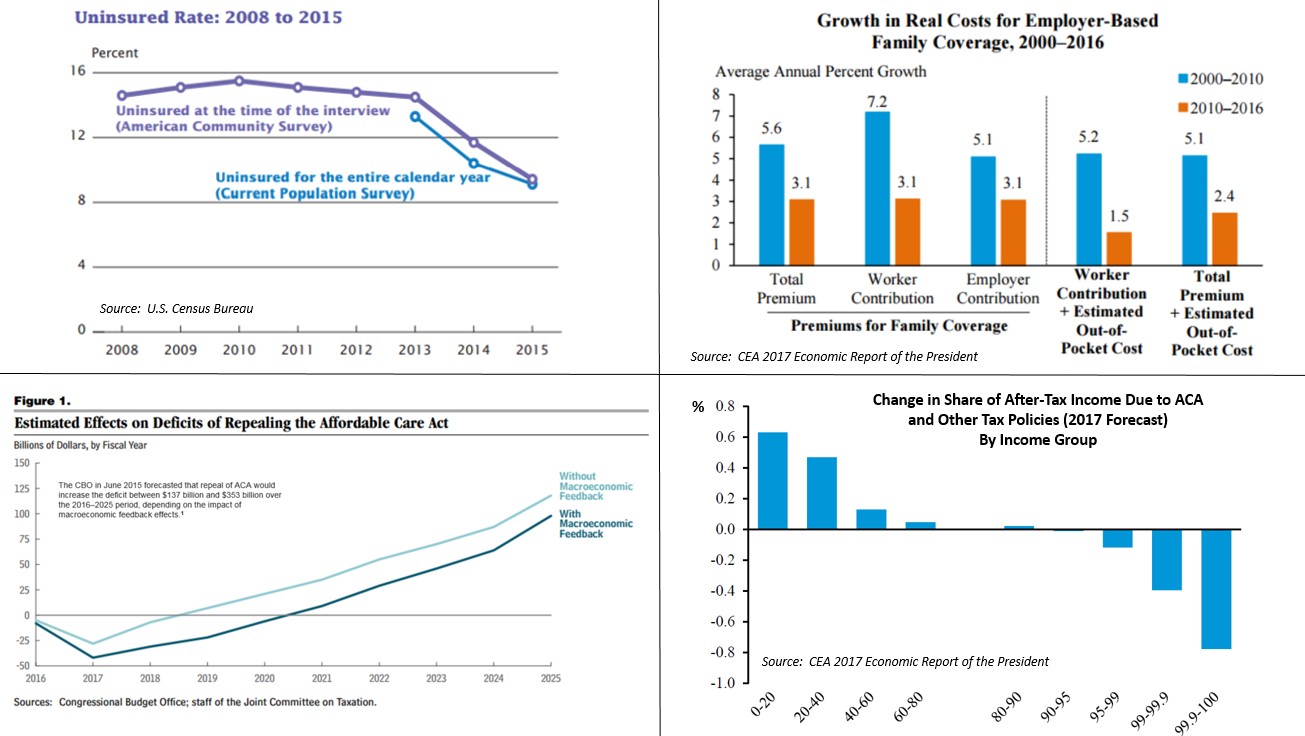
The Patient Protection and Affordable Care Act, also known as the Affordable Care Act (ACA) or colloquially as Obamacare, is a United States federal statute enacted by the 111th United States Congress and signed into law by President Barack Obama on March 23, 2010. Together with the Health Care and Education Reconciliation Act of 2010 amendment, it represents the U.S. healthcare system's most significant regulatory overhaul and expansion of coverage since the passage of Medicare and Medicaid in 1965. PPACA's major provisions came into force in 2014. By 2016, the uninsured share of the population had roughly halved, with estimates ranging from 20 to 24 million additional people covered. The law also enacted a host of delivery system reforms intended to constrain healthcare costs and improve quality. After the law went into effect, increases in overall healthcare spending slowed, including premiums for employer-based insurance plans. The increased coverage was due, roughly equally, to an expansion of Medicaid eligibility and to changes to individual insurance markets. Both received new spending, funded through a combination of new taxes and cuts to Medicare provider rates and Medicare Advantage. Several Congressional Budget Office reports said that overall these provisions reduced the budget deficit, that repealing PPACA would increase the deficit, and that the law reduced income inequality by taxing primarily the top 1% to fund roughly $600 in benefits on average to families in the bottom 40% of the income distribution. The act largely retained the existing structure of Medicare, Medicaid and the employer market, but individual markets were radically overhauled. Insurers were made to accept all applicants without charging based on pre-existing conditions or demographic status (except age). To combat the resultant adverse selection, the act mandated that individuals buy insurance (or pay a fine/tax) and that insurers cover a list of "essential health benefits". Before and after enactment PPACA faced strong political opposition, calls for repeal and legal challenges. In National Federation of Independent Business v. Sebelius, the Supreme Court ruled that states could choose not to participate in PPACA's Medicaid expansion, although it upheld the law as a whole. The federal health exchange, HealthCare.gov, faced major technical problems at the beginning of its rollout in 2013. Polls initially found that a plurality of Americans opposed the act, although its individual provisions were generally more popular and the law gained majority support by 2017.
- healthcare spending
- healthcare costs
- quality
1. Specific Provisions


PPACA amended the Public Health Service Act of 1944 and inserted new provisions on affordable care into Title 42 of the United States Code.[1][2][3][4][5] The individual insurance market was radically overhauled, and many of the law's regulations applied specifically to this market,[1] while the structure of Medicare, Medicaid, and the employer market were largely retained.[2] Some regulations applied to the employer market, and the law also made delivery system changes that affected most of the health care system.[2]
1.1. Insurance Regulations: Individual Policies
All new individual major medical health insurance policies sold to individuals and families faced new requirements.[6] The requirements took effect on January 1, 2014. They include:
- Guaranteed issue prohibits insurers from denying coverage to individuals due to pre-existing conditions.
- States were required to ensure the availability of insurance for individual children who did not have coverage via their families.
- A partial community rating allows premiums to vary only by age and location, regardless of preexisting conditions. Premiums for older applicants can be no more than three times those for the youngest.[7]
- Essential health benefits must be provided. The National Academy of Medicine defines the law's "essential health benefits" as "ambulatory patient services; emergency services; hospitalization; maternity and newborn care; mental health and substance use disorder services, including behavioral health treatment; prescription drugs; rehabilitative and habilitative services and devices; laboratory services; preventive and wellness services and chronic disease management; and pediatric services, including oral and vision care"[8][9] and others[10] rated Level A or B[11] by the U.S. Preventive Services Task Force.[12] In determining essential benefits, the law required that standard benefits should offer at least that of a "typical employer plan".[13] States may require additional services.[14]
- Preventive care and screenings for women.[15] "[A]ll Food and Drug Administration approved contraceptive methods, sterilization procedures, and patient education and counseling for all women with reproductive capacity".[16] This mandate applies to all employers and educational institutions except for religious organizations.[17][18] These regulations were included on the recommendations of the Institute of Medicine.[19][20]
- Annual and lifetime coverage caps on essential benefits were banned.[21][22]
- Insurers are forbidden from dropping policyholders when they become ill.[23]
- All policies must provide an annual maximum out of pocket (MOOP) payment cap for an individual's or family's medical expenses (excluding premiums). After the MOOP payment is reached, all remaining costs must be paid by the insurer.[24]
- Preventive care, vaccinations and medical screenings cannot be subject to co-payments, co-insurance or deductibles.[25][26][27] Specific examples of covered services include: mammograms and colonoscopies, wellness visits, gestational diabetes screening, HPV testing, STI counseling, HIV screening and counseling, contraceptive methods, breastfeeding support/supplies and domestic violence screening and counseling.[28]
- The law established four tiers of coverage: bronze, silver, gold and platinum. All categories offer the essential health benefits. The categories vary in their division of premiums and out-of-pocket costs: bronze plans have the lowest monthly premiums and highest out-of-pocket costs, while platinum plans are the reverse.[13][29] The percentages of health care costs that plans are expected to cover through premiums (as opposed to out-of-pocket costs) are, on average: 60% (bronze), 70% (silver), 80% (gold), and 90% (platinum).[30]
- Insurers are required to implement an appeals process for coverage determination and claims on all new plans.[23]
- Insurers must spend at least 80–85% of premium dollars on health costs; rebates must be issued if this is violated.[31][32]
1.2. Individual Mandate
The individual mandate[33] required everyone to have insurance or pay a penalty. The mandate and limits on open enrollment[34][35] were designed to avoid the insurance death spiral, minimize the free rider problem and prevent the healthcare system from succumbing to adverse selection.
The mandate was intended to increase the size and diversity of the insured population, including more young and healthy participants to broaden the risk pool, spreading costs.[36]
Among the groups who were not subject to the individual mandate are:
- Illegal immigrants, estimated at around 8 million—or roughly a third of the 23 million projection—are ineligible for insurance subsidies and Medicaid.[37][38] They remain eligible for emergency services.
- Medicaid-eligible citizens not enrolled in Medicaid.[39]
- Citizens whose insurance coverage would cost more than 8% of household income and are exempt from the penalty.[39]
- Citizens who live in states that opt out of Medicaid expansion and who qualify for neither existing Medicaid coverage nor subsidized coverage.[40]
The Tax Cuts and Jobs Act of 2017,[41] reduced to 0 the fine/tax for violating the individual mandate, starting in 2019.[42]
1.3. Premium Subsidies
Individuals whose household incomes are between 100% and 400% of the federal poverty level (FPL) are eligible to receive federal subsidies applied towards premiums for policies purchased via a PPACA exchange, provided they are not eligible for Medicare, Medicaid, the Children's Health Insurance Program, or other forms of public assistance health coverage, and provided they do not have access to affordable coverage (no more than 9.86% of income for the employee's coverage) through their own or a family member's employer.[43][44][45] Households below the federal poverty level are not eligible to receive these subsidies. Lawfully present immigrants whose household income is below 100% FPL and are not otherwise eligible for Medicaid are eligible for subsidies if they meet all other eligibility requirements.[43]) Married individuals must file taxes jointly in order to receive subsidies. Enrollees must have U.S. citizenship or proof of legal residency to obtain a subsidy.
The subsidies for an PPACA plan purchased on an exchange stop at 400% of the Federal Poverty Level (FPL). According to the Kaiser Foundation, this results in a sharp "discontinuity of treatment" at 400% FPL, which is sometimes called the "subsidy cliff".[46] After-subsidy premiums for the second lowest cost silver plan (SCLSP) just below the cliff are 9.86% of income in 2019.[47]
Subsidies are provided as an advanceable, refundable tax credit.[48][49]
The amount of subsidy is sufficient to reduce the premium for the second lowest cost silver plan (SCLSP) on an exchange cost a sliding-scale percentage of income. The percentage is based on the percent of Federal Poverty Level (FPL) for the household, and varies slightly from year to year. In 2019, it ranged from 2.08% of income (100%-133% FPL) to 9.86% of income (300%-400% FPL).[45] The subsidy can be used towards any plan available on the exchange, but not catastrophic plans. The subsidy may not exceed the premium for the purchased plan.
(In this section, the term "income" refers to Modified Adjusted Gross Income.[43][50])
Small businesses are eligible for a tax credit provided they enroll in the SHOP Marketplace.[51]
| Income % of federal poverty level | Premium Cap as a Share of Income | Incomea | Maximumb Annual Net Premium After Subsidy
(Second Lowest Cost Silver Plan) |
Out-of-pocket Max |
|---|---|---|---|---|
| 133% | 3.11% of income | $33,383 | $1,038 | $5,200 |
| 150% | 4.15% of income | $37,650 | $1,562 | $5,200 |
| 200% | 6.54% of income | $50,200 | $3,283 | $5,200 |
| 250% | 8.36% of income | $62,750 | $5,246 | $12,600 |
| 300% | 9.86% of income | $75,300 | $7,425 | $15,800 |
| 400% | 9.86% of income | $100,400 | $9,899 | $15,800 |
|
a.^ In 2019, the Federal Poverty Level was $25,100 for family of four (outside of Alaska and Hawaii). b.^ If the premium for the second lowest cost silver plan (SLCSP) is greater than the amount in this column, the amount of the premium subsidy will be such that it brings the net cost of the SCLSP down to the amount in this column. Otherwise, there will be no subsidy, and the SLCSP premium will (of course) be no more than (usually less than) the amount in this column. Note: The numbers in the table do not apply for Alaska and Hawaii. |
||||
1.4. Exchanges
PPACA mandated that health insurance exchanges be provided for each state. The exchanges are regulated, largely online marketplaces, administered by either federal or state governments, where individuals, families and small businesses can purchase private insurance plans.[52][53][54] Exchanges first offered insurance for 2014. Some exchanges also provide access to Medicaid.[55][56]
States that set up their own exchanges gives them some discretion on standards and prices.[57][58] For example, states approve plans for sale, and thereby influence (through negotiations) prices. They can impose additional coverage requirements—such as abortion.[59] Alternatively, states can make the federal government responsible for operating their exchanges.[57]
1.5. Cost-Sharing Reduction Subsidies
As written PPACA mandated that insurers reduce copayments and deductibles for PPACA exchange enrollees earning less than 250% of the FPL. Medicaid recipients were not eligible for the reductions.
So-called cost-sharing reduction (CSR) subsidies were to be paid to insurance companies to fund the reductions. During 2017, approximately $7 billion in CSR subsidies were to be paid, versus $34 billion for premium tax credits.[60]
The latter were defined as mandatory spending that does not require an annual Congressional appropriation. CSR payments were not explicitly defined as mandatory. This led to litigation and disruption later.
1.6. Risk Management
PPACA implemented multiple approaches to helping mitigate the disruptions to insurers that came with its many changes.
