Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Hemorrhoids are blood cushions located into the anus and lower rectum, acknowledged as a common cause of bleeding, which can reduce the quality of life. The development of minimally invasive techniques such as endovascular embolization of superior rectal artery, "Emborrhoid technique", is an effective treatment, with no pain or ischemic complications, and allows quick patient recovery.
- hemorrhoid
- superior rectal artery
- bleeding
1. Introduction
Hemorrhoids (HD) are the most prevalent disease in the anorectal disorders field, representing 4% to 35% of the population; patients between 45 and 65 years old make up the highest incidence [1]. The classification of HD between internal and external comes from their location, whether above or below the dentate line (pectinate line). Internal HD often manifest with rectal bleeding, which reduces quality of life and may result in anemia [2][3].
They can be graded using the Goligher classification (GC) (Table 1), based on their degree of prolapse, and the French bleeding score (FBS) (Table 2), with a top score of 9, which implies the most intense bleeding [4].
Table 1. Goligher classification.
| Grade | Description |
|---|---|
| 1 | Bleeding with no protrusion |
| 2 | Protrusion spontaneously reduced |
| 3 | Protrusion needing digital reduction |
| 4 | Irreducible protrusion |
Table 2. French Bleeding Score.
| Frequency (0–4) |
Never | 0 |
| >1 per year | 1 | |
| >1 per month | 2 | |
| >1 per week | 3 | |
| >1 per day | 4 | |
| Bleeding (0–3) |
Never | 0 |
| At wiping | 1 | |
| In the toilet | 2 | |
| On underwear | 3 | |
| Anemia (0–2) |
Never | 0 |
| Without transfusion | 1 | |
| With transfusion | 2 |
Conservative management as dietary measures and topical medications can treat bleeding in the first instance [5][6][7][8]. However, 10% of all patients will need surgery such as conventional hemorrhoidectomy (CH) [9], circular anopexia [10], or stapled hemorrhoidopexy (SH) [11]. Over the years, less invasive techniques such as rubber band ligation (RBL) [12][13], sclerotherapy (SCL) [14][15][16], and infrared coagulation have been developed, allowing an outpatient setting and a quicker patient recovery, despite an increased recurrence. Recently, minimally invasive techniques based on the hyperflow of hemorrhoidal arteries, such as transanal hemorrhoidal dearterialization (THD) [17], doppler-guided hemorrhoidal artery ligation (DGHAL) [18][19], or its endovascular version, the “Emborrhoid technique” [20][21], have emerged, showing promising results and more patient comfort (Table 3) [22].
Table 3. Existing treatments for hemorrhoids.
| Technique | Description | Indications | Advantages | Disadvantages |
|---|---|---|---|---|
| Conservative treatment: fiber, laxatives, phlebotonics | Improvement of stool consistency and vascular tone | Control of symptoms of HD grade I and II | Well tolerated with low adverse effects, symptoms relief | No changes in pathophysiology |
| Rubber band ligation (RBL) | With a proctoscope a rubber band is applied in each hemorrhoid to cause ischemia, followed by shrinkage and fibrosis | HD grade I, II, and III not responding to conservative management | Outpatient treatment, non-invasive procedure, more cost-effective, less recurrence rate than SCL and IRC | Relatively contraindicated in patients with anticoagulants, bleeding, or inflammatory disorders More painful than other outpatient procedures |
| Sclerotherapy (SCL) | The sclerosant injection into each hemorrhoid generates local inflammation and scarring | HD grade I, II, and III not responding to conservative management | Outpatient treatment, early improvement in bleeding and protrusion symptoms | Painful intraprocedural injection Mucosal ulceration up to 3.6% of patients Recurrence between 15–80% after the first year |
| Infrared coagulation | Infrared light applied directly to each hemorrhoid causes vessel coagulation followed by ischemia and scarring | HD grade I, II, and III not responding to conservative management | Outpatient treatment Coagulation of the internal hemorrhoid immediately visible Good patient improvement in I and II HD degree |
Postprocedural pain and bleeding Insufficient data on long-term efficacy |
| Stapled hemorrhoidopexy (SH) | A trans-anal circular stapler sections circularly the hemorrhoidal network 4 cm above the dentate line. | HD grade III and IV (irreducible protrusion) | Non-excisional procedure Less operating time and hospital stay than CH |
