Pituitary pars intermedia dysfunction is one of the most common endocrinopathies in horses; however, the pathophysiology of PPID is incompletely understood [
33,
34,
35,
36,
37,
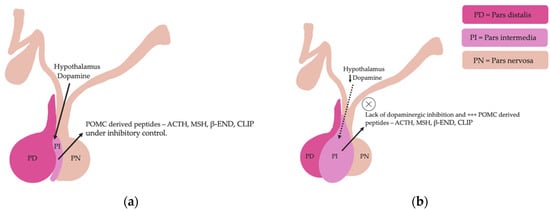
38]. The disease is caused by loss of dopaminergic inhibition of the pituitary PI due to oxidative-stress and subsequent neurodegeneration of dopaminergic neurons within the hypothalamus [
17,
39]. This theory was confirmed recently in a study that aimed to determine whether it was decreased dopamine or dopamine D2 receptor dysfunction that led to PPID. Tyrosine hydroxylase is a biomarker of dopaminergic neurons, and this retrospective study used 28 horses with PPID to measure tyrosine hydroxylase expression within the pars intermedia. A negative correlation between pituitary histomorphological grades and tyrosine hydroxylase was observed, confirming the involvement of reduced dopamine in the pathogenesis of PPID [
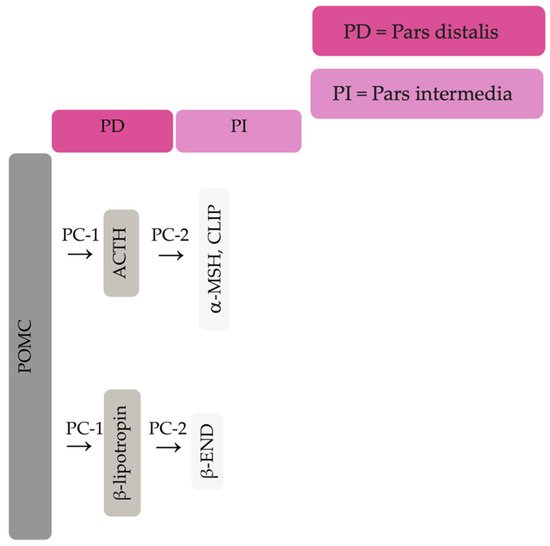
38]. The loss of dopaminergic inhibition on the melanotropes of the pars intermedia results in hyperplasia, microadenoma or macroadenoma formation and overproduction of POMC derived peptides including ACTH and α-MSH (
Figure 2) [
16]. The ACTH secreted by the PI of horses with PPID is largely biologically inactive [
17,
40,
41]. Subsequently, increased plasma ACTH concentrations do not result in adrenal stimulation and hypercortisolaemia [
16,
17,
42,
43,
44]. Horses with PPID have resting serum concentrations of free thyroxine and TSH that are lower than age-matched control horses, with normal TSH responses to exogenous TRH administration [
24]. Because glucocorticoids exert an inhibitory action on the hypothalamic-pituitary-thyroid axis [
24,
25], it has been hypothesized that increased glucocorticoid activity does exist, with prolonged tonic suppression of TRH [
24].