Risk corridors
The risk-corridor program was a temporary risk management device.[61]:1 It was intended to encourage reluctant insurers into PPACA insurance market from 2014–2016. For those years the Department of Health and Human Services (DHHS) Loss-making insurers would receive payments paid for in part by profit-making insurers.[62][63][attribution needed] Similar risk corridors had been established for the Medicare prescription drug benefit.[64]
Many insurers initially offered exchange plans. However, the program did not pay for itself as planned, losing up to $8.3 billion for 2014 and 2015. Authorization had to be given so DHHS could pay insurers from "general government revenues".[attribution needed] However, the Consolidated Appropriations Act, 2014 (H.R. 3547) stated that no funds "could be used for risk-corridor payments".[65][attribution needed] leaving the government in a potential breach of contract with insurers who offered qualified health plans.[66][66]
Several insurers sued the government at the United States Court of Federal Claims to recover the funds believed owed to them under the Risk Corridors program. While several were summarily closed, in the case of Moda Health v the United States, Moda Health won a $214-million judgment in February 2017. Federal Claims judge Thomas C. Wheeler stated, "the Government made a promise in the risk corridors program that it has yet to fulfill. Today, the court directs the Government to fulfill that promise. After all, to say to [Moda], 'The joke is on you. You shouldn't have trusted us,' is hardly worthy of our great government."[67] Moda Health's case was appealed by the government to the United States Court of Appeals for the Federal Circuit along with the appeals of the other insurers; here, the Federal Circuit reversed the Moda Health ruling and ruled across all the cases in favor of the government, that the appropriations riders ceded the government from paying out remain money due to the insurers. The Supreme Court reversed this ruling in the consolidated case, Maine Community Health Options v. United States, reaffirming as with Judge Wheeler that the government had a responsibility to pay those funds under the ACA and the use of riders to de-obligate its from those payments was illegal.[68]
Reinsurance
The temporary reinsurance program is meant to stabilize premiums by reducing the incentive for insurers to raise premiums due to concerns about higher-risk people enrollees. Reinsurance was based on retrospective costs rather than prospective risk evaluations. Reinsurance was available from 2014 through 2016.[69]
Risk adjustment
Risk adjustment involves transferring funds from plans with lower-risk enrollees to plans with higher-risk enrollees. It was intended to encourage insurers to compete based on value and efficiency rather than by attracting healthier enrollees. Of the three risk management programs, only risk adjustment was permanent. Plans with low actuarial risk compensate plans with high actuarial risk.[69]
1.7. Medicaid Expansion
PPACA revised and expanded Medicaid eligibility starting in 2014. All U.S. citizens and legal residents with income up to 133% of the poverty line, including adults without dependent children, would qualify for coverage in any state that participated in the Medicaid program. The federal government was to pay 100% of the increased cost in 2014, 2015 and 2016; 95% in 2017, 94% in 2018, 93% in 2019, and 90% in 2020 and all subsequent years.[70][71][72] A 5% "income disregard" made the effective income eligibility limit for Medicaid 138% of the poverty level.[73] However, the Supreme Court ruled in NFIB v. Sebelius that this provision of PPACA was coercive, and that states could choose to continue at pre-PPACA eligibility levels.
1.8. Medicare Savings
Medicare reimbursements were reduced to insurers and drug companies for private Medicare Advantage policies that the Government Accountability Office and Medicare Payment Advisory Commission found to be excessively costly relative to standard Medicare;[74][75] and to hospitals that failed standards of efficiency and care.[74]
1.9. Taxes
Medicare taxes
Income from self-employment and wages of single individuals in excess of $200,000 annually are subjected to an additional tax of 0.9%. The threshold amount is $250,000 for a married couple filing jointly (threshold applies to their total compensation), or $125,000 for a married person filing separately.[76]
In PPACA's companion legislation, the Health Care and Education Reconciliation Act of 2010, an additional tax of 3.8% was applied to unearned income, specifically the lesser of net investment income and the amount by which adjusted gross income exceeds the above income limits.[77]
Excise taxes
PPACA includes an excise tax of 40% ("Cadillac tax") on total employer premium spending in excess of specified dollar amounts (initially $10,200 for single coverage and $27,500 for family coverage[78]) indexed to inflation. This tax was originally scheduled to take effect in 2018, but was delayed until 2020 by the Consolidated Appropriations Act, 2016. Excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs. An excise tax of 2.3% on medical devices and a 10% excise tax on indoor tanning services were applied as well.[79]
1.10. SCHIP
The State Children's Health Insurance Program (CHIP) enrollment process was simplified.[80]
1.11. Dependents
Dependents were permitted to remain on their parents' insurance plan until their 26th birthday, including dependents who no longer lived with their parents, are not a dependent on a parent's tax return, are no longer a student, or are married.[81][82]
1.12. Employer Mandate
Businesses that employ fifty or more people but do not offer health insurance to their full-time employees are assessed additional tax if the government has subsidized a full-time employee's healthcare through tax deductions or other means. This is commonly known as the employer mandate.[83][84] This provision was included to encourage employers to continue providing insurance once the exchanges began operating.[85]
1.13. Delivery System Reforms
The act includes delivery system reforms intended to constrain costs and improve quality. These include Medicare payment changes to discourage hospital-acquired conditions and readmissions, bundled payment initiatives, the Center for Medicare and Medicaid Innovation, the Independent Payment Advisory Board, and Accountable care organizations.
Hospital quality
Health care cost/quality initiatives included incentives to reduce hospital infections, adopt electronic medical records, and to coordinate care and prioritize quality over quantity.[86]
Bundled payments
Medicare switched from fee-for-service to bundled payments.[87][88] A single payment was to be paid to a hospital and a physician group for a defined episode of care (such as a hip replacement) rather than separate payments to individual service providers.[89]
Accountable Care Organizations
The Medicare Shared Savings Program (MSSP) was established by section 3022 of the Affordable Care Act. It is the program by which an Accountable Care Organization interacts with the federal government, and by which Accountable Care Organizations can be created.[90] It is a fee-for-service model.
The Act allowed the creation of Accountable Care Organizations (ACOs), which are groups of doctors, hospitals and other providers that commit to give coordinated care to Medicare patients. ACOs were allowed to continue using fee-for-service billing. They receive bonus payments from the government for minimizing costs while achieving quality benchmarks that emphasize prevention and mitigation of chronic disease. Missing cost or quality benchmarks subjected them to penalties.[91]
Unlike Health Maintenance Organizations, ACO patients are not required to obtain all care from the ACO. Also, unlike HMOs, ACOs must achieve quality of care goals.[91]
1.14. Medicare Drug Benefit (Part D)
Medicare Part D participants received a 50% discount on brand name drugs purchased after exhausting their initial coverage and before reaching the catastrophic-coverage threshold.[92] By 2020, the "doughnut hole" would be completely filled.[93]
1.15. State Waivers
From 2017 onwards, states can apply for a "waiver for state innovation" which allows them to conduct experiments that meet certain criteria.[94] To obtain a waiver, a state must pass legislation setting up an alternative health system that provides insurance at least as comprehensive and as affordable as PPACA, covers at least as many residents and does not increase the federal deficit.[95] These states can escape some of PPACA's central requirements, including the individual and employer mandates and the provision of an insurance exchange.[96] The state would receive compensation equal to the aggregate amount of any federal subsidies and tax credits for which its residents and employers would have been eligible under PPACA, if they cannot be paid under the state plan.[94]
1.16. Other Insurance Provisions
The Community Living Assistance Services and Supports Act (or CLASS Act) established a voluntary and public long-term care insurance option for employees,[97][98][99] The program was abolished as impractical without ever having taken effect.[100]
Consumer Operated and Oriented Plans (CO-OP), member-governed non-profit insurers, could start providing health care coverage, based on a 5-year federal loan.[101] As of 2017, only four of the original 23 co-ops were still in operation.[102]
1.17. Nutrition Labeling Requirements
Nutrition labeling requirements officially took effect in 2010, but implementation was delayed, and they actually took effect on May 7, 2018.[103]
2. Legislative History
PPACA followed a long series of unsuccessful attempts by one party or the other to pass major insurance reforms. Innovations were limited to health savings accounts (2003), medical savings accounts (1996) or flexible spending accounts, which increased insurance options, but did not materially expand coverage. Health care was a major factor in multiple elections, but until 2009, neither party had the votes to overcome the other's opposition.
2.1. Individual Mandate
The concept of an individual mandate goes back to at least 1989, when the conservative The Heritage Foundation proposed an individual mandate as an alternative to single-payer health care.[104][105] It was championed for a time by conservative economists and Republican senators as a market-based approach to healthcare reform on the basis of individual responsibility and avoidance of free rider problems. Specifically, because the 1986 Emergency Medical Treatment and Active Labor Act (EMTALA) requires any hospital participating in Medicare (nearly all do) to provide emergency care to anyone who needs it, the government often indirectly bore the cost of those without the ability to pay.[106][107][108]
President Bill Clinton proposed a major healthcare reform bill in 1993[109] that ultimately failed.[110] Clinton negotiated a compromise with the 105th Congress to instead enact the State Children's Health Insurance Program (SCHIP) in 1997.[111] The failed Clinton plan included a mandate for employers to provide health insurance to all employees through a regulated marketplace of health maintenance organizations. Republican Senators proposed an alternative that would have required individuals, but not employers, to buy insurance.
The 1993 Republican Health Equity and Access Reform Today (HEART) Act, contained a "universal coverage" requirement with a penalty for noncompliance—an individual mandate—as well as subsidies to be used in state-based 'purchasing groups'.[112] Advocates included prominent Republican Senators such as John Chafee, Orrin Hatch, Chuck Grassley, Bob Bennett and Kit Bond.[113][114] The 1994 Republican Consumer Choice Health Security Act, initially contained an individual mandate with a penalty provision;[115] however, author Don Nickles subsequently removed the mandate, stating, "government should not compel people to buy health insurance".[116] At the time of these proposals, Republicans did not raise constitutional issues; Mark Pauly, who helped develop a proposal that included an individual mandate for George H. W. Bush, remarked, "I don't remember that being raised at all. The way it was viewed by the Congressional Budget Office in 1994 was, effectively, as a tax."[104]
In 2006, an insurance expansion bill was enacted at the state level in Massachusetts. The bill contained both an individual mandate and an insurance exchange. Republican Governor Mitt Romney vetoed the mandate, but after Democrats overrode his veto, he signed it into law.[118] Romney's implementation of the 'Health Connector' exchange and individual mandate in Massachusetts was at first lauded by Republicans. During Romney's 2008 presidential campaign, Senator Jim DeMint praised Romney's ability to "take some good conservative ideas, like private health insurance, and apply them to the need to have everyone insured". Romney said of the individual mandate: "I'm proud of what we've done. If Massachusetts succeeds in implementing it, then that will be the model for the nation."[119]
In 2007 Republican Senator Bob Bennett and Democratic Senator Ron Wyden introduced the Healthy Americans Act, which featured an individual mandate and state-based, regulated insurance markets called "State Health Help Agencies".[108][119] The bill attracted bipartisan support, but died in committee. Many of its sponsors and co-sponsors remained in Congress during the 2008 healthcare debate.[120]
By 2008 many Democrats were considering this approach as the basis for healthcare reform. Experts said the legislation that eventually emerged from Congress in 2009 and 2010 bore similarities to the 2007 bill[112] and that it took ideas from the Massachusetts reforms.[121]
2.2. Healthcare Debate, 2008–10
Healthcare reform was a major topic during the 2008 Democratic presidential primaries. As the race narrowed, attention focused on the plans presented by the two leading candidates, Hillary Clinton and the eventual nominee, Barack Obama. Each candidate proposed a plan to cover the approximately 45 million Americans estimated to not have health insurance at some point each year. Clinton's proposal would have required all Americans to obtain coverage (in effect, an individual mandate), while Obama's proposal provided a subsidy without a mandate.[122][123]
During the general election, Obama said fixing healthcare would be one of his top four priorities as president.[124] Obama and his opponent, Senator John McCain, both proposed health insurance reforms, though their plans differed. McCain proposed tax credits for health insurance purchased in the individual market, which was estimated to reduce the number of uninsured people by about 2 million by 2018. Obama proposed private and public group insurance, income-based subsidies, consumer protections, and expansions of Medicaid and SCHIP, which was estimated at the time to reduce the number of uninsured people by 33.9 million by 2018 at a higher cost.[125]
Obama announced to a joint session of Congress in February 2009 his intent to work with Congress to construct a plan for healthcare reform.[126][127] By July, a series of bills were approved by committees within the House of Representatives.[128] On the Senate side, from June to September, the Senate Finance Committee held a series of 31 meetings to develop a proposal. This group—in particular, Democrats Max Baucus, Jeff Bingaman and Kent Conrad, along with Republicans Mike Enzi, Chuck Grassley and Olympia Snowe—met for more than 60 hours, and the principles they discussed, in conjunction with the other committees, became the foundation of a Senate bill.[129][130][131]
Congressional Democrats and health policy experts MIT economics professor Jonathan Gruber[132] and David Cutler argued that guaranteed issue would require both community rating and an individual mandate to ensure that adverse selection and/or "free riding" would not result in an insurance "death spiral".[133] They chose this approach after concluding that filibuster-proof support in the Senate was not present for more progressive plans such as single-payer. By deliberately drawing on bipartisan ideas—the same basic outline was supported by former Senate majority leaders Howard Baker, Bob Dole, Tom Daschle and George J. Mitchell—the bill's drafters hoped to garner the necessary votes.[134][135]
However, following the incorporation of an individual mandate into the proposal, Republicans threatened to filibuster any bill that contained it.[104] Senate minority leader Mitch McConnell, who led the Republican response, concluded Republicans should not support the bill.[136]
Republican Senators, including those who had supported earlier proposals with a similar mandate, began to describe the mandate as "unconstitutional". Journalist Ezra Klein wrote in The New Yorker, "a policy that once enjoyed broad support within the Republican Party suddenly faced unified opposition."[108]
The reform attracted attention from lobbyists,[137] including deals between lobby groups and the advocates to win the support of groups who had opposed past proposals.[138][139][140]

During the August 2009 summer congressional recess, many members went back to their districts and held town hall meetings on the proposals. The nascent Tea Party movement organized protests and many conservative groups and individuals attended the meetings to oppose the proposed reforms.[127] Threats were made against members of Congress over the course of the debate.[141]
In September 2009 Obama delivered another speech to a joint session of Congress supporting the negotiations.[142] On November 7, the House of Representatives passed the Affordable Health Care for America Act on a 220–215 vote and forwarded it to the Senate for passage.[127]
Senate
The Senate began work on its own proposals while the House was still working. The United States Constitution requires all revenue-related bills to originate in the House.[143] To formally comply with this requirement, the Senate repurposed H.R. 3590, a bill regarding housing tax changes for service members.[144] It had been passed by the House as a revenue-related modification to the Internal Revenue Code. The bill became the Senate's vehicle for its healthcare reform proposal, discarding the bill's original content.[145] The bill ultimately incorporated elements of proposals that were reported favorably by the Senate Health and Finance committees. With the Republican Senate minority vowing to filibuster, 60 votes would be necessary to pass the Senate.[146] At the start of the 111th Congress, Democrats had 58 votes. The Minnesota Senate election was ultimately won by Democrat Al Franken, making 59. Arlen Specter switched to the Democratic party in April 2009, giving them 60 seats, enough to end a filibuster.
