Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Others
This is a timeline of tuberculosis, describing especially major discoveries, advances in treatment and major organizations.
- tuberculosis
- timeline
1. Big Picture
| Year/period | Key developments |
|---|---|
| Ancient times | Typical skeletal abnormalities of tuberculosis, including characteristic Pott's deformities, are found in Egyptian mummies and are depicted in early Egyptian art. Tuberculosis is also noted in the Biblical books of Deuteronomy and Leviticus. Written texts describe tuberculosis in India as early as 3300 years ago and in China 2300 years ago. Tuberculosis is well known in classical Greece, where it is called phthisis.[1][2] |
| Middle Ages and Renaissance | The incidence of tuberculosis grows progressively in these times, displacing leprosy, peaking between the 18th and 19th century as field workers move to the cities looking for work.[3] In parts of Europe, tuberculosis is known as the “king’s evil” and is widely believed that the kings of England and France can cure scrofula simply by touching those affected.[4] |
| 1700s–1800s | Description of tuberculosis is developed in medical literature. Toward 1800s sanatoria start to open for treating patients, with often successful outcomes. Understanding of the pathogenesis of tuberculosis begins with the works of Laennec, Villemin and the identification of the tubercle bacillus as the etiologic agent by Robert Koch. |
| 1920s–1930s | The International Union Against Tuberculosis (IUAT) is founded. BCG vaccine against tuberculosis is developed. Several international conferences are held, focusing on the fundamental, biological, clinical and social aspects of tuberculosis.[5] |
| 1940s onward | During the Nazi occupation of Poland, SS-Obergruppenführer Wilhelm Koppe organized the execution of more than 30,000 Polish patients suffering from tuberculosis - little knowing or caring that by that time, a cure was nearly achieved. The isolation of streptomycin is generally considered the beginning of the modern era of tuberculosis. The revolution continues with the development of isoniazid, the first oral mycobactericidal drug. The advent of rifampin in the 1970s hastens recovery times, and significantly reduces the number of tuberculosis cases in the following years.[6][7]
In Italy for some decades the Italian competitor of the French tubercular vaccine BCG vaccine.was the Salvioli's diffusing vaccine (acronym 'VDS from its Italian name Vaccino Diffondente Salvioli) used from 1948 until 1976. It was prepared by professor Gaetano Salvioli (1894–1982) of the University of Bologna. |
| 1980s onward | Tuberculosis drug-resistant strains appear, provoking a rise in incidence in countries like Britain. Also, the association with AIDS has contributed to the rise of tuberculosis in some sectors.[8] |
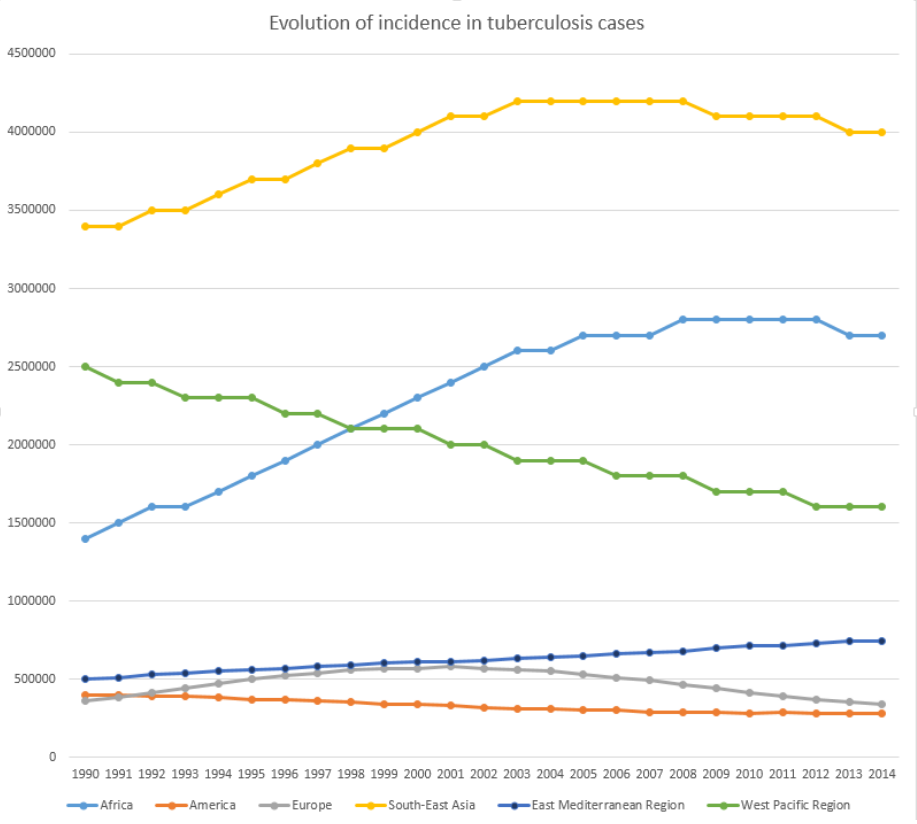
| Present | Today, tuberculosis continues to be a top infectious disease killer worldwide. However, the death rate has dropped 47% since 1990. Over 95% of cases and deaths are in developing countries, with the most severe burden in Africa.[9] At least 1 million children fall ill with tuberculosis each year, represent about 11% of all cases.[10] |
2. Full Timeline
| Year/period | Type of event | Event | Location |
|---|---|---|---|
| 1689 | Development | English physician Richard Morton first states that tubercles are always present in the tuberculosis disease of the lungs.[12] | England |
| 1761 | Development | Austrian physician Leopold Auenbrugger develops a percussion method for diagnosing tuberculosis.[13] | |