Higher recurrence than CH Early bleeding Early fecal urgency up to 8% of patients |
| Transanal hemorrhoidal dearterialization (THD) or Doppler-guided hemorrhoidal artery ligation (DGHAL) | A proctoscope and a Doppler transducer are used to recognize and ligate distal branches of the SRA above the dentate line. If combined with mucopexy, sutures are used to ensure the hemorrhoidal tissue in place. | II and III HD degree, and possibly IV in experienced surgeons | Low postprocedural pain and faster recovery than CH, SH, and RBL Added targeted mucopexy can be performed to treat prolapse |
Higher recurrence rates than CH Tenesmus and pain if added mucopexy |
| Conventional hemorrhoidectomy (CH) | By an open (Milligan-Morgan) or closed (Ferguson) incision at the mucocutaneous junction the hemorrhoid cushion is exposed and excised | First choice for HD grade III and IV | Gold standard Lowest recurrence rate among all the techniques |
Longer operating time and postoperative pain More loss of working days Fecal incontinence in 6% of the patients |
| Embolization of superior rectal artery (HE) | By angiography it is possible to identify and therefore occlude all the distal branches dependent on the SRA, lowering the vascular supply of internal hemorrhoids | HD grade II and III in patients with contraindications to surgery or refractory symptoms | Outpatient treatment Avoids rectal manipulation Preserves anal continence Quick and effective reduction of bleeding |
Radiation No changes in prolapse Need for a second embolization in anatomy variants with high blood supply by MRA or IRA |
| Hemorrhoidal Laser Procedure | A Doppler transducer is used to detect the terminal branches of the SRA 2.5 cm above the dentate line, then a 980-nm diode causes shrinkage, thus reducing the blood supply | HD grade II and III IV if rectoanal repair or mucopexy is associated |
Outpatient treatment It shares the foundation of DGHAL and THD but is less invasive and does not require general anesthesia |
Postoperative bleeding and pain in up to 9% of cases |
| Laser hemorrhoidoplasty | After making a 1-mm opening, a fiber delivers 15 W pulses, inducing shrinkage of underlying tissues up to 5 mm in depth | HD grade II and III | It reduces postoperative pain and analgesics need if compared with CH | Recurrence up to 39% of patients |
Among the main advantages of hemorrhoid embolization (HE) compared with other therapies is the identification and therefore, the occlusion of all branches dependent on the superior rectal artery (SRA) and any anastomoses with the middle rectal artery (MRA) and the inferior rectal artery (IRA), which reduces recurrence of bleeding. Compared to surgery, the endovascular approach avoids rectal manipulation, eliminating the risk of rectal trauma, allowing the preservation of anal continence. Coil and particle embolization of the SRA has been found to be a well-tolerated, effective, and safe technique [23][24][25][26][27][28].
Clear indications and patient selection have not been fully specified. The Italian society of colorectal surgery [22] indicates HE to patients suffering refractory symptoms from II and III HD degrees with contraindications to surgery (level of evidence 2, grade of recommendation C).
Some studies have analyzed the impact of HE on frail patients with severe cardiovascular, pulmonary, or neurological disease, which usually contraindicates the use of general anesthesia, finding excellent modifications in hemorrhoid bleeding, anemia, and patient’s quality of life after the endovascular procedure [23]. Patients with congenital or acquired bleeding disorders have shown good responses to HE, even without suspending antiplatelet or anticoagulant therapy [24][25]. Inflammatory bowel disease stays controversial as it appears as a particular indication or contraindication in the different literature [23][25][26]. Nowadays, it is also a suitable procedure for young surgical candidates who are averse to direct rectal manipulation [27].
As contraindications, it can be found any situation that risks an endovascular procedure, like platelet count inferior to 50,000/μL, international normalized ratio (INR) superior to 1.5, allergy or intolerance to contrast media, non-available vascular access, or sepsis. Special situations that contraindicate HE are rectosigmoid resection, colorectal cancer, colonic angiodysplasia, or acute anorectal infection [23].