Negotiations were undertaken attempting to satisfy moderate Democrats and to bring Republican senators aboard; particular attention was given to Republicans Bennett, Enzi, Grassley and Snowe.
After the Finance Committee vote on October 15, negotiations turned to moderate Democrats. Majority leader Harry Reid focused on satisfying centrists. The holdouts came down to Joe Lieberman of Connecticut, an independent who caucused with Democrats, and conservative Nebraska Democrat Ben Nelson. Lieberman's demand that the bill not include a public option[133][147] was met,[148] although supporters won various concessions, including allowing state-based public options such as Vermont's failed Green Mountain Care.[148][149]
![]()
On December 23, the Senate voted 60–39 to end debate on the bill: a cloture vote to end the filibuster.[153] The bill then passed, also 60–39, on December 24, 2009, with all Democrats and two independents voting for it, and all Republicans against (except Jim Bunning, who did not vote).[154] The bill was endorsed by the American Medical Association and AARP.[155]
On January 19, 2010, Massachusetts Republican Scott Brown was elected to the Senate in a special election to replace the recently deceased Edward Kennedy, having campaigned on giving the Republican minority the 41st vote needed to sustain Republican filibusters.[127][156][157] His victory was significant because of its effects on the legislative process. The first was psychological: the symbolic importance of losing Kennedy's traditionally Democratic Massachusetts seat made many Congressional Democrats concerned about the political cost of the bill.[158][159]
House
Brown's election meant Democrats could no longer break a filibuster in the Senate. In response, White House Chief of Staff Rahm Emanuel argued that Democrats should scale back to a less ambitious bill; House Speaker Nancy Pelosi pushed back, dismissing it as "Kiddie Care".[160][161]
Obama remained insistent on comprehensive reform. The news that Anthem in California intended to raise premium rates for its patients by as much as 39% gave him new evidence of the need for reform.[160][161] On February 22, he laid out a "Senate-leaning" proposal to consolidate the bills.[162] He held a meeting with both parties' leaders on February 25. The Democrats decided the House would pass the Senate's bill, to avoid another Senate vote.
House Democrats had expected to be able to negotiate changes in a House–Senate conference before passing a final bill. Since any bill that emerged from conference that differed from the Senate bill would have to pass the Senate over another Republican filibuster, most House Democrats agreed to pass the Senate bill on condition that it be amended by a subsequent bill.[159] They drafted the Health Care and Education Reconciliation Act, which could be passed by the reconciliation process.[160][163][164]
Per the Congressional Budget Act of 1974, reconciliation cannot be subject to a filibuster. But reconciliation is limited to budget changes, which is why the procedure was not used to pass PPACA in the first place; the bill had inherently non-budgetary regulations.[165][166] Although the already-passed Senate bill could not have been passed by reconciliation, most of House Democrats' demands were budgetary: "these changes—higher subsidy levels, different kinds of taxes to pay for them, nixing the Nebraska Medicaid deal—mainly involve taxes and spending. In other words, they're exactly the kinds of policies that are well-suited for reconciliation."[163]
The remaining obstacle was a pivotal group of pro-life Democrats led by Bart Stupak who were initially reluctant to support the bill. The group found the possibility of federal funding for abortion significant enough to warrant opposition. The Senate bill had not included language that satisfied their concerns, but they could not address abortion in the reconciliation bill as it would be non-budgetary. Instead, Obama issued Executive Order 13535, reaffirming the principles in the Hyde Amendment.[167] This won the support of Stupak and members of his group and assured the bill's passage.[164][168] The House passed the Senate bill with a 219–212 vote on March 21, 2010, with 34 Democrats and all 178 Republicans voting against it.[169] The next day, Republicans introduced legislation to repeal the bill.[170] Obama signed PPACA into law on March 23, 2010.[171]
2.3. Post-Enactment
Since passage, Republicans have voted to repeal all or parts of the Affordable Care Act more than sixty times; none have been successful.[172]
The Tax Cuts and Jobs Act of 2017 eliminated the fine for violating the individual mandate, starting in 2019. (The requirement itself is still in effect.)[42] In 2019 Congress repealed the so-called "Cadillac" tax on health insurance benefits, an excise tax on medical devices, and the Health Insurance Tax.[173]
3. Impact
3.1. Coverage
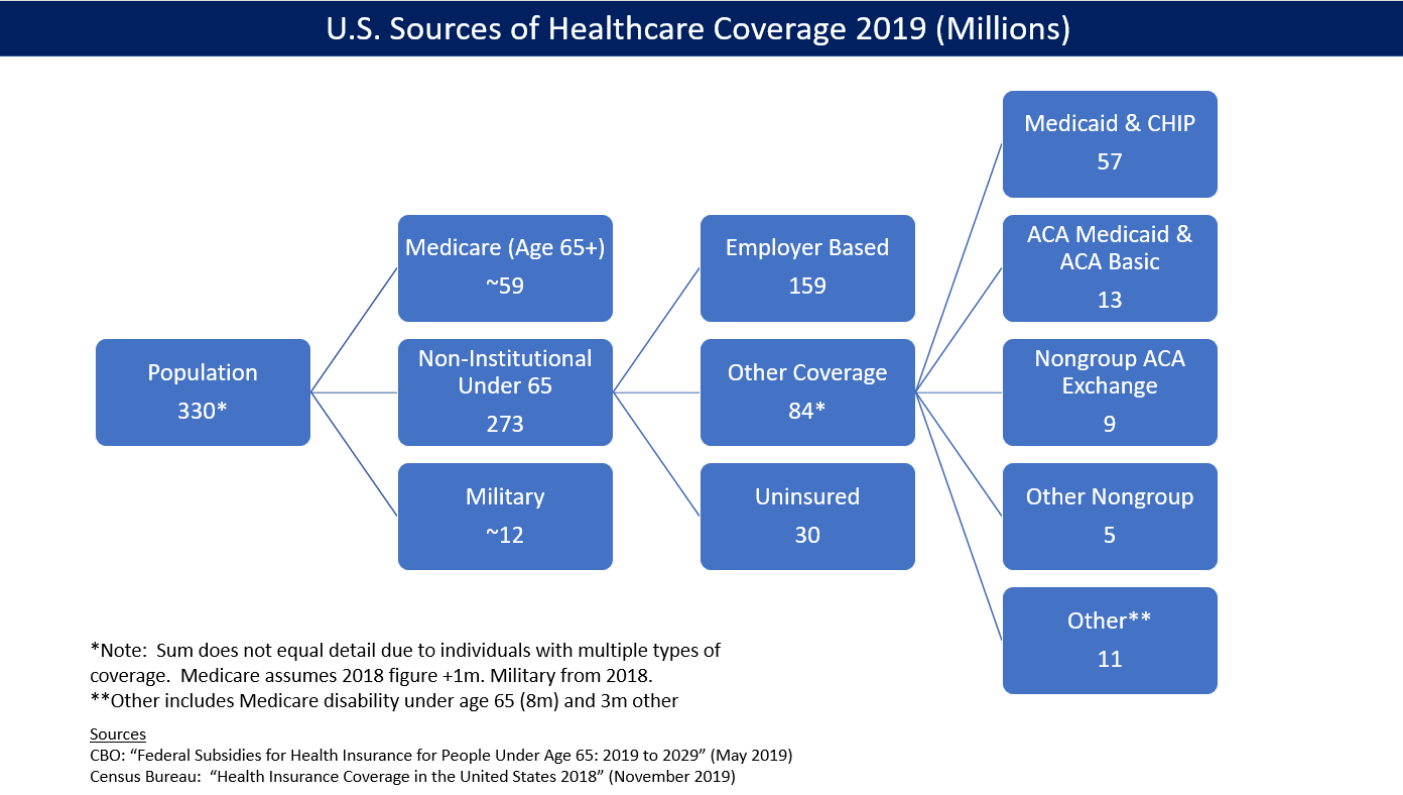
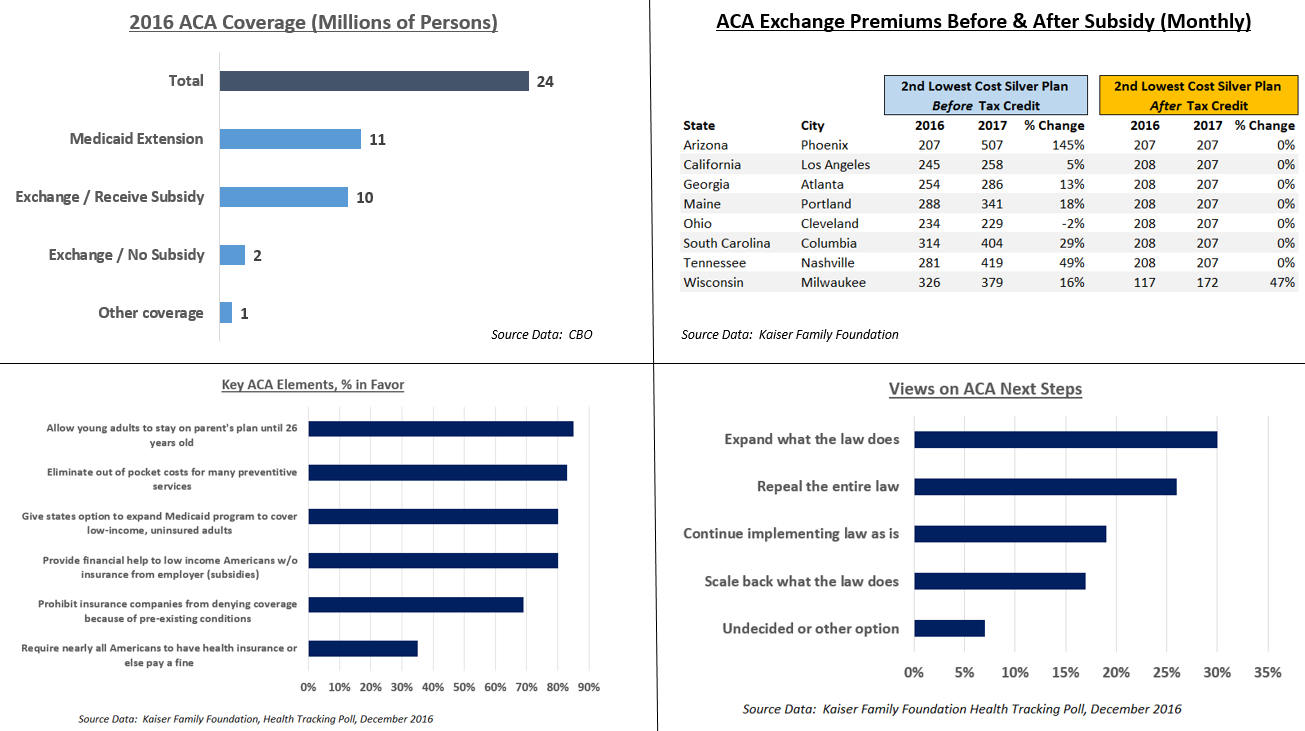
The law caused a significant reduction in the number and percentage of people without health insurance. The CDC reported that the percentage of people without health insurance fell from 16.0% in 2010 to 8.9% from January to June 2016.[175] The uninsured rate dropped in every congressional district in the U.S. from 2013 to 2015.[176] The Congressional Budget Office reported in March 2016 that approximately 12 million people were covered by the exchanges (10 million of whom received subsidies) and 11 million added to Medicaid. Another million were covered by PPACA's "Basic Health Program", for a total of 24 million.[174] CBO estimated that PPACA would reduce the net number of uninsured by 22 million in 2016, using a slightly different computation for the above figures totaling PPACA coverage of 26 million, less 4 million for reductions in "employment-based coverage" and "non-group and other coverage".[174]
The U.S. Department of Health and Human Services (HHS) estimated that 20.0 million adults (aged 18–64) gained healthcare coverage via PPACA as of February 2016;[177] similarly, the Urban Institute found in 2016 that 19.2 million non-elderly Americans gained health insurance coverage from 2010 to 2015.[178] In 2016, CBO estimated the uninsured at approximately 27 million people, or around 10% of the population or 7–8% excluding unauthorized immigrants.[174]
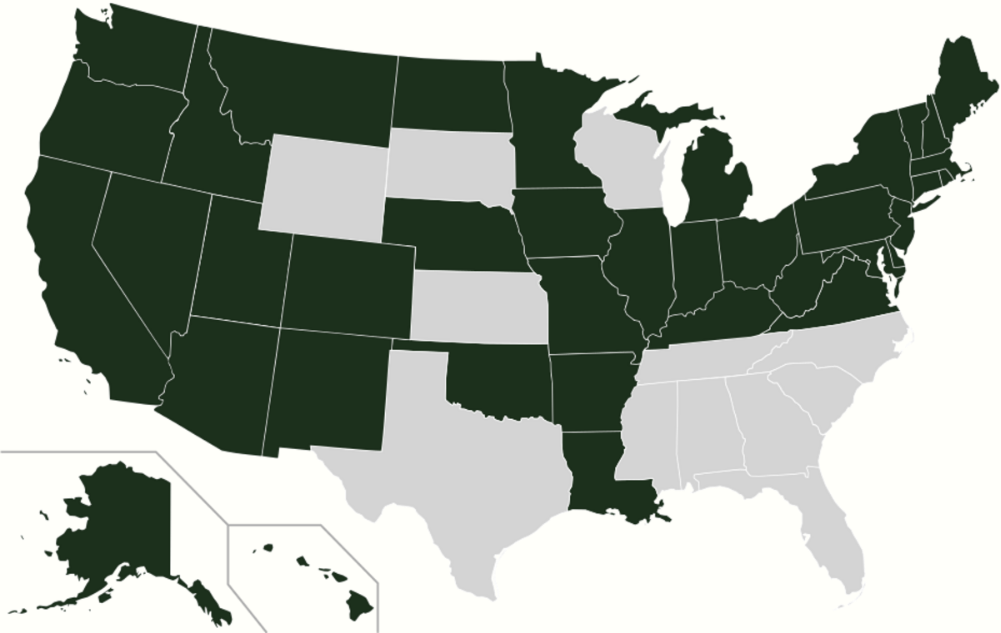
States that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while those that did not had a 14.1% uninsured rate, among adults aged 18–64.[179] As of December 2016 32 states (including Washington DC) had adopted the Medicaid extension.[180]
A 2017 study found that the ACA reduced socioeconomic disparities in health care access.[181]
The Affordable Care Act reduced the percent of Americans between 18 and 64 who were uninsured from 22.3 percent in 2010 to 12.4 percent in 2016. About 21 million more people have coverage ten years after the enactment of the ACA.[182][183]Ten years after its enactment studies showed that the ACA also had a positive effect on health and caused a reduction in mortality.[183]
3.2. Taxes
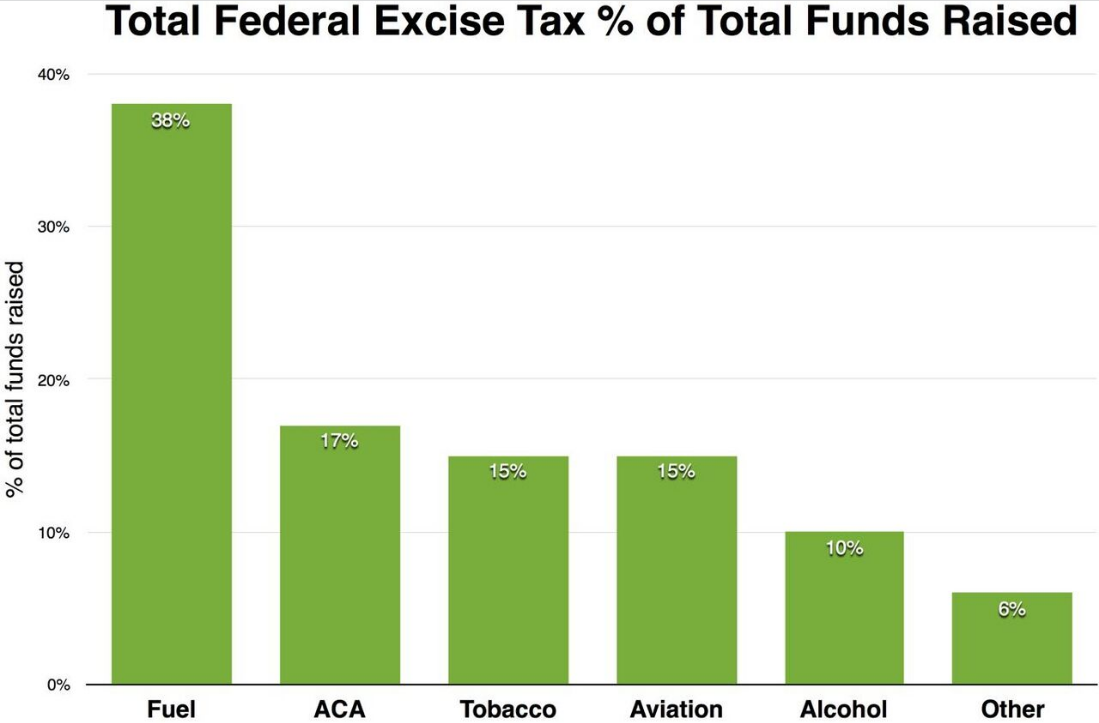
Excise taxes from the Affordable Care Act raised $16.3 billion in fiscal year 2015. $11.3 billion came from an excise tax placed directly on health insurers based on their market share. Annual excise taxes totaling $3 billion were levied on importers and manufacturers of prescription drugs.