| 1768 | Development | Scottish physician Robert Whytt gives the first clinical description of tuberculous meningitis.[14] | |
| 1779 | Development | English surgeon Percivall Pott first describes the arthritic tuberculosis of the spine (today known as Pott disease).[15] | |
| 1810 | Development | French physician Gaspard Laurent Bayle publishes his article Recherches sur la Pthisie Pulmonaire, in which he divides phthisis into six types: tubercular phthisis, glandular phthisis, ulcerous phthisis, phthisis with melanosis, calculous phthisis, and cancerous phthisis, basing his findings on more than 900 autopsies.[16] | |
| 1816 | Development | French physician René Laennec, working at the Necker-Enfants Malades Hospital, develops the stethoscope, which proves to be a breakthrough. The stethoscope marks a major step in the redefinition of disease from being a bundle of symptoms, to the current sense of a disease as a problem with an anatomical system even if there are no noticeable symptoms. The work of Laennec is considered to have clearly elucidated the pathogenesis of tuberculosis and unified the concept of the disease, whether pulmonary or extrapulmonary.[17][18] | Paris, France |
| 1839 | Development | German naturalist Johann Lukas Schönlein is attributed with naming the disease tuberculosis.[19] | |
| 1854 | Organization | Hermann Brehmer establishes the first German sanatorium for the systematic open-air treatment of tuberculosis, with treatment including adjusting lifestyle at high altitude, abundant diet with some alcohol, and exercise in the open air under strict medical supervision. The results are eventually regarded as highly successful, surpassing any previous treatment.[20] | Strehlen, Prussia |
| 1865 | Development | French physician Jean Antoine Villemin demonstrates of the transmissibility of Mycobacterium tuberculosis.[2] | France |
| 1882 | Discovery | German physician Robert Koch, a founder of modern bacteriology, identifies the tubercle bacillus as the etiologic agent that causes tuberculosis. Some years later, Koch develops what today is known as Koch's postulates, which he applies to describe the etiology of cholera and tuberculosis. Koch is also attributed for having created and improved laboratory technologies and techniques in the field of microbiology, and making key discoveries in public health. Koch receives the Nobel Prize in Physiology or Medicine in 1905.[2] | |
| 1890 | Discovery | Hungarian physiologist Franz Tangl publishes what later became known as Baumgarten-Tangl law, stating that the location where the bacteria intrudes is the one where the inflammation can be observed first.[21] | |
| 1900 | Study | French bacteriologists Albert Calmette and Camille Guérin begin research for an antituberculosis vaccine at the Pasteur Institute.[22] | Lille, France |
| 1903 | Organization | American entrepreneur Henry Phipps, Jr. founds the Phipps Institute for the Study, Treatment and Prevention of Tuberculosis at the University of Pennsylvania.[23] | Philadelphia, US |
| 1904 | Organization | The National Association for the Study and Prevention of Tuberculosis (NASPT) is founded.[24] | |
| 1907 | Development | French physician Charles Mantoux introduces his eponymous Mantoux test as a serological skin test to determine whether a person is infected with tuberculosis.[25] | |
| 1908 | Development | French physician Charles Mantoux, perfects test for diagnosis of tuberculosis contact (latent tuberculosis).[26] | |
| 1909 | Organization | American philanthropist Nathan Straus opens the first preventorium for patients infected with tuberculosis.[27] | |
