Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Biotechnology & Applied Microbiology
Transfer of regenerative approaches into clinical practice is limited by strict legal regulation of in vitro expanded cells and risks associated with substantial manipulations. Isolation of cells for the enrichment of bone grafts directly in the Operating Room appears to be a promising solution for the translation of biomedical technologies into clinical practice. These intraoperative approaches could be generally characterized as a joint concept of tissue engineering in situ.
- bone repair
- cell therapy
- in situ
- minimally manipulated cells
1. Introduction
Translation of regenerative medical approaches into routine clinical practice is limited by strict legal regulations of cultured cells. Legal restrictions are intended to protect patients from the risks associated with substantial cell manipulation [1,2,3]. Therefore, tissue-engineered grafts created directly in the operating room (O.R.) with minimal manipulation of cells appear to be extremely promising.
Intraoperative tissue engineering in situ demonstrated its effectiveness in recent clinical studies [4]. Traditionally, the term ‘tissue engineering in situ’ means different approaches to creating grafts that will mature into functionally active tissue inside the recipient’s body using its own regenerative potential [5]. However, we believe that the term ‘tissue engineering in situ’ should be applied to the process of intraoperative creation of tissue-engineered grafts with their implantation during the same surgical procedure. The obvious advantage of in situ tissue-engineered grafts is off-the-shelf availability, while traditional full-cycle tissue engineering requires sufficient time and financial expenses for cell culture in vitro. Importantly, tissue-engineered grafts created during surgical procedures can be enriched with cells isolated intraoperatively with minimal manipulation.
Traditional tissue engineering in situ does not include scaffold enrichment with cells since it requires in vitro culturing [5]. However, existing techniques and devices allow intraoperative cell isolation and cell seeding on scaffolds. The osteoconductive and osteoinductive properties of scaffolds are required for successful bone regeneration. However, the addition of a cellular component to various types of scaffolds can bring additional therapeutic value. Enrichment of scaffolds with intraoperatively isolated cells is an effective tool to create a unique milieu around the graft, enhance its maturation, and stimulate the intrinsic regenerative potential of the recipient’s body. In particular, seeding with bone marrow-derived mononuclear cells can contribute to angiogenesis in the implantation area [6]. Mesenchymal stem cells (MSCs) are one of the most important cell types within mononuclear and stromal vascular fractions. Tissue engineering in situ may benefit from MSCs due to their ability to reduce inflammation and promote angiogenesis. Also, scaffold enrichment with MSCs in situ may be of value due to the MSC potential for osteogenic differentiation. Calcium phosphate-containing scaffolds are shown to promote MSC differentiation into osteoblasts [7]. Notably, MSCs seeded on calcium phosphate-containing scaffolds underwent osteogenic differentiation and formed bone tissue in vivo earlier than embryonic stem cells [8]. Enrichment with stromal vascular fraction cells has also been shown to enhance the effectiveness of osteoinductive scaffolds in a critical-size cranial defect in mice [9].
The understanding of tissue engineering in situ as a process of intraoperative creation of tissue-engineered graft comprises the possibility of scaffold enrichment with intraoperatively isolated minimally manipulated cells (Figure 1). These cells can be isolated intraoperatively from structural and non-structural tissues including bone marrow, adipose tissue, skin, mucous tissue, etc., seeded on the scaffold and implanted in a patient in a one-step procedure [10,11]. In contrast, tissue engineering with cultured cells requires two separate interventions (e.g., bone marrow aspiration/adipose tissue harvesting and surgical implantation of created tissue-engineered graft), authorized manufacturing facilities, and compliance with special regulations for advanced therapy medicinal products [2,12].
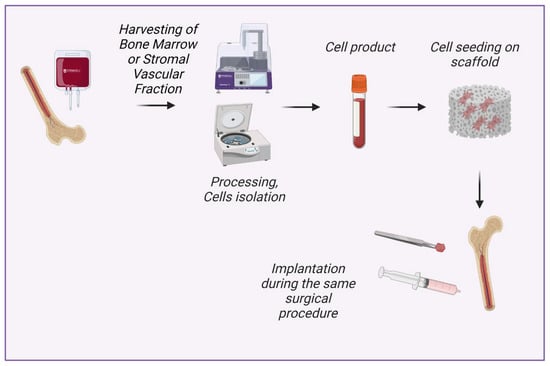
Figure 1. New concept of tissue engineering in situ: intraoperative isolation of cells with minimal manipulation, cell seeding on scaffold and implantation during the same surgical procedure. Created with BioRender.com.