4. Diagnosis
A presumptive diagnosis of PPID can be made based on the presence of hypertrichosis in aged horses [
108,
109,
110,
111,
112]. Laboratory testing is recommended in cases where treatment is financially feasible, where early or severe clinical disease is suspected [
54], or to determine the response to treatment [
54]. Currently, testing horses for subclinical PPID is not recommended [
54]. However, the disease can have severe, life threatening consequences and ability to diagnose subclinical or mild PPID and initiate treatment before end-stage disease may be beneficial [
40,
47,
113]. A recent prospective case series measured basal and TRH-stimulated ACTH concentrations in seven horses with subclinical PPID, and found that TRH-stimulation testing in late summer or early autumn (February and March in Australia) identified most horses that transitioned to clinical PPID over a 3.5 year period [
113]. This was a small case series, so further research is required to determine if early diagnosis is warranted. Currently, there is no ante-mortem diagnostic test that can be completely relied upon for an accurate diagnosis of PPID [
31,
32]. Post-mortem evaluation of pituitary glands via histopathology has been used to confirm laboratory test results [
111]. A grading system was created to determine the severity of pituitary pars intermedia histological changes [
114], and the grade has been shown to correlate with laboratory results and clinical signs [
114,
115]. However, histopathology remains a subjective test, and concordance between pathologists is only moderate [
116]. Pituitary size and histomorphology are also affected by season [
115] and age [
117] making the use of histopathology in diagnosis of PPID challenging [
40]. Results of tests in horses that are affected by early or subclinical disease, are often equivocal [
113]. Untreated PPID cases due to false-negative test results can lead to morbidity through muscle wastage, opportunistic infections, and difficulty thermoregulating. False positive test results may lead to unnecessary treatment. This is not only a financial burden, but the risks associated with long-term treatment with pergolide have not been established [
2,
118]. It is imperative that diagnostic tests be interpreted with care to reduce the incidence of false positive and false negative results [
32].
Current recommendations for diagnosis of PPID are to measure the basal ACTH concentration in horses with obvious clinical signs, utilising seasonally adjusted diagnostic thresholds and an equivocal zone [
54]. For the diagnosis of early disease, measurement of TRH-stimulated ACTH concentrations is recommended [
2,
54]. When finances or availability of laboratory testing of ACTH concentrations are not available, response to therapy with pergolide mesylate may be used as a more practical approach to diagnosing PPID in aged horses with generalised hypertrichosis [
54]. Other diagnostic techniques include measurement of endogenous α-MSH and the now superseded overnight dexamethasone suppression test. Measurement of endogenous α-MSH, it is not commercially available and did not perform as well as basal ACTH [
28,
31,
119]. Seasonally adjusted DCOV are yet to be established for the overnight dexamethasone suppression test. Although not discussed in this review, additional diagnostic testing for hyperinsulinemia is recommended for horses with regional adiposity and/or a history of laminitis, as management practices are altered in these horses [
120].
4.1. Basal ACTH
Basal ACTH is the most popular and common test used for diagnosis of PPID as it is easy to perform and requires only a single blood measurement [
121]. Interpretation of results must take into consideration stress, illness, pain, season, age, sex, and body condition score, as all these factors can increase concentrations of ACTH [
30]. Breed differences in ACTH concentration have been observed with a greater and prolonged peak in ACTH concentrations in late summer and autumn in Shetland and Welsh ponies compared to Warmbloods, Thoroughbreds and Cob breeds. These differences were not observed outside of late summer and autumn. Arabians and donkeys had ACTH concentrations greater than other breeds for a more prolonged period from May to November [
122,
123]. These differences in ACTH concentration do not appear to have led to overrepresentation of these breeds in diagnosis of PPID [
3]. The test can be performed at any time of day [
124,
125]. Performing paired measurement of ACTH has no benefit to performing a single measurement [
125]. If these results are equivocal, a TRH stimulation test should be performed due to the greater accuracy of this test [
2,
40].
The blood sample should be collected in an EDTA tube, centrifuged, kept at 4 °C and analysed as soon as possible after sampling, ideally within 24 h [
126,
127]. If the sample cannot be tested immediately, the centrifuged plasma should be frozen as heat results in degradation of ACTH [
128]. Multiple freeze-thaw cycles should be avoided as this will alter the ACTH concentration [
129].
In all horses, basal ACTH follows a circannual rhythm that demonstrates a peak in concentration in the autumn months. Basal ACTH was thought to be the most sensitive and specific diagnostic test in the autumn due to increased magnitude of differences in ACTH concentrations between affected and unaffected horses [
31]. However, more recent literature has demonstrated the accuracy of basal ACTH is reduced in March (September in the Northern hemisphere). Basal ACTH concentration still had good accuracy for diagnosis of PPID in March (accuracy 0.8–0.9), but accuracy was improved to excellent (accuracy > 0.9) in April and May [
2]. Meta-analyses and systematic reviews have been performed to establish the sensitivity and specificity of basal ACTH. Although not broken down by season, the median sensitivity and specificity of basal ACTH in one study were 75.5% and 95.2% respectively [
36], while another study reported the mean sensitivity and specificity at 66% and 87% respectively [
130]. Based on these results, basal ACTH is excellent for ruling out PPID, and less accurate for detecting the condition unless the horse has severe clinical signs. As such, basal ACTH is not recommended for screening purposes or use in horses with early disease [
130]. However, both studies identified biases, between-study variations and suboptimal study designs and populations. Less biased studies examining the diagnostic accuracy of basal ACTH are required to accurately establish sensitivity and specificity.