| 1921 | Development | Bacillus Calmette–Guérin (BCG) vaccine is first administered. It is still the only vaccine available against tuberculosis.[22] | Paris, France |
| 1930 | Crisis | Lübeck disaster. 250 newborn babies are given doses of BCG contaminated by virulent tubercle bacilli. After four to six weeks a large number of the infants develop tuberculosis. 73 babies die in the first year and another 135 are infected but finally recover.[22] | Lübeck, Germany |
| 1932 | Development | The Löwenstein–Jensen medium is developed as diagnosis for tuberculosis. It is used for culture of Mycobacterium species, notably Mycobacterium tuberculosis.[28] | |
| 1936 | Development | Brazilian physician Manuel de Abreu develops chest photofluorography, a technique for mass screening for tuberculosis.[29] | Rio de Janeiro, Brazil |
| 1944 | Development | Swedish chemist Jörgen Lehmann develops antibiotic 4-aminosalicylic acid for treating tuberculosis.[30] | |
| 1944 | Development | Albert Schatz, Elizabeth Bugie, and Selman Waksman at Rutgers University isolate streptomycin, the first antibiotic and first bacterial agent effective against tuberculosis.[31] | New Jersey, US |
| 1946–1948 | Treatment | The first randomized trial of streptomycin against pulmonary tuberculosis is carried out.[32][33] | United States |
| 1948 | Treatment | Researchers at Britain's Medical Research Council demonstrate that combined treatment with streptomycin and 4-aminosalicylic acid is superior to either drug alone.[34] | UK |
| 1950 | Campaign | Mass tuberculosis immunization is under way with the BCG vaccine. This vaccine is recommended to be given intradermally, immediately after birth. This vaccine is mandatory to attend school in France between 1950 and 2007, introduced in Brazil in 1967, and to the Philippines in 1979.[35][36][37] | |
| 1952 | Discovery | Isoniazid is first used in the treatment of tuberculosis.[2][38] | |
| 1952 | Treatment | The amino acid derivative cycloserine is first isolated. It is found to be effective against Mycobacterium tuberculosis.[39] | |
| 1962 | Treatment | The bacteriostatic drug ethambutol is developed as a medication primarily used to treat tuberculosis.[40] | |
| 1971 | Treatment | The antibiotic rifampicin is first sold as a medication to treat several types of bacterial infections, including tuberculosis.[41] | |
| 1976 | Organization | The Seattle Biomedical Research Institute (today known as Center for Infectious Disease Research) is founded as a non-profit organization focused solely on infectious disease discovery research, including tuberculosis.[42][43] | Issaquah, Washington, US |
| 1995 | Program launch | The World Health Organization launches DOTS (Directly Observed Treatment, Short-Course) program as a control strategy for tuberculosis. DOTS works as an intermittent, supervised system of drug intake by patient, which eliminates drug default. DOTS has been described by WHO as "the most important public health breakthrough of the decade in terms of lives saved".[44][45] | |
| 1998 | Development | The mycobacterium tuberculosis (H37Rv strain) genome is sequenced, with aims at helping scientists develop better therapies, ranging from treatments for tuberculosis to vaccines to prevent it.[46][47] | |
| 1999 | Campaign | Médecins Sans Frontières launch the Campaign for Access to Essential Medicines. It pushes to lower the prices of existing drugs, vaccines and diagnostic tests, to stimulate research and development into new treatments for diseases (tuberculosis among them) that primarily affect the poor.[48] | |