Considerable studies have been published on this subject, commonly using right transfemoral access (TFA). Nonetheless, many recent studies have demonstrated that transradial access (TRA) has faster ambulation and discharge but a higher radiation dose for not radial access trained specialists [26][28].
2. Anatomy
The rectum is mainly supplied by the SRA, a branch of the inferior mesenteric artery (IMA), and to a lesser extent by the MRA and IRA, branches of the internal iliac artery.
The IMA origins from the anterior and left aspect of the abdominal aorta, immediately above the iliac bifurcation, at the level of the third lumbar vertebra, and bifurcates into the left colic artery, the sigmoid arteries, and the SRA, shown in Figure 1.
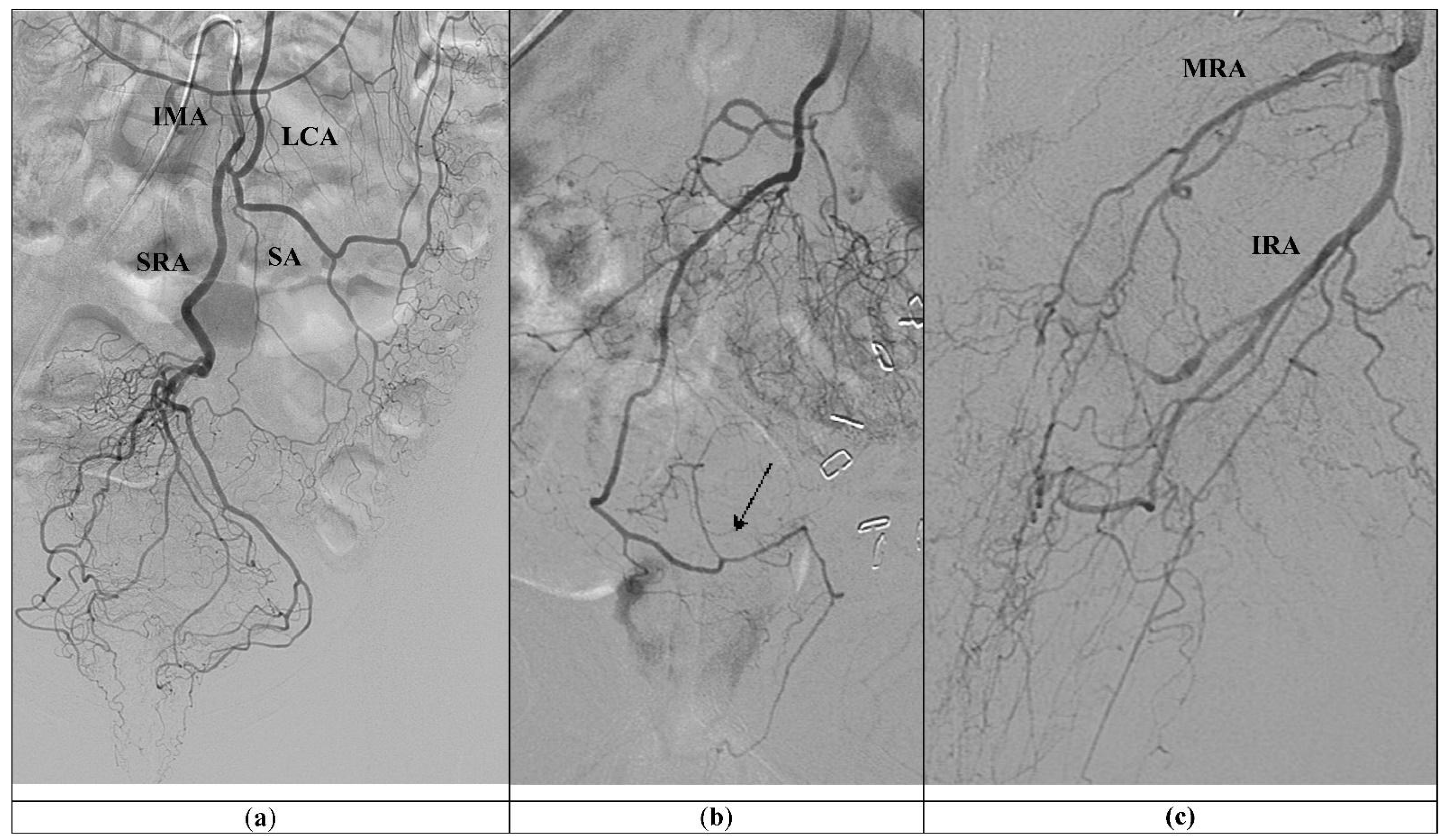
Figure 1. (a) Standard vascular anatomy of IMA: left colic artery (LCA), sigmoid arteries (SA), and type I superior rectal artery (SRA) are visualized after contrast injection. (b) Type II SRA: a right main trunk crosses and gives branches to the left (arrow). (c) Prominent left middle rectal artery (MRA) and inferior rectal artery (IRA) give the main blood supply to the left wall of the distal rectum.