The Individual mandate tax was $695 per individual or $2,085 per family at a minimum, reaching as high as 2.5% of household income (whichever was higher). The tax was reduced to 0 at the end of 2018.[184]
In fiscal year 2018, the individual and employer mandates yielded $4 billion each. Excise taxes on insurers and drug makers added $18 billion. Income tax surcharges produced 437 billion.[185]
PPACA reduced income inequality measured after taxes, due to the income tax surcharges and subsidies.[186] CBO estimated that subsidies paid under the law in 2016 averaged $4,240 per person for 10 million individuals receiving them, roughly $42 billion. The tax subsidy for the employer market, was approximately $1,700 per person in 2016, or $266 billion total.[174]
3.3. Insurance Exchanges
As of August 2016, 15 states operated their own health insurance marketplace. Other states either used the federal exchange, or operated in partnership with or supported by the federal government.[187] By 2019, 12 states and Washington DC operated their own exchanges.[188]
3.4. Medicaid Expansion
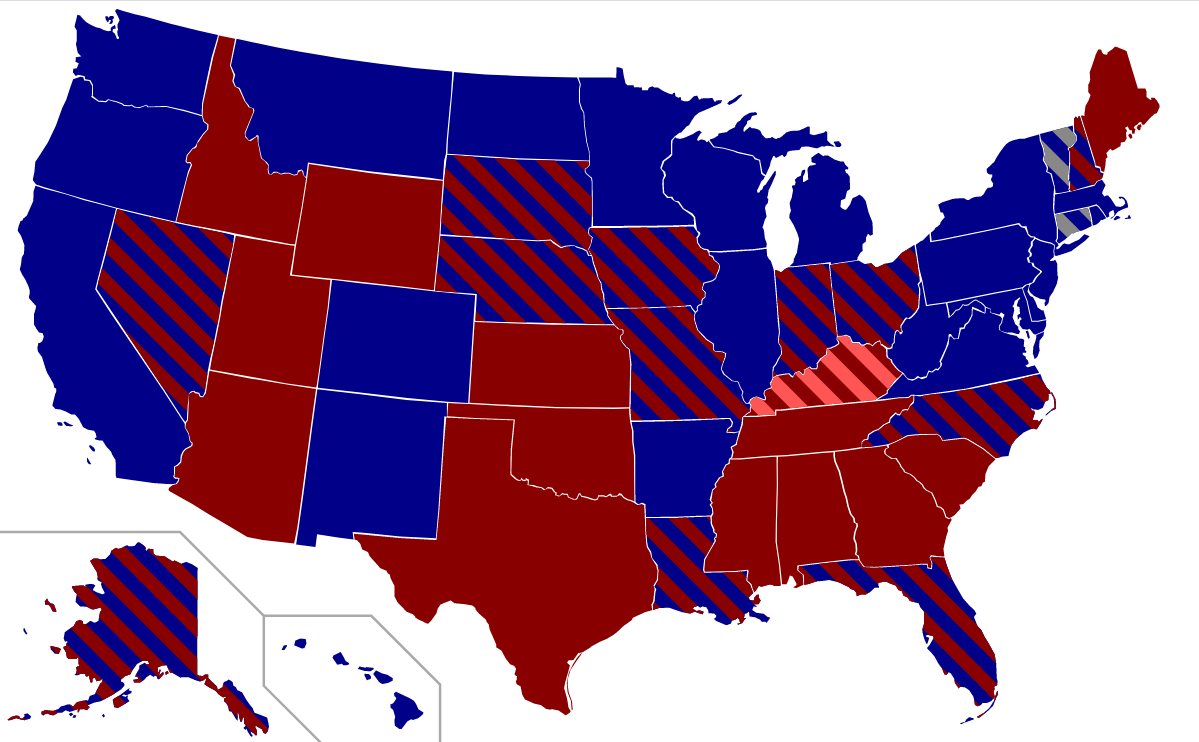
![]()
As of December 2019, 37 states (including Washington DC) had adopted the Medicaid extension.[180] Those states that expanded Medicaid had a 7.3% uninsured rate on average in the first quarter of 2016, while the others had a 14.1% uninsured rate, among adults aged 18 to 64.[179] Following the Supreme Court ruling in 2012, which held that states would not lose Medicaid funding if they did not expand Medicaid under PPACA, several states rejected the option. Over half the national uninsured population lived in those states.[191]
The Centers for Medicare and Medicaid Services (CMS) estimated that the cost of expansion was $6,366 per person for 2015, about 49 percent above previous estimates. An estimated 9 to 10 million people had gained Medicaid coverage, mostly low-income adults.[192] The Kaiser Family Foundation estimated in October 2015 that 3.1 million additional people were not covered because of states that rejected the Medicaid expansion.[193]
In many states income thresholds were significantly below 133% of the poverty line.[194] Many states did not make Medicaid available to childless adults at any income level.[195] Because subsidies on exchange insurance plans were not available to those below the poverty line, such individuals had no new options.[196][197] For example, in Kansas, where only able-bodied adults with children and with an income below 32% of the poverty line were eligible for Medicaid, those with incomes from 32% to 100% of the poverty level ($6,250 to $19,530 for a family of three) were ineligible for both Medicaid and federal subsidies to buy insurance. Absent children, able-bodied adults were not eligible for Medicaid there.[191]
Studies of the impact of Medicaid expansion rejections calculated that up to 6.4 million people would have too much income for Medicaid but not qualify for exchange subsidies.[198] Several states argued that they could not afford the 10% contribution in 2020.[199][200] Some studies suggested rejecting the expansion would cost more due to increased spending on uncompensated emergency care that otherwise would have been partially paid for by Medicaid coverage,[201]
A 2016 study found that residents of Kentucky and Arkansas, which both expanded Medicaid, were more likely to receive health care services and less likely to incur emergency room costs or have trouble paying their medical bills. Residents of Texas, which did not accept the Medicaid expansion, did not see a similar improvement during the same period.[202] Kentucky opted for increased managed care, while Arkansas subsidized private insurance. Later Arkansas and Kentucky governors proposed reducing or modifying their programs. From 2013 to 2015, the uninsured rate dropped from 42% to 14% in Arkansas and from 40% to 9% in Kentucky, compared with 39% to 32% in Texas.[203]
A 2016 DHHS study found that states that expanded Medicaid had lower premiums on exchange policies, because they had fewer low-income enrollees, whose health on average is worse than that of those with higher income.[204]
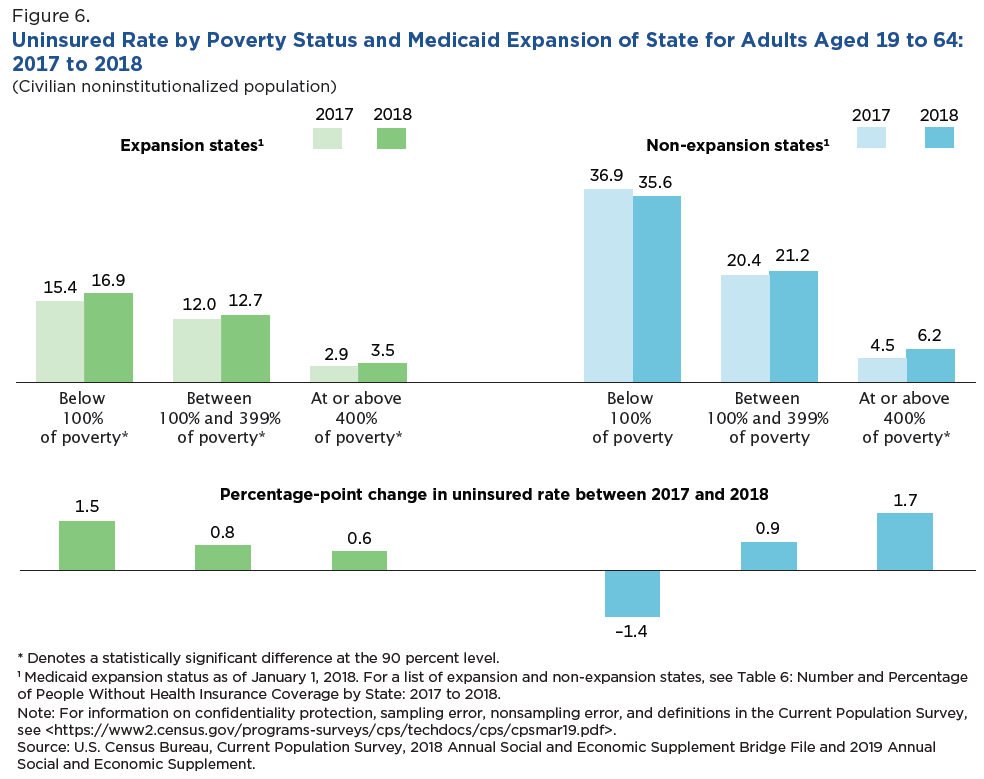
The Census Bureau reported in September 2019 that states that expanded Medicaid under PPACA had considerably lower uninsured rates than states that did not. For example, for adults between 100% and 399% of poverty level, the uninsured rate in 2018 was 12.7% in expansion states and 21.2% in non-expansion states. Of the 14 states with uninsured rates of 10% or greater, 11 had not expanded Medicaid.[190]
A July 2019 study by the National Bureau of Economic Research (NBER) indicated that states enacting Medicaid expansion exhibited statistically significant reductions in mortality rates.[205] From that study, states that took Medicaid expansion "saved the lives of at least 19,200 adults aged 55 to 64 over the four-year period from 2014 to 2017."[206] Further, 15,600 older adults died prematurely in the states that did not enact Medicaid expansion in those years according to the NBER research. "The lifesaving impacts of Medicaid expansion are large: an estimated 39 to 64 percent reduction in annual mortality rates for older adults gaining coverage."[206]
3.5. Insurance Costs
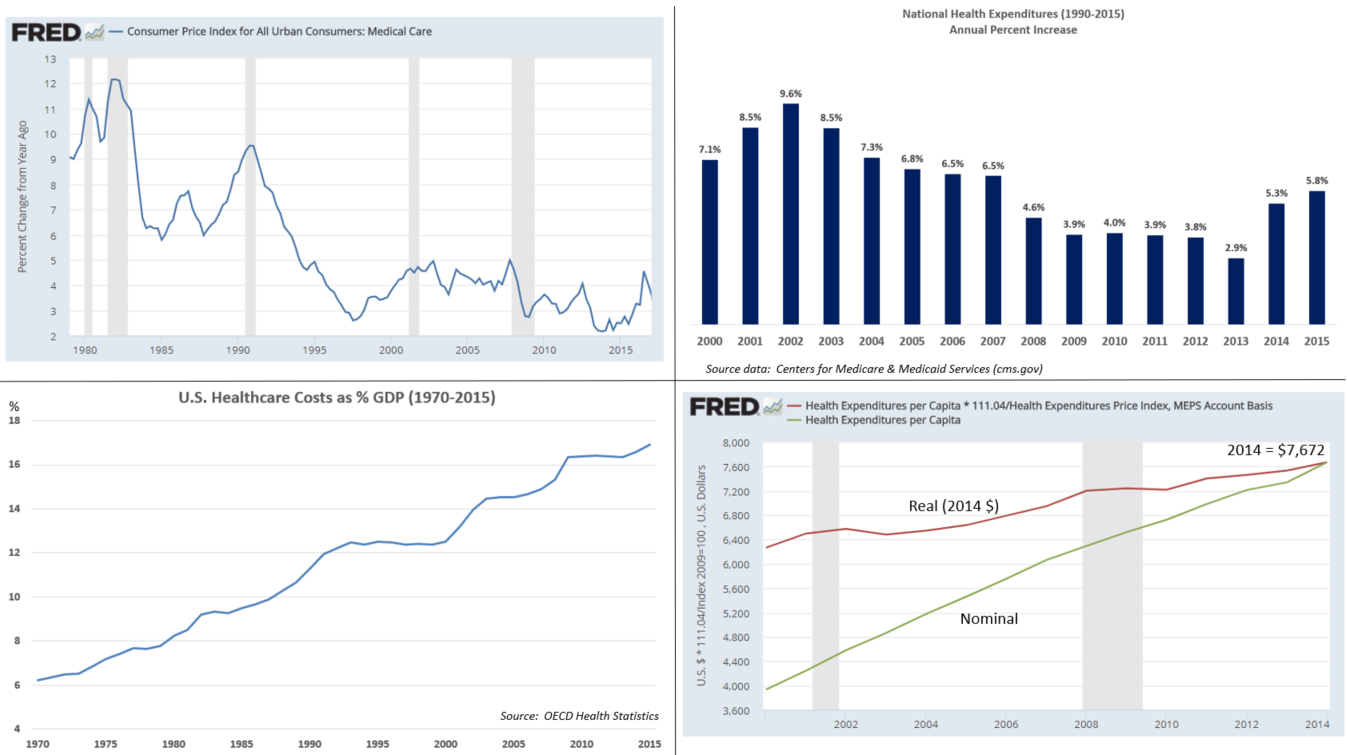
National health care expenditures rose faster than national income both before (2009-2013: 3.73%) and after (2014-2018: 4.82%) PPACA's major provisions took effect.[207] Premium prices rose considerably before and after. For example, a study published in 2016 found that the average requested 2017 premium increase among 40-year-old non-smokers was about 9 percent, according to an analysis of 17 cities, although Blue Cross Blue Shield proposed increases of 40 percent in Alabama and 60 percent in Texas.[208] However, some or all these costs were offset by tax credits. For example, the Kaiser Foundation reported that for the second-lowest cost "Silver plan", a 40-year old non-smoker making $30,000 per year would pay effectively the same amount in 2017 as they did in 2016 (about $208/month) after the tax credit, despite a large increase in the list price. This was consistent nationally. In other words, the subsidies increased along with the premium price, fully offsetting the increases for subsidy-eligible enrollees.[209]
Premium cost increases in the employer market moderated after 2009. For example, healthcare premiums for those covered by employers rose by 69% from 2000 to 2005, but only 27% from 2010 to 2015,[210] with only a 3% increase from 2015 to 2016.[211] From 2008 to 2010 (before passage of PPACA) health insurance premiums rose by an average of 10% per year.[212]
Several studies found that the financial crisis and accompanying recession could not account for the entirety of the slowdown and that structural changes likely shared at least partial credit.[213][214][215][216] A 2013 study estimated that changes to the health system had been responsible for about a quarter of the recent reduction in inflation.[217][clarification needed] Paul Krawzak claimed that even if cost controls succeed in reducing the amount spent on healthcare, such efforts on their own may be insufficient to outweigh the long-term burden placed by demographic changes, particularly the growth of the population on Medicare.[218]
In a 2016 review, Barack Obama claimed that from 2010 through 2014 mean annual growth in real per-enrollee Medicare spending was negative, down from a mean of 4.7% per year from 2000 through 2005 and 2.4% per year from 2006 to 2010; similarly, mean real per-enrollee growth in private insurance spending was 1.1% per year over the period, compared with a mean of 6.5% from 2000 through 2005 and 3.4% from 2005 to 2010.[219]
Deductibles and co-payments
A contributing factor to premium cost moderation was that the insured faced higher deductibles, copayments and out-of-pocket maximums. In addition, many employees chose to combine a health savings account with higher deductible plans, making the net impact of PPACA difficult to determine precisely.
For the group market (employer insurance), a 2016 survey found that:
- Deductibles grew 63% from 2011 to 2016, while premiums increased 19% and worker earnings grew by 11%.
- In 2016, 4 in 5 workers had an insurance deductible, which averaged $1,478. For firms with less than 200 employees, the deductible averaged $2,069.
- The percentage of workers with a deductible of at least $1,000 grew from 10% in 2006 to 51% in 2016. The 2016 figure dropped to 38% after taking employer contributions into account.[220]
For the non-group market, of which two-thirds are covered by PPACA exchanges, a survey of 2015 data found that:
- 49% had individual deductibles of at least $1,500 ($3,000 for family), up from 36% in 2014.
- Many exchange enrollees qualify for cost-sharing subsidies that reduce their net deductible.
- While about 75% of enrollees were "very satisfied" or "somewhat satisfied" with their choice of doctors and hospitals, only 50% had such satisfaction with their annual deductible.
- While 52% of those covered by PPACA exchanges felt "well protected" by their insurance, in the group market 63% felt that way.[221]
3.6. Health Outcomes
According to a 2014 study, PPACA likely prevented an estimated 50,000 preventable patient deaths from 2010 to 2013.[222] Himmelstein and Woolhandler wrote in January 2017 that a rollback of PPACA's Medicaid expansion alone would cause an estimated 43,956 deaths annually.[223]
According to the Kaiser Foundation, expanding Medicaid in the remaining states would cover up to 4.5 million persons.[224] A study by the National Bureau of Economic Research found a significant decline in mortality rates in the states that opted in to the Medicaid expansion program compared with those states that did not do so. The study reported that states decisions' not to expand Medicaid resulted in approximately 15,600 excess deaths from 2014 through 2017.[225][226]