| 2000 | Organization | The Mycobacterium tuberculosis Structural Genomics Consortium is formed as a worldwide consortium of scientists with the goal of providing a structural basis for the development of therapeutics for tuberculosis. The consortium has five core facilities (located at Lawrence Livermore National Laboratory, Los Alamos National Lab, Lawrence Berkeley National Laboratory, University of California, Los Angeles and Texas A&M University) that carry out an increasing fraction of routine tasks such as protein production, crystallization and X-ray data collection.[49] | United States |
| 2000 | Organization | The Global Alliance for TB Drug Development (TB Alliance) is established as a nonprofit organization dedicated to the discovery and development of new, faster-acting and affordable tuberculosis medicines.[50] | Cape Town, South Africa |
| 2001 | Organization | The Stop TB Partnership is established with the purpose of eliminating tuberculosis as a public health problem. It has 1000 partner organizations, including international, nongovernmental and governmental organizations and patient groups.[51] | Geneva, Switzerland |
| 2002 | Organization | The Global Fund to Fight AIDS, Tuberculosis and Malaria is founded as an international financing institution dedicated to attract and fund additional resources to stop and treat those diseases.[52] | Geneva, Switzerland |
| 2006 | Organization | Unitaid is launched as a global health initiative. It provides sustainable funding in order to tackle inefficiencies in markets for medicines, diagnostics and prevention for HIV/AIDS, malaria and tuberculosis in developing countries. UNITAID finances its project through the international solidarity levy on airline tickets that is currently collected in nine out of 29 UNITAID member countries.[53] | France, Brazil, Chile, Norway and United Kingdom |
| 2008 | Organization | The Millennium Foundation for Innovative Finance for Health is established. Its project MassiveGood is meant to collect funds for combating HIV/AIDS, malaria and tuberculosis.[54] | United States, United Kingdom, Germany, Austria, Switzerland and Spain (serves worldwide) |
| 2009 | WHO calls for universal access to tuberculosis culture by 2015.[28] | ||
| 2012 | Treatment | FDA approves bedaquiline for treating multi-drug-resistant tuberculosis. It is the first new medicine for tuberculosis in more than forty years.[55][56] | United States |
| 2012 | Report | 155 000 people fall ill with tuberculosis in low-incidence countries, averaging 10,000 deaths (30 TB deaths a day).[57] | |
| 2012 | Report | More than 180 countries sign a pledge, vowing to redouble efforts to stop children from dying of preventable diseases, including tuberculosis.[10] | |
| 2014 | Report | The World Health Organization and partners launch first-ever targeted and costed roadmap with key steps to scale up the response to childhood tuberculosis and end childhood tuberculosis-related deaths.[10] | United States (Washington DC) |
| 2014 | Report | At a global level, 9.6 million people fell ill with tuberculosis and 1.5 million died from the disease in 2014.[9] |
The content is sourced from: https://handwiki.org/wiki/Medicine:Timeline_of_tuberculosis
References
- Thomas, M. Daniel (2006). "The history of tuberculosis". Respiratory Medicine 100 (11): 1862–1870. doi:10.1016/j.rmed.2006.08.006. PMID 16949809. http://www.resmedjournal.com/article/S0954-6111%2806%2900401-X/fulltext#back-bib19.
- Daniel, Thomas M. (2006). "The history of tuberculosis". Respiratory Medicine 100 (11): 1862–1870. doi:10.1016/j.rmed.2006.08.006. PMID 16949809. http://www.resmedjournal.com/article/S0954-6111%2806%2900401-X/fulltext. Retrieved 2 September 2016.