Monthly reference intervals (RI) and DCOV for the interpretation of ACTH results were established in a study of 106 mature horses. In this study DCOV were recommended to improve the detection of early PPID, and RI were recommended to reduce the likelihood of false positives [
2]. This study proposed that determination of basal ACTH concentrations is accurate for diagnosis of PPID in horses, providing these DCOV and RI are used, and the results are interpreted within the clinical context. The TRH stimulation test may improve the accuracy of diagnosis of PPID irrespective of season [
2]. Another recent retrospective study using a population of 75,892 horses used an indirect approach to calculate diagnostic thresholds. This study similarly proposed that diagnostic thresholds should be used alongside clinical judgement, and the appropriate threshold should be chosen when there is a reason to avoid false positive or false negative results [
32]. This study established diagnostic thresholds using intervals as short as one week. Inter-weekly variability was low for most of the year, with a nadir in June to December (northern hemisphere) [
32]. The Equine Endocrinology Group recommends using seasonal thresholds with equivocal zones for interpretation of results. Prior to recommending treatment for horses without strong clinical signs that have basal ACTH results that fall within equivocal zones, re-testing or use of a TRH stimulation test is recommended [
54].
4.2. Thyrotropin-Releasing Hormone (TRH) Stimulation Test
In early PPID or when clinical signs are mild, the TRH stimulation test is useful for increased accuracy of diagnosis [
1,
2,
40,
113,
121]. Plasma ACTH is measured before and either 10 or 30 min after administration of 1 mg TRH IV (0.5 mg for ponies). Thyrotropin-releasing hormone increases ACTH and α-MSH concentrations in plasma through stimulation of TRH R1 receptors on the pituitary pars intermedia and pars distalis [
1,
21,
40,
119,
131]. Thyrotropin-releasing hormone stimulation in normal horses results in POMC derived peptide secretion by the pars distalis that is restricted by glucocorticoid negative feedback. In horses with PPID, TRH stimulation results in POMC-derived peptide secretion by the melanotrophs of the pars intermedia, and excessive ACTH secretion by hyperplastic or neoplastic melanotrophs that is unaffected by a negative feedback loop, resulting in a dramatic increase in ACTH concentration [
1,
2,
21,
26]. As with basal ACTH, the TRH stimulation test should be interpreted in accordance with seasonally adjusted DCOV to improve diagnostic accuracy [
2,
54]. Several investigators recommend not using the TRH stimulation test in the autumn [
40,
42,
54], and repeatability of the test in autumn appears to be reduced [
132]. However, recent studies have found that while variation in ACTH concentrations are greater in autumn, it should not impact diagnostic accuracy providing DCOV and RI are used [
2,
133]. The disparity in results could be due to the difference in ages of the populations investigated, as well as sample sizes.
