may provide useful information for more effective subtype-tailored therapies for PDAC patients. However, due to their complexity, these classifications of PDAC have not been utilized in daily pathologic diagnosis or clinical practice.
4. Heterogeneous Response of PDAC to Neoadjuvant Therapy
Neoadjuvant therapy is routinely used to treat PDAC patients with borderline resectable and high-risk resectable disease, as well as selected patients with locally advanced disease [
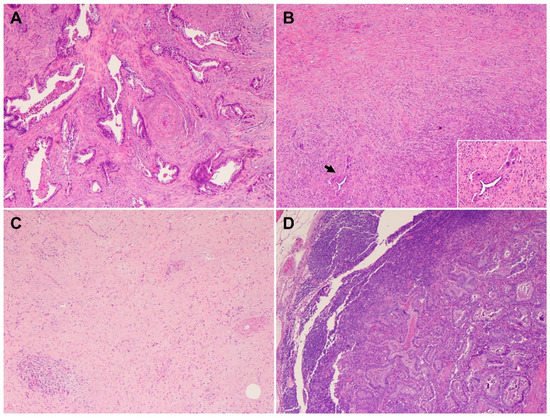
45]. Pathologic studies of the post-therapy pancreatectomy specimens have shown that only 12.6% to 18.6% PDAC patients demonstrate a complete or near complete pathologic response to neoadjuvant therapy, which is associated with better survival, while the majority of PDAC patients (>80%) demonstrate a moderate or minimal response to neoadjuvant therapy and poor survival [
46,
47,
48,
49]. These data highlight not only the fact that vast majority of PDACs are resistant to neoadjuvant chemotherapy with or without radiation but also the inter-tumoral heterogeneity in tumor response among PDAC patients. It is also not uncommon to observe significant intra-tumoral, heterogeneous response to neoadjuvant therapy in different areas of the same treated tumor, with some areas of the tumor showing complete or near complete response and other areas showing minimal or no response (
Figure 4A,B). Occasionally, differential responses to neoadjuvant therapy are also observed between the primary PDAC and the metastatic carcinoma in lymph node(s) in the same patient (
Figure 4C,D). Currently, there are limited data on the molecular correlation with tumor response to neoadjuvant therapies. The molecular mechanisms underlying the inter- and intra-tumoral heterogeneity in response to neoadjuvant therapy is not clear. It is possible that the cellular and molecular/genetic heterogeneity and the heterogeneity in the TME contribute to the heterogeneous response in PDAC patients. The recent molecular profiling of treated PDACs suggested that the NRP malignant program was enriched in residual carcinoma after chemoradiation therapy and plays a role in tumor resistance to therapy [
44]. Future biomarker-driven clinical trials of neoadjuvant therapy are needed to address this important question.
Figure 4. Heterogeneous response of PDAC to neoadjuvant therapy (hematoxylin and eosin stain). (A,B) Representative micrographs showing a PDAC with an area of minimal response (A) and near complete response in other areas (B); (C,D) representative micrographs showing a PDAC with complete response in primary tumor (C) but minimal response in the metastatic PDAC in the regional lymph node (D).