- Aufderheide 1998:129
- "History of Tuberculosis". 11 December 2009. http://www.news-medical.net/health/History-of-Tuberculosis.aspx. Retrieved 2 September 2016.
- "History of Tuberculosis". http://www.theunion.org/who-we-are/history. Retrieved 3 September 2016.
- "Box 1: History of tuberculosis drug development". http://www.nature.com/nrd/journal/v12/n5/box/nrd4001_BX1.html. Retrieved 5 September 2016.
- Raviglione, Mario C. (2016-04-19). Tuberculosis: The Essentials, Fourth Edition. p. 113. ISBN 9781420090239. https://books.google.com/books?id=IlvvBQAAQBAJ&pg=PA113&lpg=PA113&dq=%22isoniazid%22+%22revolution%22#v=onepage.
- "Tuberculosis (TB) and other mycobacterial diseases: diagnosis, screening, management and data". https://www.gov.uk/government/collections/tuberculosis-and-other-mycobacterial-diseases-diagnosis-screening-management-and-data. Retrieved 10 September 2016.
- "Tuberculosis". http://www.who.int/mediacentre/factsheets/fs104/en/. Retrieved 9 September 2016.
- "ENDING TUBERCULOSIS IN CHILDREN". WHO. http://www.who.int/tb/challenges/childhood_tb_informationsheet.pdf?ua=1. Retrieved 21 January 2017.
- "Mortality and prevalence Data by WHO region (all years)". http://apps.who.int/gho/data/view.main.57016ALL?lang=en. Retrieved 22 November 2016.
- Kontić, O; Vasiljević, N; Jorga, J; Lakić, A; Jasović-Gasić, M (2009). "Richard Morton (1637-1698)--the distinguished physician of the 17th century". Srp Arh Celok Lek 137 (11–12): 706–9. PMID 20069934. http://www.ncbi.nlm.nih.gov/pubmed/20069934
- Walker, Kenneth (1990). The Origins of the History and Physical Examination. Butterworths. ISBN 9780409900774. https://www.ncbi.nlm.nih.gov/books/NBK458/#A25.
- Breathnach, CS (2014). "Robert Whytt (1714-1766): from dropsy in the brain to tuberculous meningitis.". Ir J Med Sci 183 (3): 493–9. doi:10.1007/s11845-014-1106-3. PMID 24682631. https://dx.doi.org/10.1007%2Fs11845-014-1106-3
- "Pott disease". http://emedicine.medscape.com/article/226141-overview. Retrieved 5 September 2016.
- "Complete Record - Heirs of Hippocrates No. 1291". http://fm.iowa.uiowa.edu/fmi/xsl/hardin/heirs/record_detail.xsl?-db=heirs&-lay=WebLayout&-recid=1483&-find=. Retrieved 5 September 2016.
- Duffin, Jacalyn. "Big Ideas: Jacalyn Duffin on the History of the Stethoscope". TVO. Archived from the original on 27 September 2013. https://web.archive.org/web/20130927173037/http://ww3.tvo.org/video/182217/jacalyn-duffin-history-stethoscope. Retrieved 9 September 2016.
- Daniel, Thomas M. (2006). "The history of tuberculosis". Respiratory Medicine 100 (11): 1862–1870. doi:10.1016/j.rmed.2006.08.006. PMID 16949809. https://dx.doi.org/10.1016%2Fj.rmed.2006.08.006
- Zur Pathogenie der Impetigines. Auszug aus einer brieflichen Mitteilung an den Herausgeber. [Müller's] Archiv für Anatomie, Physiologie und wissenschaftliche Medicin. 1839, page 82.
- McCarthy, O R (August 2001). "The key to the sanatoria". J R Soc Med 94 (8): 413–7. doi:10.1177/014107680109400813. PMID 11461990. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1281640
- "Baumgarten-Tangl law". http://www.whonamedit.com/synd.cfm/846.html. Retrieved 4 September 2016.