The TRH stimulation test has been associated with side effects such as yawning, muscle fasciculation, transient coughing, lip-smacking and the flehmen response, but appears safe. The test is applicable for both hospital and ambulatory practice [
40]. Measuring ACTH concentration 10-min post TRH administration is favoured by ambulatory practitioners for time efficiency, hence its recommendation by the Equine Endocrinology Group (EEG) [
54]. However, as there is a much larger variation in the ACTH concentration 1 min pre and post the 10 min time point [
40,
42,
131,
134], compared to 1 min pre and post the 30 min time point [
2,
132] (where the ACTH response curve is flatter), some researchers favour using the 30 min time point due to greater accuracy when repeated samples are required [
134]. Further research is required to determine the variability of ACTH concentrations 30 min post TRH administration [
134]. Prior to the availability of a compounded product in the USA, most research papers utilise the chemical grade TRH (Sigma-Aldrich Pty Ltd. (subsidiary of Merck), North Ryde BC, Australia or synthetic thyrotropin releasing hormone, Sigma-Aldrich Inc, St. Louis, MO, USA) [
2,
121,
124,
127,
129,
132]. Although TRH is now available as a compounded product in the USA, in Europe and Australia TRH is not available as a sterile registered product, and use tends to be limited to referral hospitals [
132,
133,
134]. In the UK and most of Europe, the use of unlicenced chemicals is restricted, limiting the use of TRH for the diagnosis of PPID.
4.3. Dexamethasone Suppression Test
The dexamethasone suppression test for detection of PPID requires two consecutive visits making it a less popular option. It is also less valuable in the identification of early disease, and administration of dexamethasone has been associated with negative consequences such as laminitis [
135,
136]. Serum cortisol concentration is measured before and 18–20 h after administration of 0.04 mg/kg dexamethasone IM [
28,
137,
138]. In normal horses, administration of dexamethasone results in negative feedback on the corticotropes of the pars distalis, suppressed ACTH secretion and a reduction in plasma cortisol concentration. However, in horses with PPID, cortisol secretion is maintained as the melanotropes of the pars intermedia continue to secrete large quantities of ACTH [
1]. Results of the dexamethasone suppression test are frequently inconsistent with TRH stimulation test results [
40]. There is also some evidence to suggest that season influences the result of the dexamethasone suppression test, with false positives more likely in the autumn months [
27,
139]. The dexamethasone suppression test is no longer recommended if laboratory measurement of ACTH concentration is available.
4.4. Plasma α-MSH
Unlike ACTH, α-MSH is a direct product of the pars intermedia [
21]. In horses with PPID, the hyperplastic pars intermedia secretes α-MSH in quantities in excess of ACTH production [
21,
119,
131], indicating that α-MSH may increase earlier in the disease process [
5,
51]. Measuring α-MSH has shown to have improved diagnostic accuracy than basal ACTH and may be more useful in detecting early disease [
21,
28,
51,
119,
131]. α-MSH has a higher specificity and sensitivity than ACTH in the autumn months, and specificity is also greater than that of basal ACTH in the non-autumn months, but the sensitivity reduces [
31]. Measurement of α-MSH has been identified as a test that could be useful in the diagnosis of PPID, as unlike ACTH, α-MSH is not known to be confounded by variables such as stress, transportation, exercise and pain [
2,
21]. Similar to ACTH, α-MSH concentration is influenced by season and is highest in the autumn months [
21,
28,
51,
119]. Seasonally adjusted DCOV for basal α-MSH were established using the Youden index and compared to ACTH DCOV, and found that α-MSH and ACTH were highly correlated [
31]. α-MSH is not as stable as ACTH in chilled whole blood, remaining stable for 8 h prior to centrifugation, plasma separation and freezing [
51]. Therefore, its use may be restricted in ambulatory practice. Laboratory measurement of α-MSH is not commercially available. Some research has been established investigating α-MSH response to TRH administration, but it is not any more useful than measuring ACTH after TRH administration [
131]. Increases in α-MSH in response to TRH were substantially greater than ACTH in the autumn months [
21,
119], which may complicate the use of the test unless seasonally adjusted DCOVs are established. However, this may also prove to be a valuable diagnostic test if interpreted correctly [
119].
4.5. Imaging
Computed tomography (CT) [
107] and more recently, magnetic resonance imaging (MRI) [
140] have been used to evaluate the equine pituitary gland, and both modalities appear to provide adequate detail [
107,
140]. Because no laboratory test for PPID can be completely relied upon, imaging may be useful for earlier detection of the disease [
140]. Imaging may also be useful to assess pituitary size, surrounding structures, and obtain a more accurate prognosis [
141]. The use of imaging modalities is limited at this stage due to expense and accessibility, but may become a suitable diagnostic technique in the future [
107].