Two 2018 JAMA studies found the Hospital Readmissions Reduction Program was associated with increased post-discharge mortality for patients hospitalized for heart failure and pneumonia.[227][228][229] A 2019 JAMA study found that PPACA decreased emergency department and hospital use by uninsured individuals.[230] A 2019 paper by Treasury Department economists using a randomized controlled trial (the IRS sent letters to some taxpayers noting that had paid a fine for not signing up for health insurance but not to other taxpayers) found that over the span of two years, obtaining health insurance reduced mortality by 12 percent.[231][232] The study concluded that the letters, sent to 3.9 million people, may have saved 700 lives.[231]
A 2020 JAMA study found that Medicare expansion under the ACA was associated with reduced incidence of advanced-stage breast cancer, indicating that Medicaid accessibility led to early detection of breast cancer and higher survival rates.[233]
3.7. Distributional Impact
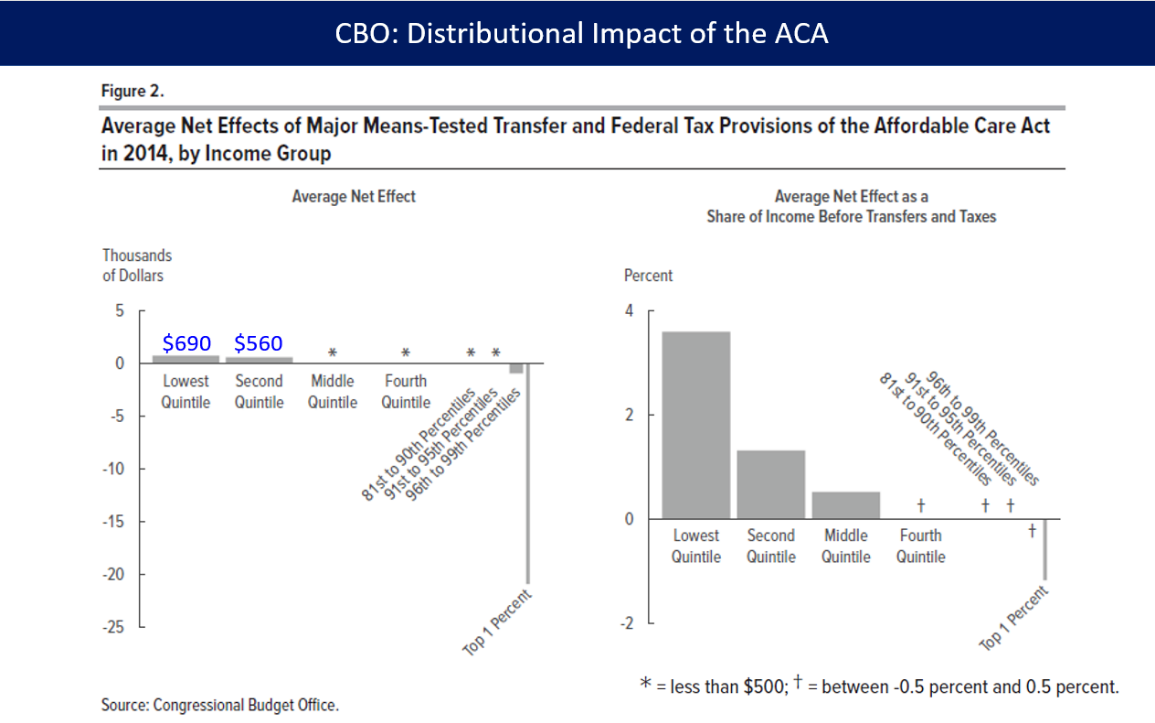
In March 2018, the CBO reported that PPACA had reduced income inequality in 2014, saying the law led the lowest and second quintiles (the bottom 40%) to receive an average of an additional $690 and $560 respectively while causing households in the top 1% to pay an additional $21,000 due mostly to the net investment income tax and the additional Medicare tax. The law placed relatively little burden on households in the top quintile (top 20%) outside of the top 1%.[234]
3.8. Federal Deficit
CBO estimates of revenue and impact on deficit
The CBO reported in multiple studies that PPACA would reduce the deficit, and repealing it would increase the deficit, primarily because of the elimination of Medicare reimbursement cuts.[235][236] The 2011 comprehensive CBO estimate projected a net deficit reduction of more than $200 billion during the 2012–2021 period:[236][237] it calculated the law would result in $604 billion in total outlays offset by $813 billion in total receipts, resulting in a $210 billion net deficit reduction.[236] The CBO separately predicted that while most of the spending provisions do not begin until 2014,[238][239] revenue would exceed spending in those subsequent years.[240] The CBO claimed the bill would "substantially reduce the growth of Medicare's payment rates for most services; impose an excise tax on insurance plans with relatively high premiums; and make various other changes to the federal tax code, Medicare, Medicaid, and other programs"[241]—ultimately extending the solvency of the Medicare trust fund by eight years.[242]
This estimate was made prior to the Supreme Court's ruling that enabled states to opt out of the Medicaid expansion, thereby forgoing the related federal funding. The CBO and JCT subsequently updated the budget projection, estimating the impact of the ruling would reduce the cost estimate of the insurance coverage provisions by $84 billion.[243][244][245]
The CBO in June 2015 forecast that repeal of PPACA would increase the deficit between $137 billion and $353 billion over the 2016–2025 period, depending on the impact of macroeconomic feedback effects. The CBO also forecast that repeal of PPACA would likely cause an increase in GDP by an average of 0.7% in the period from 2021 to 2025, mainly by boosting the supply of labor.[235]
Although the CBO generally does not provide cost estimates beyond the 10-year budget projection period because of the degree of uncertainty involved in the projection, it decided to do so in this case at the request of lawmakers, and estimated a second decade deficit reduction of $1.2 trillion.[241][246] CBO predicted deficit reduction around a broad range of one-half percent of GDP over the 2020s while cautioning that "a wide range of changes could occur".[247]
In 2017 CBO estimated that repealing the individual mandate alone would reduce the 10-year deficit by $338 billion.[248]
Opinions on CBO projections
The CBO cost estimates were criticized because they excluded the effects of potential legislation that would increase Medicare payments by more than $200 billion from 2010 to 2019.[249][250][251] However, the so-called "doc fix" is a separate issue that would have existed with or without PPACA.[252][253][254] The Center on Budget and Policy Priorities objected that Congress had a good record of implementing Medicare savings. According to their study, Congress followed through on the implementation of the vast majority of provisions enacted in the past 20 years to produce Medicare savings, although not the doc fix.[255][256] The doc fix became obsolete in 2015 when the savings provision was eliminated, permanently removing that spending restraint.[257]
Health economist Uwe Reinhardt, wrote, "The rigid, artificial rules under which the Congressional Budget Office must score proposed legislation unfortunately cannot produce the best unbiased forecasts of the likely fiscal impact of any legislation."[258] Douglas Holtz-Eakin alleged that the bill would increase the deficit by $562 billion because, he argued, it front-loaded revenue and back-loaded benefits.[259]
Scheiber and Cohn rejected critical assessments of the law's deficit impact, arguing that predictions were biased towards underestimating deficit reduction. They noted, for example, it is easier to account for the cost of definite levels of subsidies to specified numbers of people than to account for savings from preventive healthcare, and that the CBO had a track record of overestimating costs and underestimating savings of health legislation;[260][261] stating, "innovations in the delivery of medical care, like greater use of electronic medical records[262] and financial incentives for more coordination of care among doctors, would produce substantial savings while also slowing the relentless climb of medical expenses ... But the CBO would not consider such savings in its calculations, because the innovations hadn't really been tried on such large scale or in concert with one another—and that meant there wasn't much hard data to prove the savings would materialize."[260]
In 2010 David Walker said the CBO estimates were not likely to be accurate, because they were based on the assumption that the law would not change.[263]
3.9. Employer Mandate and Part-Time Work
The employer mandate applies to employers of more than fifty where health insurance is provided only to the full-time workers.[264] Critics claimed it created a perverse incentive to hire part-timers instead.[265][266] However, between March 2010 and 2014, the number of part-time jobs declined by 230,000 while the number of full-time jobs increased by two million.[267][268] In the public sector full-time jobs turned into part-time jobs much more than in the private sector.[267][269] A 2016 study found only limited evidence that PPACA had increased part-time employment.[270]
Several businesses and the state of Virginia added a 29-hour-a-week cap for their part-time employees,[271][272] to reflect the 30-hour-or-more definition for full-time worker.[264] As of 2013, few companies had shifted their workforce towards more part-time hours (4% in a survey from the Federal Reserve Bank of Minneapolis).[266] Trends in working hours[273] and the recovery from the Great Recession correlate with the shift from part-time to full-time work.[274][275] Other confounding impacts include that health insurance helps attract and retain employees, increases productivity and reduces absenteeism; and lowers corresponding training and administration costs from a smaller, more stable workforce.[266][273][276] Relatively few firms employ over 50 employees[266] and more than 90% of them already offered insurance.[277]
Most policy analysts (both right and left) were critical of the employer mandate provision.[265][277] They argued that the perverse incentives regarding part-time hours, even if they did not change existing plans, were real and harmful;[278][279] that the raised marginal cost of the 50th worker for businesses could limit companies' growth;[280] that the costs of reporting and administration were not worth the costs of maintaining employer plans;[278][279] and noted that the employer mandate was not essential to maintain adequate risk pools.[281][282] The provision generated vocal opposition from business interests and some unions who were not granted exemptions.[279][283]
3.10. Hospitals
From the start of 2010 to November 2014, 43 hospitals in rural areas closed. Critics claimed the new law had caused these closures. Many rural hospitals were built using funds from the 1946 Hill–Burton Act. Some of these hospitals reopened as other medical facilities, but only a small number operated emergency rooms (ER) or urgent care centers.[284]
Between January 2010 and 2015, a quarter of ER doctors said they had seen a major surge in patients, while nearly half had seen a smaller increase. Seven in ten ER doctors claimed they lacked the resources to deal with large increases in the number of patients. The biggest factor in the increased number of ER patients was insufficient primary care providers to handle the larger number of insured.[285]
Several large insurers formed ACOs. Many hospitals merged and purchased physician practices, amounting to a significant consolidation of the provider industry. The increased market share gave them more leverage with insurers and reduced patient care options.[91]
4. Attempted Repeals
The House, led by Republicans, repeatedly voted to repeal PPACA. The Senate, led by Democrats, did not follow suit.