The concept of intraoperative tissue engineering in situ does not contradict traditional tissue engineering in situ since the enrichment of scaffolds with intraoperatively isolated cells may contribute to the stimulation of the recipient’s own regenerative potential [13].
2. Cells Used for Bone Tissue Engineering In Situ
The use of in vitro cultured cells has been shown to enhance bone healing in multiple studies. In particular, it helped to treat non-unions [14,15]. In this section, we will consider cells that have shown their effectiveness for bone regeneration and that can be isolated during a surgical procedure with minimal manipulations.
Cells contained in the bone marrow mononuclear fraction are often used to create tissue-engineered grafts in the operating room, although in some clinical studies scaffolds were enriched with bone marrow aspirate concentrate or with non-concentrated bone marrow aspirate [16,17].
Bone marrow mononuclear cells (BM-MNCs) are widely used in clinical practice alone or in combination with various scaffolds, including bone autografts, hydroxylapatite, β-tricalcium phosphate, etc. Multiple clinical and animal studies demonstrated results in improved bone healing [4,18,19]. Importantly, BM-MNCs are available as minimally-manipulated cells without preliminary cell culture [20]. BM-MNCs are a heterogeneous population of cells with a single nucleus, which includes mesenchymal stromal and stem cells, hematopoietic stem cells, endothelial progenitor cells, very small embryonic-like stem cells, embryonic stem cells, etc. The presence of different cell types in the mononuclear fraction causes combinative effects on regeneration. In particular, endothelial progenitor cells promote vascularization, and mesenchymal stem cells reduce inflammation.
Mesenchymal stem cells (MSCs) as well as mesenchymal stromal cells are components of BM-MNCs and one of the key players in tissue regeneration due to their ability to reduce inflammation, express growth factors, and differentiate into osteoblasts [21]. MSCs represent the population of osteoblasts progenitors in the bone marrow. Interestingly, ultrasound microwave irradiation was used for stimulation of MSCs osteo-differentiation in culture [22]. A combination of various scaffolds and cultured bone marrow-derived MSCs (BM-MSCs) has been used for the treatment of bone fractures or resorption in multiple clinical and animal studies [14,19,23,24]. Importantly, the combination of uncultured BM-MNCs and β-tricalcium phosphate resulted in enhanced bone regeneration and mineralization in vivo compared to MSCs cultured on the same scaffold [19].
For purposes of intraoperative tissue engineering in situ, MSCs can be isolated from other sources besides bone marrow. Intraoperative enrichment with adipose tissue-derived MSCs (AD-MSCs) could be achieved by the adhesion of stromal vascular fraction (SVF) cells to the scaffold. In that case, AD-MSCs will be delivered together with the other SVF components. The reparative success of SVF is also based on contained endothelial progenitor cells, M2-macrophages, smooth muscle cells, preadipocytes, etc. [25,26]. Those cells provide an essential microenvironment for MSCs and regulate their differentiation in an osteogenic direction via cell-to-cell cross-talks [27]. Also, known regenerative effects of SVF cells include improvement of angiogenesis and secretion of extracellular matrix. The chain of effects results in the ability of SVF to mineralize decellularized bone matrix and polycaprolactone and to increase new bone formation in vivo [9,28,29]. An experimental study in vitro showed that bone marrow-derived MSCs have even more osteogenic potential than adipose-derived cells [30]. However, multiple animal studies have shown no statistical difference between BM-MSCs and AD-MSCs in terms of bone regeneration [31,32]. At the same time, cell yield (incl. stem cell yield) is generally higher in adipose tissue than in bone marrow aspirate [33].
One of the promising directions is the isolation of MSCs from gingival tissues [34,35]. Some studies showed that gingiva-derived MSCs had better results in terms of staining for ALP; mineralized nodule formation; and APL, OSX, and RUNX2 gene expression compared to BM-MSCs in mice [36]. Among the advantages of isolating MSCs from the gingiva is minimal surgical intervention, as well as fast scarless healing of the gingival donor site [37]. Enzymatic treatment of gingival tissue takes around 2 h allowing the scaffold to be intraoperatively enriched with resulting suspension that contains gingiva-derived MSCs [37].