- Luca, S; Mihaescu, T (2013). "History of BCG Vaccine". Maedica 8 (1): 53–8. PMID 24023600. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3749764
- "HENRY PHIPPS INSTITUTE". The New York Times. 10 January 1903. https://query.nytimes.com/gst/abstract.html?res=9800E7DA1030E733A25753C1A9679C946297D6CF&legacy=true. Retrieved 5 September 2016.
- "Introduction to the American Lung Association and the Fight against Tuberculosis". http://exhibits.hsl.virginia.edu/alav/. Retrieved 2 September 2016.
- Horvat, RT (2015). "Gamma Interferon Assays Used in the Diagnosis of Tuberculosis". Clin Vaccine Immunol 22 (8): 845–9. doi:10.1128/CVI.00199-15. PMID 26018533. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4519719
- Mazana, JS (2009). "Tuberculosis and its eponyms: Charles Mantoux (1877-1947)". Rev Esp Sanid Penit 11 (1): 17–23. doi:10.4321/S1575-06202009000100004. PMID 23128409. https://dx.doi.org/10.4321%2FS1575-06202009000100004
- "The Garrett Building: An Architectural Record of the Children's Preventorium Movement". http://www.faculty.virginia.edu/blueridgesanatorium/preventorium.html. Retrieved 4 September 2016.
- "Does TB culture impact on clinical decision - making?". http://www.teachepi.org/documents/courses/tbdiagrx/day2/Hepple_Does%20TB%20culture%20impact%20on%20clinical%20decision-making%2005.07.2011.pdf. Retrieved 3 September 2016.
- "Portraits of our lungs". http://revistapesquisa.fapesp.br/en/2015/02/28/portraits-of-our-lungs/. Retrieved 3 September 2016.
- Lehmann, J. (1946). "Para-aminosalicylic acid in the treatment of tuberculosis". Lancet 1 (6384): 15–16. doi:10.1016/s0140-6736(46)91185-3. PMID 21008766. https://dx.doi.org/10.1016%2Fs0140-6736%2846%2991185-3
- Boyd Woodruff, H. (2013). "Selman A. Waksman, Winner of the 1952 Nobel Prize for Physiology or Medicine". Appl Environ Microbiol 80 (1): 2–8. doi:10.1128/AEM.01143-13. PMID 24162573. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3911012
- Comroe JH Jr (1978). "Pay dirt: the story of streptomycin. Part I: from Waksman to Waksman". American Review of Respiratory Disease 117 (4): 773–781. doi:10.1164/arrd.1978.117.4.773. PMID 417651. https://dx.doi.org/10.1164%2Farrd.1978.117.4.773
- Kingston W (July 2004). "Streptomycin, Schatz v. Waksman, and the balance of credit for discovery". J Hist Med Allied Sci 59 (3): 441–62. doi:10.1093/jhmas/jrh091. PMID 15270337. https://dx.doi.org/10.1093%2Fjhmas%2Fjrh091
- Fox, W.; Ellard, G. A.; Mitchison, D. A. (1999). "Studies on the treatment of tuberculosis undertaken by the British Medical Research Council tuberculosis units, 1946-1986, with relevant subsequent publications". The International Journal of Tuberculosis and Lung Disease 3 (10 Suppl 2): S231–S279. PMID 10529902. http://www.ncbi.nlm.nih.gov/pubmed/10529902
- "WHO in 60 years: a chronology of public health milestones". World Health Organization. http://www.who.int/features/history/WHO_60th_anniversary_chronology.pdf. Retrieved April 2, 2016.
- Loi n° 50-7 du 5 janvier 1950
- décret n° 2007-1111 du 17 juillet 2007
- Siddiqi, Salman; Takhar, Param; Baldeviano, Christian; Glover, William; Zhang, Ying (2007). "Isoniazid Induces Its Own Resistance in Nonreplicating Mycobacterium tuberculosis". Antimicrobial Agents and Chemotherapy 51 (6): 2100–2104. doi:10.1128/AAC.00086-07. PMID 17438054. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1891357
- Donald, P.R. (2011-09-07). Antituberculosis Chemotherapy. p. 88. ISBN 9783805596282. https://books.google.com/books?id=aZc7AQAAQBAJ&pg=PA88&lpg=PA88&dq=%22Cycloserine%22+%22isolated+in%22#v=onepage.