4.1. Economic Consequences
CBO estimated in June 2015 that repealing PPACA would:
- Decrease GDP in the short-term, as government spending (on subsidies) was only partially replaced by spending by recipients.
- Increase the supply of labor and aggregate compensation by about 0.8 and 0.9 percent over the 2021–2025 period. CBO cited PPACA's expanded eligibility for Medicaid and subsidies and tax credits that rise with income as disincentives to work, so repealing PPACA would remove those disincentives, encouraging workers to supply more labor, increasing the total number of hours worked by about 1.5% over the 2021–2025 period.
- Remove the higher tax rates on capital income, thereby encouraging investment, raising the capital stock and output in the long-run.[235]
In 2015 the progressive Center for Economic and Policy Research found no evidence that companies were reducing worker hours to avoid PPACA requirements[286] for employees working more than 30 hours per week.[287]
CBO estimated that PPACA would slightly reduce the size of the labor force and number of hours worked, as some would no longer be tethered to employers for their insurance. Jonathan Cohn claimed that PPACA's primary employment effect was to alleviate job lock[288] and the reform's only significant employment impact was the retirement of those who were working only to stay insured.[289]
5. Public Opinion
Public views became increasingly negative in reaction to specific plans discussed during the legislative debate over 2009 and 2010. Approval varied by party, race and age. Some elements were more widely favored (pre-existing conditions) or opposed (individual mandate).
In a 2010 poll, 62% of respondents said they thought PPACA would "increase the amount of money they personally spend on health care", 56% said the bill "gives the government too much involvement in health care", and 19% said they thought they and their families would be better off with the legislation.[290] Other polls found that people were concerned the law would cost more than projected and would not do enough to control costs.[291]
In a 2012 poll 44% supported the law, with 56% against. By 75% of Democrats, 27% of Independents and 14% of Republicans favored the law. 82% favored banning insurance companies from denying coverage to people with pre-existing conditions, 61% favored allowing children to stay on their parents' insurance until age 26, 72% supported requiring companies with more than 50 employees to provide insurance for their employees, and 39% supported the individual mandate to own insurance or pay a penalty. By party affiliation, 19% of Republicans, 27% of Independents, and 59% of Democrats favored the mandate.[292] Other polls showed additional provisions receiving majority support, including the exchanges, pooling small businesses and the uninsured with other consumers and providing subsidies.[293][294]
Some opponents believed the reform did not go far enough: a 2012 poll indicated that 71% of Republican opponents rejected it overall, while 29% believed it did not go far enough; independent opponents were divided 67% to 33%; and among the much smaller group of Democratic opponents, 49% rejected it overall and 51% wanted more.[292]
In June 2013, a majority of the public (52–34%) indicated a desire for "Congress to implement or tinker with the law rather than repeal it".[295] After the Supreme Court upheld the individual mandate, a 2012 poll held that "most Americans (56%) want to see critics of President Obama's health care law drop efforts to block it and move on to other national issues".[296]
As of October 2013, approximately 40% were in favor while 51% were against.[297][298] About 29% of whites approved of the law, compared with 61% of Hispanics and 91% of African Americans.[299] A solid majority of seniors opposed the idea and a solid majority of those under forty were in favor.[300]
A 2014 poll reported that 26% of Americans support PPACA.[301] A later 2014 poll reported that 48.9% of respondents had an unfavorable view of PPACA vs. 38.3% who had a favorable view (of more than 5,500 individuals).[302] Another held that 8% of respondents agreed the Affordable Care Act "is working well the way it is".[303] In late 2014, a Rasmussen poll reported Repeal: 30%, Leave as is: 13%, Improve: 52%.[304]
In 2015, a poll reported that 47% of Americans approved the health care law. This was the first time a major poll indicated that more respondents approved than disapproved.[305] A December 2016 poll reported that: a) 30% wanted to expand what the law does; b) 26% wanted to repeal the entire law; c) 19% wanted to move forward with implementing the law as it is; and d) 17% wanted to scale back what the law does, with the remainder undecided.[306]
Separate polls from Fox News and NBC/WSJ, both taken during January 2017, indicated more people viewed the law favorably than did not for the first time. One of the reasons for the improving popularity of the law is that Democrats who had once opposed it (many still prefer "Medicare for all") shifted their positions because PPACA was under threat of repeal.[307] Another January 2017 poll reported that 35% of respondents believed "Obamacare" and the "Affordable Care Act" were different or did not know. (About 45% were unsure whether "repeal of Obamacare" also meant "repeal of the Affordable Care Act".) 39% did not know that "many people would lose coverage through Medicaid or subsidies for private health insurance if the A.C.A. were repealed and no replacement enacted," with Democrats far more likely (79%) to know that fact than Republicans (47%).[308] A 2017 study found that personal experience with public health insurance programs led to greater support for the Affordable Care Act, most prominently among Republicans and low-information voters.[309]
6. Political Aspects
6.1. "Obamacare"
The term "Obamacare" was originally coined by opponents as a pejorative. The term emerged in March 2007 when healthcare lobbyist Jeanne Schulte Scott wrote, "We will soon see a 'Giuliani-care' and 'Obama-care' to go along with 'McCain-care', 'Edwards-care', and a totally revamped and remodeled 'Hillary-care' from the 1990s".[310][311] According to research by Elspeth Reeve, the expression was used in early 2007, generally by writers describing the candidate's proposal for expanding coverage for the uninsured.[312] In May 2007 Mitt Romney introduced it to political discourse, saying, "How can we get those people insured without raising taxes and without having government take over healthcare?' And let me tell you, if we don't do it, the Democrats will. If the Democrats do it, it will be socialized medicine; it'll be government-managed care. It'll be what's known as Hillarycare or Barack Obamacare, or whatever you want to call it."[310]
By mid-2012, Obamacare had become the colloquial term used both by supporters and by opponents.[312] Obama endorsed the nickname, saying, "I have no problem with people saying Obama cares. I do care."[313]
6.2. Common Misconceptions
"Death panels"
On August 7, 2009, Sarah Palin pioneered the term "death panels" to describe groups who would decide whether sick patients were "worthy" of medical care.[314] "Death panel" referred to two claims about early drafts.
One was that under the law, seniors could be denied care due to their age[315] and the other that the government would advise seniors to end their lives instead of receiving care. The ostensible basis of these claims was the provision for an Independent Payment Advisory Board (IPAB).[316] IPAB was given the authority to recommend cost-saving changes to Medicare by facilitating the adoption of cost-effective treatments and cost-recovering measures when statutory expenditure levels were exceeded within any given 3-year period. In fact, the Board was prohibited from recommending changes that would reduce payments before 2020, and was prohibited from recommending changes in premiums, benefits, eligibility and taxes, or other changes that would result in rationing.[317][318]
The other related issue concerned advance-care planning consultation: a section of the House reform proposal would have reimbursed physicians for providing patient-requested consultations for Medicare recipients on end-of-life health planning (which is covered by many private plans), enabling patients to specify, on request, the kind of care they wished to receive.[319] The provision was not included in PPACA.[320]
In 2010, the Pew Research Center reported that 85% of Americans were familiar with the claim, and 30% believed it was true, backed by three contemporaneous polls.[321] The allegation was named PolitiFact's "Lie of the Year",[314][322] one of FactCheck.org's "whoppers"[323][324] and the most outrageous term by the American Dialect Society.[325] AARP described such rumors as "rife with gross—and even cruel—distortions".[326]
Members of Congress
PPACA requires members of Congress and their staffs to obtain health insurance either through an exchange or some other program approved by the law (such as Medicare), instead of using the insurance offered to federal employees (the Federal Employees Health Benefits Program).[327][328]
Illegal immigrants
PPACA explicitly denies insurance subsidies to "unauthorized (illegal) aliens".[37][38][329]
Exchange "death spiral"
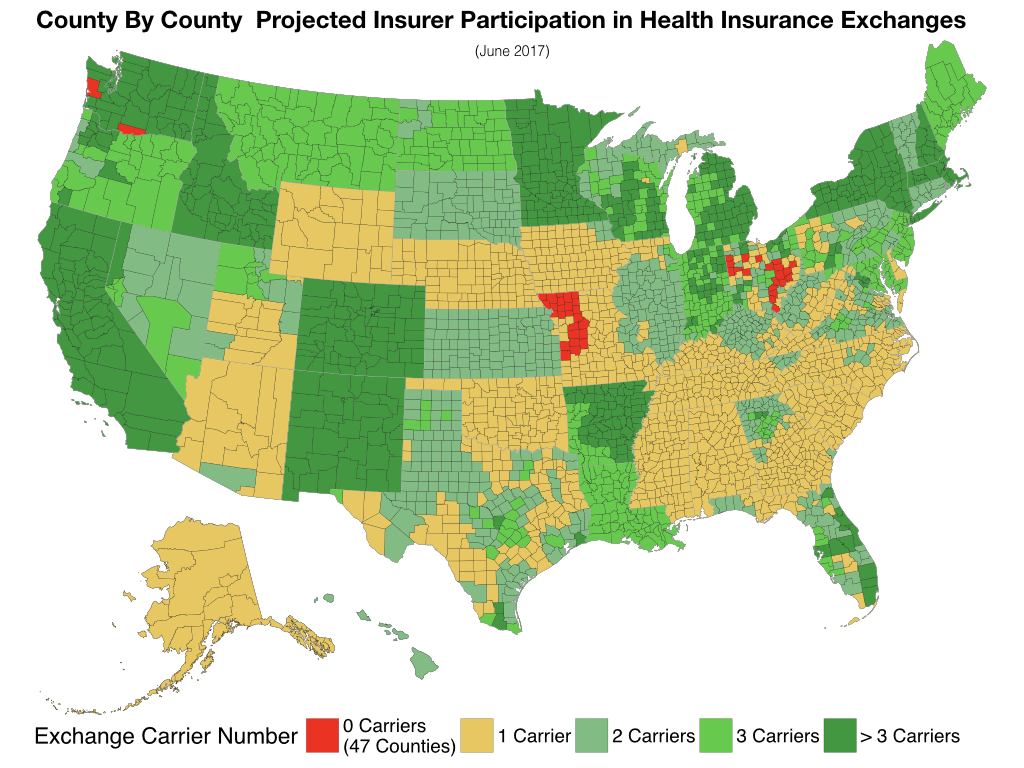
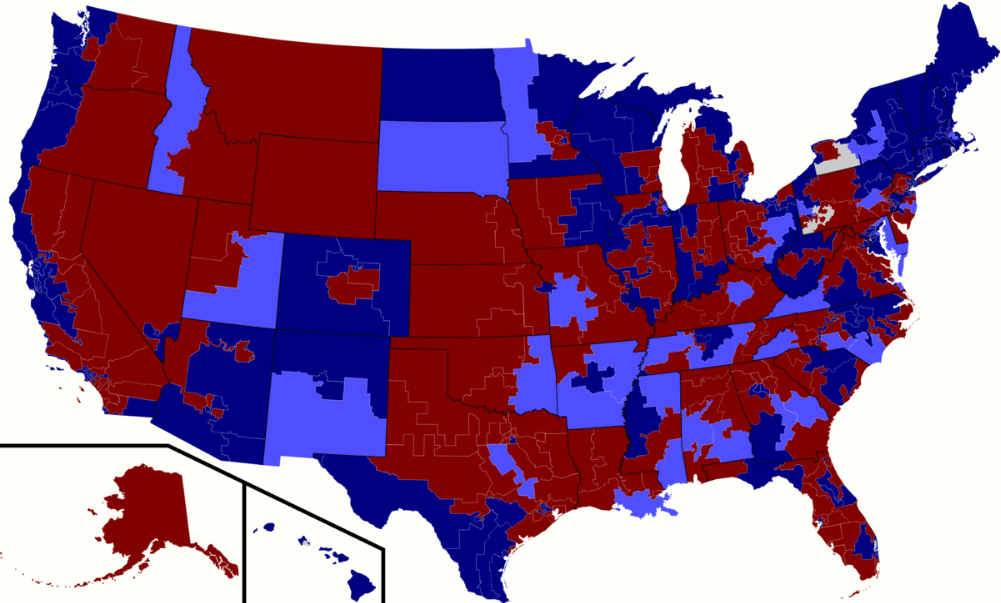
County By County Projected Insurer Participation in Health Insurance Exchanges. https://handwiki.org/wiki/index.php?curid=1587379
Opponents claimed that combining immediate coverage with no provision for pre-existing conditions would lead people to wait to get insured until they got sick. They individual mandate was designed to push people to get insured without waiting. This been called a "death spiral".[330] In the years after 2013, many insurers did leave specific marketplaces, claiming the risk pools were too small.