The anatomy of SRA was first described by Thomson in 1975, who found a common pattern in almost half of the cases, named as type I, where the main trunk divides into posterior-right and posterior-left branches and lateral-right and lateral-left branches, four branches in total. The rest of the cases were grouped into type II, where a right main trunk crosses and gives branches to the left, in type III, a left main trunk supplies the left side with a high contribution of the MRA to the corpus cavernosum recti (CCR), and type IV, the main trunk trifurcates, while in type V, the branches of the trifurcation do not reach the anal canal, because its main blood supply is done by the MRA [23][24].
3. General Technique
The “Emborrhoid technique” is generally indicated for patients with hemorrhoids type II or III and significant rectal bleeding, who have contraindications or refuse surgery, hence support by the coloproctology department must be facilitated.
Prior explanation of risk and benefit and informed consent must be obtained from each patient. Once fasting and adequate hemostasis are confirmed, the procedure is performed under aseptic conditions in a room equipped with a digital angiography. Conscious sedation is used, and local anesthetic is injected at the puncture site, which most commonly is the right femoral artery [25][26][27][28][29][30].
Simmons 2 5F (Radifocus; Terumo, Tokyo, Japan) is the most common catheter utilized to select the origin of the IMA [31][32]. In difficult catheterizations, it is also helpful to perform an inferior abdominal aortography with a Pig-tail 5F (Radifocus; Terumo, Belgium, Leuvem) (Merit; Utah, USA) and locate the c-arm in a lateral position [28].
Subsequently, there is the catheterization of the SRA with a 2.4 up to 2.7 F Progreat microcatheter® (Radifocus; Terumo, Tokyo, Japan), Direxion microcatheter HI-FLO Bern shape or J shape® (Boston Scientific; Marlborough, MA, USA) or RapidTransit microcatheter® (Cordis Endovascular Systems, Miami Lakes, FL, USA). Angiography of the SRA branches and anastomoses with MRA and inferior rectal artery (IRA) can be acquired.
Embolization of bilateral posterior and lateral branches can be performed with 2–3 mm pushable coils, such as Nester® (Cook Medical; Bloomington, IN, USA), or detachable coils, such as Target® (Stryker; Cork, Ireland) or Interlock (Boston Scientific; Marlborough, MA, USA). Some authors report bigger coil sizes of 4 to 7 mm with similar results [25][30]. Coils are the most often documented embolic material; regardless, the usage of particles and coils is preferred by some working groups. Previous injection of 300–500 μm polyvinyl alcohol (PVA) particles within the distal part of SRA branches, near the CCR; followed by coil embolization of the SRA branches themselves, may close hemorrhoid plexus more distally and obstruct persistent MRA anastomoses, as shown in Figure 2 (Table 4) [25][26][27][28][29][30][31][32]. A recent study showed that larger microspheres (900–1200 μm) have better long-term efficacy and no minor ischemic complications compared with smaller sizes [33]. Other embolization agents, like gel foam particles, have been proven effective [34].
