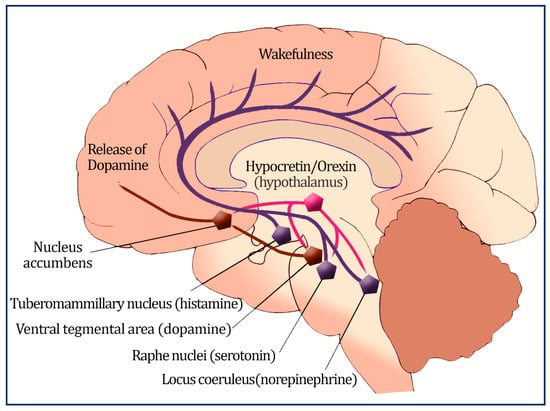
The ventral tegmental region connects orexin neurons to the reward system, as well (nucleus accumbens, containing dopamine).
2. Prevalence of Obesity in Patients with Narcolepsy
Numerous studies have evaluated the frequency of overweight and obesity in people with narcolepsy [
17], and the literature generally confirms that body mass index (BMI) is higher in people with narcolepsy than in controls (
Table 1). Waist circumference was also higher among patients with narcolepsy than among controls [
18].
A study by Poli et al. reported a higher prevalence of overweight (BMI between 85th and 97th percentile) and obesity (BMI > 97th percentile) in 43 children and adolescents diagnosed with NT1, compared with the general pediatric population (78% vs. 36%, respectively) [
17]. Furthermore, 60% of patients were reported to gain weight around narcolepsy onset [
17]. This finding concurs with Wang et al., who reported that in 65 Chinese children with NT1 for less than a year, BMI increased considerably at six, twelve, eighteen, twenty-four, and thirty months of follow-up but not at month thirty-six [
23]. In addition, Poli et al. demonstrated that high BMI was predicted by being diagnosed at a younger age, having a shorter disease duration, and lower high-density lipoprotein (HDL) levels [
17]. Notably, a high prevalence of precocious puberty was reported in 17% of patients compared with obese controls [
17]. Another important study supports the hypothesis of weight gain around narcolepsy onset in children recently diagnosed with NT1 [
30]. A retrospective review of 30 patient records over two years before narcolepsy onset, found that overweight and obesity increased from 17% to 50% at the time of diagnosis [
30]. Another recent study assessed children’s rapid weight gain (RWG) phenotype associated with narcolepsy onset [
31]. The RWG narcolepsy group was younger, sleepier, and more likely to be obese at narcolepsy diagnosis than at the beginning of symptoms, which suggests a faster-moving pathological process. The RWG group still had a higher BMI z-score and a higher prevalence of obesity compared to the non-RWG group at the most recent follow-up [
31].
Additionally, a reported defect in histamine neurotransmission (another wake-promoting neurotransmitter) has only been observed in the Cerebrospinal fluid (CSF) of NT1pediatric patients [
32], not adult patients [
33]. Since moderate obesity has been shown in knock-out mice lacking either histamine or orexin, histaminergic neurons may also be involved in the rapid weight gain process [
34,
35]. This may explain the higher reported incidence of weight gain in children with narcolepsy; however, more studies are needed to confirm the role of histamine in weight gain in humans with narcolepsy.
In addition, overweight/obese patients were found to have lower levels of HDL, higher systolic and diastolic blood pressure, and a higher prevalence of metabolic syndrome, which was diagnosed in 18.8% of cases, compared to a cohort of with normal BMI [
30].
Case-control studies also reported a higher prevalence of overweight and obesity among adult patients with narcolepsy [
36]. Schuld et al. compared patients with narcolepsy with a community-based sample and reported that the distribution of BMI in the patient sample did not substantially differ from patients who had previously received pharmacological therapy for narcolepsy and drug-naive patients [
36]. Moreover, no differences were detected between healthy individuals who were HLA-DR2 positive and negative [
36]. The authors concluded that an elevated BMI in patients with narcolepsy could be related to neuroendocrine abnormalities related to the condition rather than to HLA-DR2 antigen or narcolepsy medications [
36], as the prepro-orexin gene is downregulated in mice with hereditary obesity due to multiple leptin system abnormalities, suggesting that orexins play a role in endocrine systems [
37].