The median number of insurers per state was 4.0 in 2014, 5.0 in 2015, 4.0 in 2016 and 3.0 in 2017. Five states had one insurer in 2017; 13 had two; 11 had three; and the remainder had four or more.[331]
"If you like your plan"
At various times during and after PPACA debate Obama said, "If you like your health care plan, you'll be able to keep your health care plan."[332][333] However, in fall 2013 millions of Americans with individual policies received notices that their insurance plans were terminated,[334] and several million more risked seeing their current plans canceled.[335][336]
Poltifact cited various estimates that only about 2% of the total insured population (4 million out of 262 million) received such notices.[337] Obama's previous unambiguous assurance that consumers could keep their own plans became a focal point for critics, who challenged his truthfulness.[338][339] Various bills were introduced in Congress to allow people to keep their plans.[340] Politifact later scored Obama's claims as the "Lie of the Year".[341]
7. Criticism and Opposition
Opposition and efforts to repeal the legislation have drawn support from sources that include labor unions,[342][343] conservative advocacy groups,[344][345] Republicans, small business organizations and the Tea Party movement.[346] These groups claimed the law would disrupt existing health plans, increase costs from new insurance standards, and increase the deficit.[347] Some opposed the idea of universal healthcare, viewing insurance as similar to other unsubsidized goods.[348][349] President Donald Trump repeatedly promised to "repeal and replace" it.[350][351]
(As of 2013) unions that expressed concerns included the AFL-CIO,[352] which called PPACA "highly disruptive" to union health care plans, claiming it would drive up costs of union-sponsored plans; the International Brotherhood of Teamsters, United Food and Commercial Workers International Union, and UNITE-HERE, whose leaders sent a letter to Reid and Pelosi arguing, " PPACA will shatter not only our hard-earned health benefits, but destroy the foundation of the 40-hour work week that is the backbone of the American middle class."[343] In January 2014, Terry O'Sullivan, president of the Laborers' International Union of North America (LIUNA) and D. Taylor, president of Unite Here sent a letter to Reid and Pelosi stating, "ACA, as implemented, undermines fair marketplace competition in the health care industry."[342]
In October 2016, Mark Dayton, the governor of Minnesota and a member of the Minnesota Democratic–Farmer–Labor Party, said PPACA had "many good features" but it was "no longer affordable for increasing numbers of people"; he called on the state legislature to provide emergency relief to policyholders.[353] Dayton later said he regretted his remarks after they were seized on by Republicans seeking to repeal the law.[354]
7.1. Legal Challenges
National Federation of Independent Business v. Sebelius
Opponents challenged PPACA's constitutionality in multiple lawsuits on multiple grounds.[355][356] The Supreme Court ruled that the individual mandate was constitutional when viewed as a tax, although not under the Commerce Clause.
The Court further determined that states could not be forced to expand Medicaid. PPACA withheld all Medicaid funding from states declining to participate in the expansion. The Court ruled that this was unconstitutionally coercive and that individual states had the right to opt out without losing preexisting Medicaid funding.[357]
Contraception mandate
In March 2012, the Roman Catholic Church, while supportive of PPACA's objectives, voiced concern through the United States Conference of Catholic Bishops that aspects of the mandate covering contraception and sterilization and HHS's narrow definition of a religious organization violated the First Amendment right to free exercise of religion and conscience. Various lawsuits addressed these concerns.[358][359]
The Supreme Court ruled 7-2 on July 8, 2020, that employers with religious or moral objections to contraceptives can exclude such coverage from an employee's insurance plan. Writing for the majority, Justice Clarence Thomas said, "No language in the statute itself even hints that Congress intended that contraception should or must be covered. It was Congress, not the [administration], that declined to expressly require contraceptive coverage in the ACA itself." Justices Roberts, Alito, Gorsuch, and Kavanaugh joined Thomas' opinion. Justice Elena Kagan filed a concurring opinion in the judgment, in which Stephen Breyer joined. Justices Ginsburg and Sotomayor dissented, saying the court's ruling "leaves women workers to fend for themselves."[360]
King v Burwell
On June 25, 2015, the U.S. Supreme Court ruled 6–3 that federal subsidies for health insurance premiums could be used in the 34 states that did not set up their own insurance exchanges.[361]
House v. Price
House Republicans sued the Obama administration in 2014, alleging that Cost-sharing reduction subsidy payments to insurers were unlawful because Congress had not appropriated funds to pay for them. The argument classified the CSR subsidy as discretionary spending subject to annual appropriation. In May 2016 a federal judge ruled for the plaintiffs, but the Obama administration appealed.[362] Later, President Trump ended the payments. This led to further litigation.[363]
United States House of Representatives v. Azar
The House sued the administration alleging that the money for cost-sharing subsidy payments to insurers had not been appropriated, as required for any federal government spending. PPACA subsidy that helps customers pay premiums was not part of the suit.
Without the cost-sharing subsidies, the government estimated that premiums would increase by 20 percent to 30 percent for silver plans.[364] In 2017, the uncertainty about whether the payments would continue caused Blue Cross Blue Shield of North Carolina to try to raise premiums by 22.9 percent the next year, as opposed to an increase of only 8.8 percent that it would have sought if the payments were assured.[365]
U.S. District Judge Rosemary M. Collyer ruled that the cost-sharing program was unconstitutional for spending money that has not been specifically provided by an act of Congress, but concluded that Congress had in fact authorized that program to be created. The judge also found that Congress had provided authority to cover the spending for the tax credits to consumers who use them to help afford health coverage.[366] The judge enjoined further cost-sharing payments, but stayed the order pending appeal, to the United States Court of Appeals for the District of Columbia Circuit. The case ended in a settlement before the Circuit Court.
California v. Texas
Texas and nineteen other states filed a civil suit in the United States District Court for the Northern District of Texas in February 2018, arguing that with the passage of the Tax Cuts and Jobs Act of 2017, which eliminated the tax for not having health insurance, the individual mandate no longer had a constitutional basis and thus the entire PPACA was no longer constitutional.[367] The Department of Justice said it would no longer defend PPACA in court, but seventeen states led by California stepped in to do so.[368]
District Judge Reed O'Connor of Texas ruled for the plaintiffs on December 14, 2018, stating that the "Individual Mandate can no longer be fairly read as an exercise of Congress's Tax Power and is still impermissible under the Interstate Commerce Clause—meaning the Individual Mandate is unconstitutional." He then further reasoned that the individual mandate is an essential part of the entire law, and thus was not severable, making the entire law unconstitutional.[369][370] Judge O'Connor's decision regarding severability turned on several passages from the Congressional debate that focused on the importance of the mandate.[371] While he ruled the law unconstitutional, he did not overturn the law.[368]
The intervening states appealed the decision to the Fifth Circuit. These states argued that Congress's change in the tax was only reducing the amount of the tax, and that Congress had the power to write a stronger law to this end.[372][373] O'Connor stayed his decision pending the appeal.[374] The Fifth Circuit heard the appeal on July 9, 2019; in the interim, the U.S. Department of Justice joined with Republican states to argue that the PPACA was unconstitutional, while the Democratic states were joined by the Democrat-controlled U.S. House of Representatives. In addition to the questions on PPACA, an additional question on standing was addressed, as the Republican plaintiffs challenged whether the Democratic states had standing to defend PPACA.[375][376]
In December 2019, the Fifth Circuit agreed the individual mandate was unconstitutional. It did not, however, agree that the entire law should be voided. Instead, it remanded the case to the District Court for reconsideration of that question.[377] The Supreme Court accepted the case in March 2020, but to be heard in the 2020–2021 term,[378] with the ruling likely falling after the 2020 elections.[379]
Democrats pointed out that the effect of invalidating the entire law would be to remove popular provisions such as the protection for pre-existing conditions, and that the Republicans had still not offered any replacement plan—important issues for the 2020 elections.[379]
Risk Corridors
The Supreme Court ruled that promised Risk Corridor payments must be made even in the absence of specific appropriation of money by Congress.[68]
Non-cooperation
Officials in Texas, Florida, Alabama, Wyoming, Arizona, Oklahoma and Missouri opposed those elements over which they had discretion.[380][381] For example, Missouri declined to expand Medicaid or establish a health insurance marketplace engaging in active non-cooperation, enacting a statute forbidding any state or local official to render any aid not specifically required by federal law.[382] Other Republicans discouraged efforts to advertise the law's benefits. Some conservative political groups launched ad campaigns to discourage enrollment.[383][384]
7.2. Repeal Efforts
PPACA was the subject of many unsuccessful repeal efforts by Republicans in the 111th, 112th, and 113th Congresses: Representatives Steve King (R-IA) and Michele Bachmann (R-MN) introduced bills in the House to repeal PPACA the day after it was signed, as did Senator Jim DeMint (R-SC) in the Senate.[385] In 2011, after Republicans gained control of the House of Representatives, one of the first votes held was on a bill titled "Repealing the Job-Killing Health Care Law Act" (H.R. 2), which the House passed 245–189.[386] All Republicans and three Democrats voted for repeal.[387] In the Senate, the bill was offered as an amendment to an unrelated bill, but was voted down.[388] President Obama said he would veto the bill had passed.[389]
On February 3, 2015, the House of Representatives added its 67th repeal vote to the record (239 to 186). This attempt also failed.[390]
2013 federal government shutdown
Strong partisan disagreement in Congress prevented adjustments to the Act's provisions.[391] However, at least one change, a proposed repeal of a tax on medical devices, has received bipartisan support.[392] Some Congressional Republicans argued against improvements to the law on the grounds they would weaken the arguments for repeal.[279][393]
Republicans attempted to defund its implementation,[381][394] and in October 2013 House Republicans refused to fund the federal government unless it came with an implementation delay, after the President unilaterally deferred the employer mandate by one year, which critics claimed he had no power to do. The House passed three versions of a bill funding the government while submitting various versions that would repeal or delay PPACA, with the last version delaying enforcement of the individual mandate. The Democratic Senate leadership stated the Senate would pass only a bill without any restrictions on PPACA. The government shutdown lasted from October 1–17.[395][396][397]
2017 repeal effort
During a midnight congressional session starting January 11, the Senate of the 115th Congress of the United States voted to approve a "budget blueprint" that would allow Republicans to repeal parts of the law "without threat of a Democratic filibuster".[398][399] The plan, which passed 51–48, was named by Senate Republicans the "Obamacare 'repeal resolution.'"[400] Democrats opposing the resolution staged a protest during the vote.[401]
House Republicans announced their replacement, the American Health Care Act, on March 6.[402] On March 24 the effort failed amid a revolt among Republican representatives.[403]
On May 4 the House voted to pass the American Health Care Act by a margin of 217 to 213.[404] The Senate Republican leadership announced that Senate Republicans would write their own version of the bill, instead of voting on the House version.[405]
Leader McConnell named a group of 13 Republicans to draft the substitute version in private, raising bipartisan concerns about a lack of transparency.[406][407][408] On June 22 Republicans released the first discussion draft, which would rename it the "Better Care Reconciliation Act of 2017" (BCRA).[409] On July 25 although no amendment proposal had garnered majority support, Republicans voted to advance the bill to the floor and begin formal consideration of amendments. Senators Susan Collins and Lisa Murkowski were the only two dissenting Republicans making the vote a 50–50 tie. Vice President Mike Pence then cast the tiebreaking vote in the affirmative.[410]
The revised BCRA failed, 43–57. A subsequent "Obamacare Repeal and Reconciliation Act" abandoned the "repeal and replace" approach in favor of a straight repeal, but that too failed. 45–55. Finally, the "Health Care Freedom Act", nicknamed "skinny repeal" because it would have made the least change to PPACA, failed by 49–51, with Collins, Murkowski, and McCain joining all the Democrats and independents in voting against it.[411]
7.3. Actions to Hinder Implementation
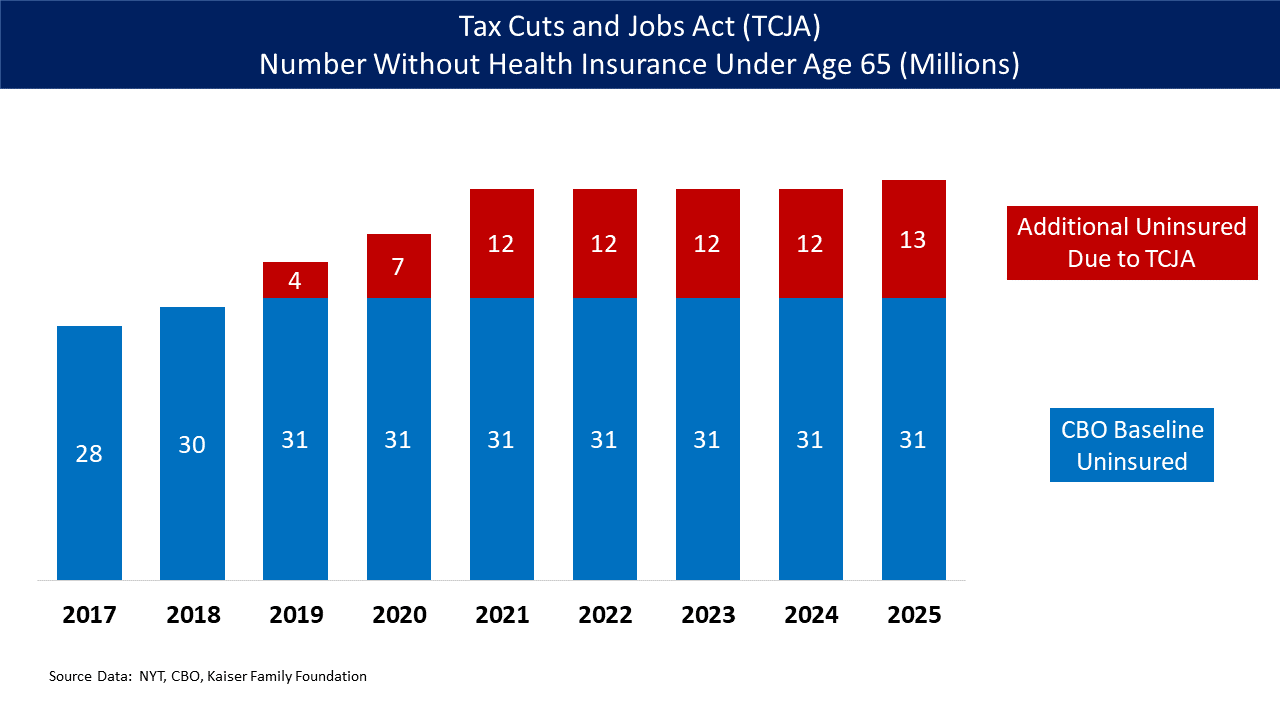
Under both PPACA (current law) and the AHCA, CBO reported that the health exchange marketplaces would remain stable.[413] However, Republican politicians took a variety of steps to undermine it, creating uncertainty that adversely impacted enrollment and insurer participation while increasing premiums.[414] Concern of the exchanges became another argument for reforms. Past and ongoing Republican attempts to weaken the law have included:
- Lawsuits such as King v. Burwell and House v. Price.