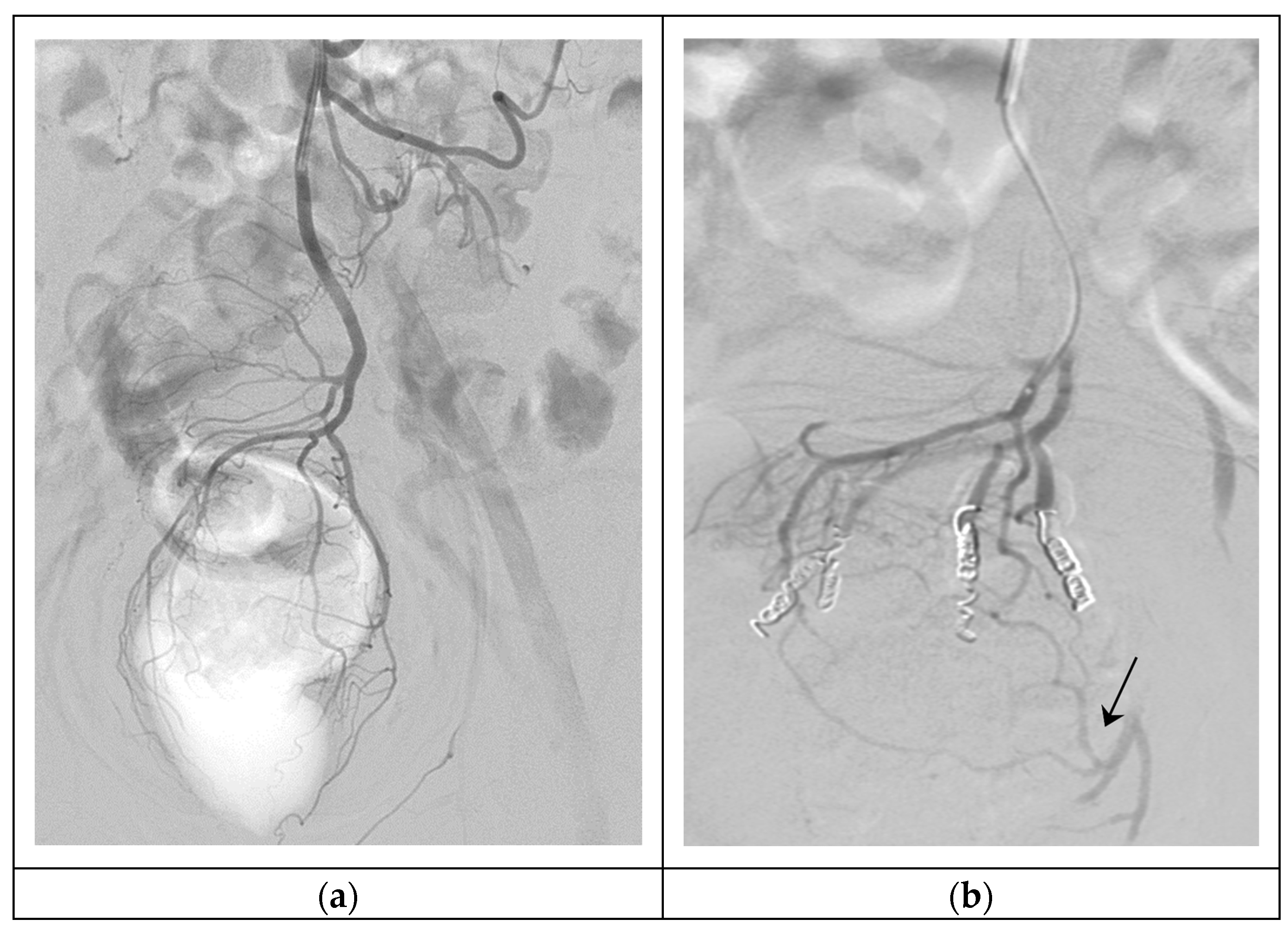
Figure 2. Hemorrhoidal embolization. (a) Arteriography of SRA, showing the vascular anatomy of the hemorrhoidal plexus (type I); (b) Super-selective embolization of four branches of the SRA with 300–500 μm particles and 3 mm 5 cm coils, persistent MRA anastomoses in the left part of the hemorrhoidal plexus (arrow).