In adults, longitudinal data suggest that patients with narcolepsy may continue to gain weight over time. Our team followed 32 NT1 patients for 10 years and reported an increase in BMI from baseline of 30 ± 5.1 to 33.3 ± 6 kg/m
2 (
p = 0.001) [
38]. These results concur with a report from South Korea, after 10 years of follow-up of nine NT1 patients and nine sex and age-matched NT2 patients; BMI increased from 26.8 ± 0.9 kg/m
2 to 29.23 ± 0.91 kg/m
2 (
p = 0.001) [
39]. These results suggested that BMI may continue to increase in patients with narcolepsy over the years.
Compared to patients with idiopathic hypersomnia (IH), a small study demonstrated that patients with narcolepsy with low orexin had significantly higher BMI, greater waist-to-hip ratio and waist circumference, lower levels of HDL, higher total cholesterol and triglycerides, higher diastolic blood pressure, higher fasting insulin, and a higher glucose/insulin ratio (suggesting insulin resistance) [
27]. Interestingly, after adjusting for BMI, patients with narcolepsy remained significantly higher in waist circumference, lower in HDL, and higher in glucose/insulin ratio compared with controls [
27].
Changes in patients with narcolepsy seem to be related not only to BMI but also to fat distribution. A magnetic resonance imaging (MRI) study of 19 adolescents diagnosed with NT1, demonstrated that patients with narcolepsy had higher total abdominal adipose tissue, higher visceral adipose tissue (VAT), and higher abdominal subcutaneous adipose tissue than healthy controls of matched age and sex [
22]. On the other hand, another study reported no difference between 14 patients with narcolepsy and 14 age-sex-BMI-matched controls in terms of body fat percentage, fat mass, fat mass index, fat-free mass, fat-free mass index, and total body water [
40]. However, less muscle mass was found in patients with narcolepsy compared with controls [
40].
Putting it all together, overweight and obesity are prevalent and well-documented in patients with narcolepsy across different ages. Based on the currently available evidence, it seems that the early onset of narcolepsy is associated with an increase in BMI [
17,
30]. The coincidence of narcolepsy onset and orexin deficiency in children and adolescents may produce amplified weight gain, possibly due to the reduced activities associated with sleepiness and reduced metabolic rate [
23]. Nevertheless, weight gain has been reported in adult patients with narcolepsy too. Therefore, closely monitoring overweight and obesity, and applying appropriate weight reduction strategies are crucially important. Moreover, generating a specific guideline for patient follow-ups, including the assessment of related laboratory investigations (such as lipid and glucose panels) at certain time intervals, may significantly impact decreasing obesity-related cardiometabolic risks and improve patients’ quality of life. Additionally, studies are needed to characterize patients with narcolepsy who are more vulnerable to developing obesity and the time period of the illness that carries the higher risk of gaining weight.
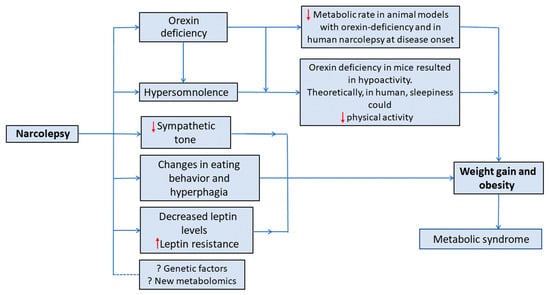
4. Proposed Theories of Weight Gain in Narcolepsy
The mechanism behind weight gain in narcolepsy is not fully understood. In fact, obesity in patients with narcolepsy may be caused by a variety of causes, such as: less physical activity [
41], binge eating behavior [
42], low metabolic rate [
23,
42], reduced sympathetic tones [
43], growth hormone deficiency [
44], and reduced plasma leptin level [
45]. Nevertheless, no consistent answer has been concluded, as investigating these possible contributing factors has shown conflicting results.
Figure 2 presents a summary of the proposed mechanisms for increased weight in patients with narcolepsy.