- Garg, P; Garg, R; Prasad, R; Mishra, AK (2015). "A prospective study of ocular toxicity in patients receiving ethambutol as a part of directly observed treatment strategy therapy". Lung India 32 (1): 16–9. doi:10.4103/0970-2113.148428. PMID 25624590. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4298911
- Oxford Handbook of Infectious Diseases and Microbiology. OUP Oxford. 2009. p. 56. ISBN 978-0-19-103962-1. https://books.google.com/books?id=5W-WBQAAQBAJ&pg=PT56.
- "Seattle Biomedical Research Institute". http://startupgenome.com/organizations/acquisitions/seattle-biomedical-research-institute. Retrieved 21 November 2016.
- "Center for Infectious Disease Research". http://www.cidresearch.org/. Retrieved 4 September 2016.
- "DOTS". http://www.wpro.who.int/mediacentre/factsheets/20120306_tuberculosis/en/index2.html. Retrieved 21 November 2016.
- Murali, M S (2002). "DOTS strategy for control of tuberculosis epidemic.". Indian J Med Sci 56 (1): 16–8. PMID 12508626. http://www.ncbi.nlm.nih.gov/pubmed/12508626
- "1998: M. Tuberculosis Bacterium Sequenced". https://www.genome.gov/25520389/online-education-kit-1998-m-tuberculosis-bacterium-sequenced/. Retrieved 9 September 2016.
- "Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence". Nature 393 (6685): 537–44. June 1998. doi:10.1038/31159. PMID 9634230. Bibcode: 1998Natur.393..537C. https://dx.doi.org/10.1038%2F31159
- Butler, Christopher (2007). "Human Rights and the World Trade Organization: The Right to Essential Medicines and the TRIPS Agreement". Journal of International Law & Policy 5: 1–27. http://www.law.upenn.edu/journals/jil/jilp/articles/5-1_Butler_Christopher.pdf. Retrieved 4 September 2016.
- "Mycobacterium tuberculosis Structural Genomics Consortium". http://www.biologybrowser.org/node/1153243. Retrieved 5 September 2016.
- "Global Alliance for TB Drug Development (TB Alliance)". http://partnerships.ifpma.org/partnership/global-alliance-for-tb-drug-development-tb-alliance. Retrieved 5 September 2016.
- "Our Hosting Arrangement". http://www.stoptb.org/about/hosting.asp. Retrieved 4 September 2016.
- "Global Fund Overview". http://www.theglobalfund.org/en/overview/. Retrieved 21 November 2016.
- "About UNITAID". http://globalhealthsciences.ucsf.edu/global-health-group/evidence-to-policy-initiative-e2pi/smarter-aid/about-unitaid. Retrieved 5 September 2016.
- "Taskforce on Innovative International Financing for Health Systems: showing the way forward". http://www.who.int/bulletin/volumes/88/6/09-075507/en/. Retrieved 4 September 2016.
- "FDA Approves 1st New Tuberculosis Drug in 40 Years". ABC News. https://abcnews.go.com/Health/wireStory/fda-approves-tuberculosis-40-years-18100650#.UOIPT-RQWe0. Retrieved 3 September 2016.
- Thomas, Katie (31 December 2012). "F.D.A. Approves New Tuberculosis Drug". New York Times. https://www.nytimes.com/2013/01/01/business/fda-approves-new-tuberculosis-drug.html?_r=0. Retrieved 3 September 2016.
- "TB elimination". WHO. http://www.who.int/tb/publications/Towards_TB_Eliminationfactsheet.pdf?ua=1. Retrieved 21 January 2017.
This entry is offline, you can click here to edit this entry!