Table 4. Comparison between coil embolization vs. particles added to coil embolization.
| Coils Alone | Particles and Coils |
|---|---|
| 2–3 mm coils in SRA branches | Particles injection in the distal part of SRA branches, near the CCR, followed by coils |
| Proximal embolization | Proximal and distal embolization |
| Persistent MRA and IRA anastomoses | Obstruction of MRA and IRA anastomoses |
| Higher recurrence of bleeding, may need a second embolization | Lower recurrence of bleeding |
| Less postprocedural symptoms | Postprocedural rectal pain and tenesmus Asymptomatic and small superficial rectal ulcerations if particles < 900 μm |
It is also possible to use TRA with a 0.018-inch arterial micro-puncture set. It is advisable to puncture the left radial artery to minimize the risk of stroke. To avoid vasospasm, a “radial cocktail” (3000 IU of unfractionated heparin and 200 ugs of nitroglycerin or 2.5 mg of verapamil) is administered. Catheterization of SRA with 110 up to 150 cm-long multipurpose 4 or 5F catheter (Radifocus; Terumo, Tokyo, Japan) is advanced over a 0.035-inch × 260 cm-long glide wire, and then a 150 up to 175 cm-long microcatheter is used as TruSelect® (Boston Scientific; Marlborough, MA, USA).
Patients with TFA are discharged home one day after the intervention, and patients with TRA after 6 h. A comparison of both accesses is made in Table 5 [28][30].
Table 5. Comparison between femoral and radial access.
| TFA | TRA |
|---|---|
| Discharge after 24 h | Discharge on the same day |
| Most common and trained access, more material available | Need for training for most of interventional radiologists, longer procedures, and higher radiation dose (No difference for new specialists) |
| Contraindicated if antiplatelet or anticoagulant therapy or bleeding disorders | Possible if affected INR or level of platelets |
| Access site vascular complications | Lower access site vascular complications |
Patients are clinically followed up between 1 and 12 months. Technical success is considered when all the arterial network is properly embolized (Figure 2), and clinical success is when no rebleeding is observed between the first month and first year after embolization [25][26][27][28][29][30][31][32][33][34].
This entry is adapted from the peer-reviewed paper 10.3390/jcm11226631
References
- Sun, Z.; Migaly, J. Review of hemorrhoid disease: Presentation and management. Clin. Colon. Rectal Surg. 2016, 29, 22–29.
- Kaidar-Person, O.; Person, B.; Wexner, S.D. Hemorrhoidal disease: A comprehensive review. J. Am. Coll. Surg. 2007, 204, 102–117.
- Ganz, R.A. The evaluation and treatment of hemorrhoids: A guide for the gastroenterologist. Clin. Gastroenterol. Hepatol. 2013, 11, 593–603.
- Moussa, N.; Sielezneff, I.; Sapoval, M.; Tradi, F.; Del Giudice, C.; Fathallah, N.; Pellerin, O.; Amouyal, G.; Pereira, H.; de Parades, V.; et al. Embolization of the superior rectal arteries for chronic bleeding due to haemorrhoidal disease. Color. Dis. 2017, 19, 194–199.
- Madoff, R.D.; Fleshman, J.W. American Gastroenterological Association technical review on the diagnosis and treatment of hemorrhoids. Gastroenterology 2004, 126, 1463–1473.
- Van Tol, R.R.; Kleijnen, J.; Watson, A.J.M.; Jongen, J.; Altomare, D.F.; Qvist, N.; Higuero, T.; Muris, J.W.M.; Breukink, S.O. European Society of ColoProctology: Guideline for haemorrhoidal disease. Color. Dis. 2020, 22, 650–662.
- Cengiz, T.B.; Gorgun, E. Hemorrhoids: A range of treatments. Cleve. Clin. J. Med. 2019, 86, 612–620.
- Perera, N.; Liolitsa, D.; Iype, S.; Croxford, A.; Yassin, M.; Lang, P.; Ukaegbu, O.; van Issum, C. Phlebotonics for haemorrhoids. Cochrane Database Syst. Rev. 2012, 8, 1465–1858.