Sufficient vascularization is crucial for the regeneration of bone defects [38]. Endothelial progenitor cells (EPCs) have been shown to enhance vascularization in several studies [39,40]. EPC is included in the mononuclear fraction of bone marrow and also are found in SVF and peripheral blood.
3. Materials for Bone Tissue Engineering In Situ
The type of implantable materials is a key factor in maintaining the shape and mechanical properties of the bone graft after implantation [41]. All materials for bone tissue engineering are mainly divided into non-resorbable (e.g., ceramic and polymeric grafts) and bioresorbable materials [42,43,44]. Various osteoinductive materials, such as beta-tricalcium phosphate (β-TCP) [45], hydroxyapatite [46], and xenografts [47] are commonly used as scaffolds in preclinical studies and clinical cases due to their commercial availability. Recent evidence also suggested bioactive glass ceramics as a suitable material for bone tissue engineering, it being capable of the promotion of osteogenesis [48].
Notably, hydroxyapatite can also be in a resorbable form. The effectiveness of resorbable high-porous acellular hydroxyapatite scaffolds is generally based on the enhanced local regenerative potential [49,50]. Resorbable scaffolds could be a suitable solution for cartilage and bone tissue engineering [51,52,53]. While the mobilization of patients’ own osteoblasts leads to the revitalization of the graft, the scaffold could be completely replaced by a newly formed extracellular matrix.
Despite numerous types of scaffolds, bone graft autotransplantation is still considered a ‘gold-standard’ approach to repairing bone defects (Figure 2a). However, a well-known method of autologous osteoplasty is commonly limited by the harvested bone volume and associated with an additional risk of complications in the donor site [20,54].
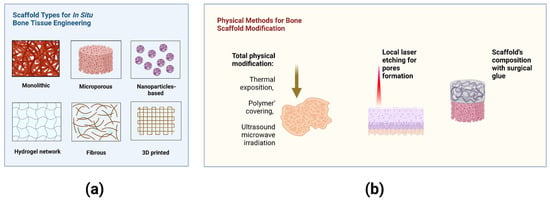
Figure 2. (a) Scaffold types for bone tissue engineering in situ. (b) Methods for physical modification of scaffolds immediately in the Operating Room. Created with BioRender.com.
The material-related complications remain to pose a sufficient risk due to individual response after implantation [55,56]. Insufficient vascularization and inflammatory response are often observed in the bone regeneration zone [57]. Bone tissue engineering in situ through BM-MSCs osteogenic differentiation may be performed using immobilized gene delivery nanocomplexes [58]. Bioactive scaffolds with modified surface properties or gene-activated materials have promising applications as scaffolds for cell seeding [59,60].
Promising physical approaches allow the modification of biomaterials and cells immediately in the Operating Room (O.R.). Laser engraving of cartilage led to improved deep chondrocyte migration into the scaffold after implantation [52,61]. The nonselective damaged cartilage also stimulated cell migration via cell secretion activity [62,63]. The methods for modification of bone scaffolds and their properties are summarized in Figure 2b.
Various materials are used in bone tissue engineering, and, notably, the adhesion capacity of BM-MNCs differs depending on the type of material. Henrich et al. (2015) showed that coating of β-TCP with fibronectin and human plasma does not increase the adhesion capacity of human BM-MNCs isolated by density gradient centrifugation, at the same time the percentage of attached cells was higher in β-TCP and demineralized bone matrix compared to bovine cancellous bone [64]. The comparative effectiveness of implantation of various materials for the treatment of large bone defects in rats showed that the fibrous demineralized bone matrix seeded with centrifugation-isolated BM-MNCs led to promising results in comparison with syngeneic cancellous bone implantation [65]. Centrifugation-isolated BM-MNCs were seeded on human demineralized bone matrix, bovine cancellous bone hydroxyapatite ceramic, and β-tricalcium phosphate scaffolds. The study showed that the effectiveness of BMC-supported therapy could be influenced by the type of scaffold. Although the demineralized bone matrix was superior in comparison to β-tricalcium phosphate and bovine cancellous bone hydroxyapatite ceramic, the level of autologous bone could not be attained [66].
This entry is adapted from the peer-reviewed paper 10.3390/bioengineering9110704
This entry is offline, you can click here to edit this entry!