4.1. Orexin’s Role in Metabolism
Orexin modulates calorie intake, energy consumption, and sleep; in response to metabolic signals such as peripheral blood glucose, leptin, and ghrelin levels, the neurons that produce orexin and quickly assess the body’s nutritional condition [
46]. Several studies in rats showed that intracerebroventricular injection of orexin (mainly orexin-A) in pharmacological doses increases food intake [
47,
48,
49,
50]. In contrast, in rats, intracerebroventricular injection of orexin receptor antagonists or antibodies decreases food consumption [
47,
48,
49,
50]. Orexin enhances food-seeking behavior in rats, and eating results in decreased orexin levels and low activity of hypocretinergic neurons [
51]. Moreover, diurnal fasting increases orexin levels in humans [
52].
Furthermore, it has been reported that orexin-A injection improved the mice’s basal metabolic rate (BMR) without the need for physical exercise [
53]. Additionally, orexin is a crucial central neuropeptide controlling non-exercise activity thermogenesis [
54]. Available results indicate that in male Sprague-Dawley rats, dual orexin receptor antagonists lower orexin-A-induced increases in spontaneous physical activity, total energy expenditure, and non-exercise activity thermogenesis during spontaneous physical activity, waking, rest, and sleep [
55]. Recent human studies also suggest that the orexin receptor antagonist “Suvorexant” may affect metabolism. In a study by Nakamura and Nagamine on children with insomnia who were started on the anti-orexin suvorexant, fasting insulin levels at week 8 were lower than baseline, nevertheless failed to achieve statistical significance, indicating that suvorexant at the therapeutic dose for insomnia may have beneficial effects on metabolism [
56]. Another study assessed the chronotherapeutic efficacy of suvorexant on subjective sleep parameters and metabolic parameters in patients with type 2 diabetes and insomnia, and demonstrated that abdominal circumference and daily sucrose intake were significantly decreased [
57]. A third short-term study demonstrated that 7 days of suvorexant improved daily glycemic control in patients with type II diabetes, which was coupled with changes in sympathomimetic tone and enhanced insulin sensitivity; however, anthropometric data were not reported [
58].
Orexin also controls brown adipose tissue thermogenesis and increases energy expenditure by improving non-exercise activity thermogenesis [
59]. It has been demonstrated that orexin injections increase brown adipose tissue, CO
2 generation, and thermogenesis in rats [
59]. In mice, orexins also delay the onset of diet-induced obesity by raising the sensitivity of orexin-coupled hypothalamic neurons and concurrently elevating nonesterified fatty acids and white adipose tissue levels of lipolysis [
60].
Due to these facts, the loss of orexin, in patients with narcolepsy, is logically expected to result in weight loss and hypophagia. Yet, surprisingly, obesity and overweight are highly prevalent and well-documented in patients with narcolepsy [
29,
61].
4.2. Orexin and Eating Behavior
It is hypothesized that orexigenic neuron degeneration affects the metabolic profile in different ways, resulting in binge eating behavior in a group of patients [
62] and hypophagia in others [
42]; nevertheless, the evidence regarding this hypothesis is controversial in the literature.
Through orexigenic neurons of the hypothalamus projections, the ventrotegmental area of the midbrain mediates reward-seeking behaviors [
63]. Also, the dorsomedial and paraventricular hypothalamic regions mediate food-seeking behavior through thyrotropin-releasing hormone (TRH) and corticotropin [
63]. Moreover, it is suggested that through the melanocortin pathway, orexin deficiency causes binge eating [
64]. Current evidence suggests that the prevalence of eating disorders, including bulimia and binge-eating disorders, is higher in patients with narcolepsy [
65,
66,
67]. Interestingly, rising BMI levels trigger eating disorders like bulimia [
42], which are linked to worsening symptoms of daytime sleepiness [
68].
A study used functional MRI in NT1 orexin-deficient patients to clarify the function of orexin in the neurocognitive processes generating food attentional bias and reported an increase in ventral-medial prefrontal cortex activity during food-driven attention, compared to controls [
69]. The finding that neurocognitive pathways influence NT1 patients’ processing of food cues suggests aberrant motivational brain responses to food in a condition of orexin deficit that may lead to overeating in this illness.
Studies showing a higher incidence of binge eating in patients with narcolepsy appear to be at odds with the theory that abnormal eating and sleep in binge eating disorders are associated with higher orexin activity [
70]. Using binge eating as a behavioral intervention to lessen tiredness and prevent disruptive sleep episodes may explain this phenomenon [
66]. A different, developmental stage-based notion by Barson contends that postnatal orexin cell loss decreases food intake while adult orexin cell loss enhances it [
71]. Additionally, the overeating and obesity phenotypes in adult orexin cell-knockout mice suggest that adult orexin cell loss may result in binge eating-like behavior and weight increase [
72]. Further, another study that involved the loss of orexin cells in mice between weeks 1 and 8 of age found that the loss of these cells resulted in a nearly 30% reduction in food intake [
73]. This is supported by the fact that the typical age of onset of narcolepsy is around the late second and early third decades [
74].