- Milligan, E.T.; Morgan, C.N.; Jones, L.E.; Officer, R. Surgical anatomy of the anal canal and operative treatment of haemorrhoids. Lancet 1937, 119, 1119–1124.
- Longo, A. Treatment of hemorrhoidal disease by reduction of mucosa and hemorrhoidal prolapse with circular stapling device: A new procedure. In Proceedings of the 6th World Congress of Endoscopic Surgery, Rome, Italy, 31 May–6 June 1998; pp. 777–784.
- Senagore, A.J.; Singer, M.; Abearian, H.; Fleshman, J.; Corman, M.; Wexner, S.; Nivatvongs, S. A prospective, randomized, controlled multicenter trial comparing stapled hemorrhoidopexy and Ferguson hemorrhoidectomy: Perioperative and 1-year results. Dis. Colon Rectum. 2004, 47, 1824–1836.
- Ratto, C. THD Doppler procedure for hemorrhoids: The surgical technique. Tech. Coloproctol. 2014, 18, 291–298.
- Elmer, S.E.; Nygren, J.O.; Lenander, C.E. A randomized trial of transanal hemorrhoidal dearterialization with anopexy compared with open hemorrhoidectomy in the treatment of hemorrhoids. Dis. Colon Rectum. 2013, 56, 484–490.
- Salgueiro, P.; Rei, A.; Garrido, M.; Rosa, B.; Oliveira, A.M.; Pereira-Guedes, T.; Morais, S.; Castro-Poças, F. Polidocanol foam sclerotherapy in the treatment of hemorrhoidal disease in patients with bleeding disorders: A multicenter, prospective, cohort study. Tech. Coloproctol. 2022, 26, 615–625.
- Lisi, G.; Gentileschi, P.; Spoletini, D.; Passaro, U.; Orlandi, S.; Campanelli, M. Sclerotherapy for III- and IV-degree hemorrhoids: Results of a prospective study. Front. Surg. 2022, 9, 978574.
- Tutino, R.; Massani, M.; Jospin Kamdem Mambou, L.; Venturelli, P.; Della Valle, I.; Melfa, G.; Micheli, M.; Russo, G.; Scerrino, G.; Bonventre, S.; et al. A Stepwise Proposal for Low-Grade Hemorrhoidal Disease: Injection Sclerotherapy as a First-Line Treatment and Rubber Band Ligation for Persistent Relapses. Front. Surg. 2022, 10, 782800.
- Ratto, C.; Campenni, P.; Papeo, F.; Donisi, L.; Litta, F.; Parello, A. Transanal hemorrhoidal dearterialization (THD) for hemorrhoidal disease: A single-center study on 1000 consecutive cases and a review of the literature. Tech. Coloproctol. 2017, 21, 953–962.
- Brown, S.R.; Tiernan, J.P.; Watson, A.J.; Biggs, K.; Shephard, N.; Wailoo, A.J.; Bradburn, M.; Alshreef, A.; Hind, D. HubBLe Study Team Haemorrhoidal artery ligation versus rubber band ligation for the management of symptomatic seconddegree and third-degree haemorrhoids (HubBLe): A multicentre, openlabel, randomised c ontrolled trial. Lancet 2016, 388, 356–364.
- Pucher, P.H.; Sodergren, M.H.; Lord, A.C.; Darzi, A.; Ziprin, P. Clinical outcome following Doppler-guided haemorrhoidal artery ligation: A systematic review. Color. Dis. 2013, 15, e284–e294.
- Vidal, V.; Louis, G.; Bartoli, J.M.; Sielezneff, I. Embolization of the hemorrhoidal arteries (the emborrhoid technique): A new concept and challenge for interventional radiology. Diagnost. Interv. Imaging 2014, 94, 307–315.
- Zakharchenko, A.; Kaitoukov, Y.; Vinnik, Y.; Tradi, F.; Sapoval, M.; Sielezneff, I.; Galkin, E.; Vidal, V. Safety and efficacy of superior rectal artery embolization with particles and metallic coils for the treatment of hemorrhoids (Emborrhoid technique). Diagnost. Interv. Imaging 2016, 97, 1079–1084.
- Gallo, G.; Martellucci, J.; Sturiale, A.; Clerico, G.; Milito, G.; Marino, F.; Cocorullo, G.; Giordano, P.; Mistrangelo, M.; Trompetto, M. Consensus statement of the Italian society of colorectal surgery (SICCR): Management and treatment of hemorrhoidal disease. Tech. Coloproctol. 2020, 24, 145–164.
- Thomson, W.H.F. The nature of haemorrhoids. Br. J. Surg. 1975, 62, 542–552.
- Rebonato, A.; Maiettini, D.; Patriti, A.; Giurazza, F.; Tipaldi, M.A.; Piacentino, F.; Fontana, F.; Basile, A.; Venturini, M. Hemorrhoids Embolization: State of the Art and Future Directions. J. Clin. Med. 2021, 10, 3537.
- Campennì, P.; Iezzi, R.; Marra, A.A.; Posa, A.; Parello, A.; Litta, F.; De Simone, V.; Ratto, C. The Emborrhoid Technique for Treatment of Bleeding Hemorrhoids in Patients with High Surgical Risk. J. Clin. Med. 2022, 11, 5533.
- Venturini, M.; De Nardi, P.; Marra, P.; Panzeri, M.; Brembilla, G.; Morelli, F.; Melchiorre, F.; De Cobelli, F.; Del Maschio, A. Embolization of superior rectal arteries for transfusion dependent haemorrhoidal bleeding in severely cardiopathic patients: A new field of application of the “emborrhoid” technique. Tech. Coloproctol. 2018, 22, 453–455.
- Moussa, N.; Bonnet, B.; Pereira, H.; Pechmajou, L.; Pellerin, O.; Abed, A.; de Giudice, C.; Dean, C.; Bouda, D.; de Parades, V.; et al. Mid-term results of superior rectal artery and coils for hemorrhoidal embolization with particles bleeding. Cardiovasc. Intervent. Radiol. 2020, 43, 1062–1069.
- Ferrer Puchol, M.D.; Esteban Hernández, E.; Blanco González, F.J.; Ramiro Gandia, R.; Solaz Solaz, J.; Pacheco Usmayo, A. Selective intra-arterial embolisation to treat haemorrhoids. Radiología 2020, 62, 313–319.
- Stecca, T.; Farneti, F.; Balestriero, G.; Barban, M.; Caratozzolo, E.; Zilio, S.; Massani, M. Superior rectal artery embolization for symptomatic grades 2 and 3 hemorrhoidal disease: 6-month follow-up among 43 patients. J. Vasc. Interv. Radiol. 2021, 32, 1348–1357.
- Iezzi, R.; Campenni, P.; Posa, A.; Parello, A.; Rodolfino, E.; Marra, A.A.; Ratto, C.; Manfredi, R. Outpatient Transradial Emborrhoid Technique: A Pilot Study. Cardiovasc. Intervent. Radiol. 2021, 44, 1300–1306.
- Sirakaya, M.; O'Balogun, A.; Kassamali, R.H. Superior Rectal Artery Embolization for Haemorrhoids: What Do We Know So Far? Cardiovasc. Intervent. Radiol. 2021, 44, 675–685.
- Talaie, R.; Torkian, P.; Moghadam, A.D.; Tradi, F.; Vidal, V.; Sapoval, M.; Golzarian, J. Hemorrhoid embolization: A review of current evidences. Diagnost. Interv. Imaging 2022, 3, 3–11.
- Küçükay, M.B.; Küçükay, F. Superior Rectal Artery Embolization with Tris-Acryl Gelatin Microspheres: A Randomized Comparison of Particle Size. J. Vasc. Interv. Radiol. 2021, 32, 819–825.
- Wang, X.; Sheng, Y.; Wang, Z.; Wang, W.; Xia, F.; Zhao, M.; Han, X. Comparison of different embolic particles for superior rectal arterial embolization of chronic hemorrhoidal bleeding: Gelfoam versus microparticle. BMC Gastroenterol. 2021, 21, 465.
This entry is offline, you can click here to edit this entry!