However, in humans, a report examining 116 patients with narcolepsy and 80 controls failed to find elevated rates of binge eating-like behavior in patients with narcolepsy [
75]. Additionally, a recent study used the Eating Disorder Evaluation Questionnaire 6th edition (EDE-Q), which is a self-report version of the Eating Disorder Examination that evaluates characteristics of eating disorders and makes four subscale results: dietary restraint, eating concern, weight concern, and shape concern [
76]. The EDE-Q total score did not differ between NT1, NT2, and controls [
76]. The above reports indicate the complexity of the association, and suggest the existence of different individual phenotypes of narcolepsy, calling for more research to explore the link between loss of orexin in patients with narcolepsy and metabolic and eating disorders.
4.3. Leptin, Ghrelin, and Other Hormonal Changes
The proteohormone leptin, an
obese gene product, is secreted by adipocytes to regulate body fat mass [
28]. The orexinergic system communicates with the hypothalamus network that responds to leptin. Orexin and leptin can stimulate and inhibit leptin-responsive cells [
28]. Leptin and orexin levels vary inversely in fasting subjects [
52,
77]. Ghrelin is an appetite-stimulating peptide that functions as a peripheral orexigen that blocks leptin’s effects [
78]. It has been suggested that the observed overweight in patients with narcolepsy may be partially attributed to changes in leptin and ghrelin levels.
A study that measured peripheral leptin levels in 42 patients with narcolepsy and 31 BMI-matched controls reported no reduction in peripheral leptin levels in patients with narcolepsy [
79]. A subsequent study reported no changes in the mean 24 h total plasma ghrelin and leptin levels or food-induced suppression of ghrelin concentrations between patients with narcolepsy and healthy controls [
80]. A third study showed no difference in serum and CSF leptin levels between NT1 patients and controls [
28].
A study that sought to find the association between BMI, orexin, and leptin levels in NT1 patients divided into low orexin levels (26 cases) and normal orexin levels (23 cases), and compared them with 46 healthy controls matched for sex and age [
81], reported a statistically significant increase in the number of obese patients (BMI > 30) in narcolepsy compared with controls. Nonetheless, the mean BMI did not differ significantly between groups. In addition, comparing the two groups of patients with narcolepsy with normal and low orexin levels, showed no statistically significant difference in the mean BMI, which suggests that mechanisms other than orexin deficiency are also involved in bodyweight changes. Furthermore, no difference in the leptin/BMI ratio was reported in patients with normal and low orexin and controls [
81], indicating a lower role for orexin on leptin. Another study found no difference in the fasting and post-prandial ghrelin levels between eight patients with narcolepsy and matched controls [
82]. On the other hand, a study reported a 50% reduction in 24 h mean plasma leptin levels in six orexin-deficient narcoleptics, compared to controls matched for fat mass, BMI, waist-to-hip ratio, age, and sex [
83]. Interestingly, the normal nocturnal acrophase of plasma leptin levels observed in controls was absent in patients with narcolepsy, suggesting a possible circadian rhythm disturbance of leptin secretion in narcolepsy [
83]. However, the study’s power was low because of the small sample size. A subsequent study on 38 patients diagnosed with NT1 reported that NT1 patients had significantly elevated CSF leptin levels compared to ethnically matched controls [
84]. Furthermore, the CSF leptin levels positively correlated with normalized BMI, and its high values may indicate leptin resistance [
84]. Nonetheless, serum leptin levels were not measured, and BMI was not matched among the two groups.
In conclusion, most of the current evidence does not support a role for leptin and ghrelin secretion in weight gain in patients with narcolepsy. The timing of sample collection and its relation to mealtimes may cause dissimilarities between different studies. Moreover, it is important to note that narcolepsy is a chronic disease, and compensatory mechanisms may develop over time [
38,
80], so investigating patients with narcolepsy in the chronic phase only, without assessing changes associated with disease onset, may generate inaccurate conclusions regarding orexin’s effect on leptin and ghrelin, and hence body weight. In addition, measuring leptin and ghrelin levels following a standard research protocol, with fixed bedtime and determined meal components and times, may not be illustrative of the patient’s real life, as leptin and ghrelin secretion is affected by several factors.
Other hormonal mechanisms have been proposed too. Animal studies have suggested that orexin deficiency increases insulin resistance. Orexin reduces insulin resistance and endoplasmic reticulum stress in the mouse liver [
85]. Furthermore, through the downregulation of insulin receptors and disruption of intracellular insulin receptor signaling, orexin deficit causes insulin resistance [
86,
87]. These results could explain why patients with narcolepsy had plasma insulin levels that were greater than those of controls. However, in humans, glucose tolerance tests of patients with narcolepsy did not substantially vary from those of the general population when controlled for BMI as a potential confounding factor [
88].
Moreover, growth hormone (GH) response to clonidine and arginine tests, showed lower levels of GH response, below the deficiency level (8 ng/mL), suggesting that GH secretion may be altered due to BMI changes in narcolepsy [
30].
5. CHANGES IN METABOLIC RATE (ENERGY EXPENDITURE) IN PATIENTS WITH NARCOLEPSY
It has been reported that preadipocytes in the brown adipose tissue of animal models with orexin deficiency may become incapable of differentiating, which in turn reduces thermogenesis and energy expenditure (89). Orexin has also been demonstrated to control the metabolism of muscle glucose via the activation of muscle sympathetic neurons and beta(2)-adrenergic transmission (87). Moreover, orexin receptor-2-deficient mice revealed lower energy expenditure when fed a high-fat diet (90). Therefore, it has been proposed that orexin may cause a lower metabolic rate in some patients with narcolepsy resulting in obesity despite eating fewer calories.
A recent systematic review investigated metabolic profiles in narcolepsy; four studies that measured BMR-RMR were assessed and found no statistically significant difference in the BMR-RMR between patients with narcolepsy (n=53) and controls (n=75) (18). Nonetheless, a meta-analysis was not performed because of the small number of studies.
In summary, measuring metabolic rate may lead to substantial insights into the pathophysiology of obesity in patients with narcolepsy. However, the limited number of studies evaluating metabolic rate in the literature and the disagreement about its reduction in patients with confirmed low orexin levels makes an association between the development of obesity and metabolic rate reduction in narcolepsy less likely. To confirm this, it would be helpful to establish a standard protocol for measuring BMR from the onset of narcolepsy, with regular follow-up of BMR and BMI in a large number of patients compared with controls matched for BMI, age, and sex, and in this regard, further research may be of additional value.
6. CONCLUSION AND FUTURE DIRECTIONS
Obesity and increased BMI and waist circumference are more prevalent among patients with narcolepsy than controls. Current evidence suggests that weight gain in narcolepsy may be higher early during the disease onset. However, the exact mechanisms of this weight gain are not known. Current evidence, though limited, does not support changes in BMR and RMR in patients with narcolepsy compared with controls except at disease onset. Moreover, current evidence did not document significant changes in different hormonal profiles related to weight gains, such as serum GH, plasma and CSF leptin, and CSF melanin-concentrating hormone levels.
Nevertheless, more work is needed to characterize the metabolic effects of orexin, including regulation of food intake with its relation to ghrelin and leptin hormones, fat and glucose metabolism, autonomic control, and energy homeostasis. Additionally, future longitudinal studies with larger sample sizes are needed to assess BMR in patients with narcolepsy under a standard protocol at the outset of narcolepsy, with regular follow-up of BMR and BMI compared to controls matched for BMI, age, and sex. Furthermore, clustering patients into different phenotypes may significantly impact our understanding of narcolepsy-related obesity.
Meanwhile, early screening for overweight and obesity in patients with narcolepsy is crucially valuable, as early non-pharmacological and pharmacological interventions could overcome the weight gain accompanying narcolepsy and reduce obesity-related complications. Patients with narcolepsy should receive proper health education about obesity and its effects. In addition, advice for a healthy lifestyle, including a healthy diet and physical exercises, could be implemented early in the management plan. Furthermore, following patients with narcolepsy in the clinic may include a periodic assessment of increased BMI and an investigation of metabolic derangements.