- President Trump ended the payment of cost-sharing reduction subsidies to insurers on October 12, 2017. CBO estimated in September 2017 that discontinuing the payments would add an average of 15–20 percentage points to health insurance costs on the exchanges in 2018 while increasing the budget deficit nearly $200 billion over a decade.[415] In response, insurers sued the government for reimbursement. Various cases are under appeal as of 2019.[363] Several insurers and actuarial groups estimated this resulted in a 20 percentage point or more increase in premiums for the 2018 plan year. In other words, premium increases expected to be 10% or less in 2018 became 28–40% instead.[416][417] The insurers would need to make up the $7 billion they had previously received in CSRs by raising premiums. Since most premiums are subsidized, the federal government would cover most of the increases. CBO also estimated that initially up to one million fewer would have health insurance coverage, although rising subsidies might eventually offset this. The 85% of enrollees who received subsidies would be unaffected. CBO expected the exchanges to remain stable (i.e., no "death spiral" before or after Trump's action) as the premiums would increase and prices would stabilize at the higher (non-CSR) level.[418] Several insurance companies who sued the United States for failure to pay cost-sharing reduction (CSR) payments won several cases in 2018 & 2019. The Judiciary decided the insurance companies are entitled to unpaid CSR payments.[419][420]
- The 2015 appropriations bill had a rider that ended the payment of risk corridor funds. This was repeated in later years. This resulted in the bankruptcy of many co-ops. This action was attributed to Senator Rubio.[421] The cutoff generated some 50 lawsuits. The Supreme Court granted certiorari in 2019 in the case Maine Community Health Options v. United States.[422][423][424]
- Trump weakened the individual mandate with his first executive order, which limited enforcement of the tax. For example, tax returns without indications of health insurance ("silent returns") will still be processed, overriding Obama's instructions to reject them.[425]
- Trump reduced funding for advertising for exchange enrollment by up to 90%, with other reductions to support resources used to answer questions and help people sign-up for coverage.[426] CBO said the reductions would reduce PPACA enrollment.[415]
- Trump reduced the enrollment period for 2018 by half, to 45 days.[427]
- Trump made public statements that the exchanges were unstable or in a death spiral.[428]
8. Implementation
In 2010 small business tax credits took effect.[429] Then Pre-Existing Condition Insurance Plan (PCIP) took effect to offer insurance to those who had been denied coverage by private insurance companies because of a pre-existing condition.[429] By 2011, insurers had stopped marketing child-only policies in 17 states, as they sought to escape this requirement.[430] In National Federation of Independent Business v. Sebelius the Supreme Court allowed states to opt out of the Medicaid expansion.[431][432][433]
In 2013, the Internal Revenue Service ruled that the cost of covering only the individual employee would be considered in determining whether the cost of coverage exceeded 9.5% of income. Family plans would not be considered even if the cost was above the 9.5% income threshold.[434][435] On July 2 Obama delayed the employer mandate until 2015.[277][436][437] The launch for both the state and federal exchanges was a disaster due to management and technical failings. HealthCare.gov, the website that offers insurance through the exchanges operated by the federal government, crashed on opening and suffered endless problems.[438] Operations stabilized in 2014, although not all planned features were complete.[439][440]
The Government Accountability Office released a non-partisan study in 2014 that concluded the administration had not provided "effective planning or oversight practices" in developing the exchanges.[441] In Burwell v. Hobby Lobby the Supreme Court exempted closely held corporations with religious convictions from the contraception rule.[442] At the beginning of the 2015, 11.7 million had signed up (ex-Medicaid).[443] By the end of the year about 8.8 million consumers had stayed in the program.[444] Congress repeatedly delayed the onset of the "Cadillac tax" on expensive insurance plans first until 2020[445] and later until 2022.
An estimated 9 to 10 million people had gained Medicaid coverage in 2016, mostly low-income adults.[192] The five major national insurers expected to lose money on PPACA policies in 2016,[446] in part because the enrollees were lower income, older and sicker than expected.[447]
More than 9.2 million people (3.0 million new customers and 6.2 million returning) enrolled on the national exchange in 2017, down some 400,000 from 2016. This decline was due primarily to the election of President Trump.[448] The eleven states that run their own exchanges signed up about 3 million more.[448] The IRS announced that it would not require that tax returns indicate a person has health insurance, reducing the effectiveness of the individual mandate, in response to Trump's executive order.[449] The CBO reported in March that the healthcare exchanges were expected to be stable.[413] In May the House voted to repeal PPACA using the American Health Care Act.[450][451] The individual mandate was repealed starting in 2019 via the Tax Cuts and Jobs Act.[41] The CBO estimated that the repeal would cause 13 million fewer people to have health insurance in 2027.[452]
The 2017 Individual Market Stabilization Bill was proposed to fund cost cost-sharing reductions,[453] provide more flexibility for state waivers, allow a new "Copper Plan" offering only catastrophic coverage, allow interstate insurance compacts, and redirect consumer fees to states for outreach. The bill failed.
By 2019, 35 states and the District of Columbia had either expanded coverage via traditional Medicaid or via an alternative program.[454]
The content is sourced from: https://handwiki.org/wiki/Finance:Patient_Protection_and_Affordable_Care_Act
References
- Oberlander, Jonathan (June 1, 2010). "Long Time Coming: Why Health Reform Finally Passed" (in en). Health Affairs 29 (6): 1112–1116. doi:10.1377/hlthaff.2010.0447. ISSN 0278-2715. PMID 20530339. https://dx.doi.org/10.1377%2Fhlthaff.2010.0447
- Blumenthal, David; Abrams, Melinda; Nuzum, Rachel (June 18, 2015). "The Affordable Care Act at 5 Years". New England Journal of Medicine 372 (25): 2451–2458. doi:10.1056/NEJMhpr1503614. ISSN 0028-4793. PMID 25946142. https://semanticscholar.org/paper/2b0dcda73ff2a1903393ac3ac038a6033eba8aea.
- Cohen, Alan B.; Colby, David C.; Wailoo, Keith A.; Zelizer, Julian E. (June 1, 2015) (in en). Medicare and Medicaid at 50: America's Entitlement Programs in the Age of Affordable Care. Oxford University Press. ISBN 9780190231569. https://books.google.com/books?id=H9DGBwAAQBAJ.
- Stolberg, Sheryl Gay; Pear, Robert (March 23, 2010). "Obama Signs Health Care Overhaul Into Law". The New York Times. https://www.nytimes.com/2010/03/24/health/policy/24health.html.
- Vicini, James; Stempel, Jonathan; Biskupic, Joan (June 28, 2017). "Top court upholds healthcare law in Obama triumph". Reuters. https://www.reuters.com/article/us-usa-healthcare-court-idUSBRE85R06420120628.
- "Health insurance that counts as coverage" (in en). https://www.healthcare.gov/fees/plans-that-count-as-coverage/.
- "Age Band Rating (ACA)". National Association of Personal Financial Advisors. http://www.naifa.org/practice-resources/prp/age-band-rating-(aca).
- "HHS and states move to establish Affordable Insurance Exchanges, give Americans the same insurance choices as members of Congress" (Press release). HHS. July 11, 2011. Archived from the original on April 14, 2012. Retrieved April 9, 2012. https://web.archive.org/web/20120414044029/http://www.hhs.gov/news/press/2011pres/07/20110711a.html
- "Essential Health Benefits". HealthCare.gov. September 23, 2010. https://www.healthcare.gov/glossary/essential-health-benefits/. Retrieved February 9, 2016.
- Medicare, Centers for; Baltimore, Medicaid Services 7500 Security Boulevard; Usa, Md21244 (December 19, 2014). "ratereview". https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/ratereview.html.
- "Clinical Guidelines and Recommendations" (in en-us). http://www.ahrq.gov/prevention/guidelines/index.html.
- "Login". http://www.shrm.org/publications/hrnews/pages/coverpreventivecare.aspx. Retrieved February 18, 2015.
- Levitt, Larry; Claxton, Gary; Pollitz, Karen (October 18, 2011). "Questions About Essential Health Benefits". Kaiser Family. http://kff.org/health-reform/perspective/questions-about-essential-health-benefits.
- "Quick Take: Essential Health Benefits: What Have States Decided for Their Benchmark?". Kaiser Family. December 7, 2012. http://kff.org/health-reform/fact-sheet/quick-take-essential-health-benefits-what-have-states-decided-for-their-benchmark.
- PPACA, 2713,(a)(4) https://www.govtrack.us/congress/bills/111/hr3590/text
- Women's Preventive Services Guidelines HRSA, U.S. Department of Health and Human Services https://www.hrsa.gov/womensguidelines/
- "Women's Preventive Services Coverage and Non-Profit Religious Organizations". Centers for Medicare and Medicaid Services. http://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/womens-preven-02012013.html. Retrieved September 8, 2013.
- Kliff, Sarah (August 1, 2012). "Five facts about the health law's contraceptive mandate". The Washington Post. https://www.washingtonpost.com/blogs/wonkblog/wp/2012/08/01/five-facts-about-the-health-laws-contraceptive-mandate. Retrieved November 29, 2012.
- Dept. Health and Human Services (February 10, 2012). "Group Health Plans and Health Insurance Issuers Relating to Coverage of Preventive Services Under the Patient Protection and Affordable Care Act – Final Rules" (77 FR 8725). Federal Register. http://www.gpo.gov/fdsys/granule/FR-2012-02-15/2012-3547/content-detail.html. Retrieved February 15, 2012. "Summary: These regulations finalize, without change, interim final regulations authorizing the exemption of group health plans and group health insurance coverage sponsored by certain religious employers from having to cover certain preventive health services under provisions of the Patient Protection and Affordable Care Act."
- Park, Madison (July 19, 2011). "Birth control should be fully covered under health plans, report says". CNN. http://www.cnn.com/2011/HEALTH/07/19/birth.control.iom/index.html. Retrieved August 27, 2012.
- "Provisions of the Affordable Care Act, By Year". HealthCare.gov. Archived from the original on September 9, 2011. https://web.archive.org/web/20110909133159/http://www.healthcare.gov/law/about/order/byyear.html. Retrieved January 9, 2012.
- "Key Features of the Affordable Care Act By Year". HHS. June 7, 2013. https://www.hhs.gov/healthcare/facts/timeline/timeline-text.html#print. Retrieved June 7, 2013.
- Binckes, Jeremy; Wing, Nick (March 22, 2010). "The Top 18 Immediate Effects Of The Health Care Bill". The Huffington Post. http://www.huffingtonpost.com/2010/03/22/the-top-18-immediate-effe_n_508315.html#s75147. Retrieved March 22, 2010.
- "How do out-of-pocket maximums work?". Blue Cross Blue Shield of Michigan. http://www.bcbsm.com/index/health-insurance-help/faqs/topics/how-health-insurance-works/out-of-pocket-maximums.html.
- Bowman, Lee (March 22, 2010). "Health reform bill will cause several near-term changes". Scripps Howard News Service. Archived from the original on December 27, 2010. https://web.archive.org/web/20101227022643/http://public.shns.com/node/52359. Retrieved March 23, 2010.
- "Summary of the Affordable Care Act". Kaiser Family Foundation. April 23, 2013. Archived from the original on October 3, 2013. https://web.archive.org/web/20131003011827/http://kaiserfamilyfoundation.files.wordpress.com/2011/04/8061-021.pdf.
- "Health Insurance Market Reforms: Prevention". Centers for Medicare and Medicaid Services. December 21, 2010. https://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/Prevention.html. Retrieved September 8, 2013.
- "Next Steps to Comply with Health Care Reform". The National Law Review. October 10, 2012. http://www.natlawreview.com/article/next-steps-to-comply-health-care-reform. Retrieved October 10, 2012.
- "How do I choose Marketplace insurance?". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services. https://www.healthcare.gov/how-do-i-choose-marketplace-insurance.
- "Health Plan Categories". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services. https://www.healthcare.gov/glossary/health-plan-categories/.
- "Medical Loss Ratio". Centers for Medicaid and Medicare Services. http://www.cms.gov/CCIIO/Programs-and-Initiatives/Health-Insurance-Market-Reforms/Medical-Loss-Ratio.html. Retrieved October 2, 2013.
- "Medical Loss Ratio Requirements Under the Patient Protection and Affordable Care Act". Federal Register. December 7, 2011. p. 76573. http://www.gpo.gov/fdsys/granule/FR-2011-12-07/2011-31289/content-detail.html. Retrieved April 1, 2012.
- "Minimum Coverage Provision ("individual mandate")". American Public Health Association (APHA). Archived from the original on July 1, 2014. https://web.archive.org/web/20140701171554/http://www.apha.org/advocacy/Health+Reform/ACAbasics/MC_provision.htm.
- Cohn, Jonathan (August 5, 2013). "Burn Your Obamacare Card, Burn Yourself". The New Republic. https://newrepublic.com/article/114163/limited-enrollment-periods-obamacare-means-young-people-cant-wait.
- McClanahan, Carolyn (August 4, 2013). "Reader's Questions About Obamacare – Misinformation Abounds". Forbes. https://www.forbes.com/sites/carolynmcclanahan/2013/08/04/readers-questions-about-obamacare-misinformation-abounds. Retrieved August 15, 2013.
- Cohn, Jonathan (April 9, 2010). "Common Sense". The New Republic. https://newrepublic.com/article/health-care/why-americans-should-support-individual-mandate. Cohn, Jonathan (April 2, 2012). "What If the Mandate Goes?". The New Republic. https://newrepublic.com/blog/jonathan-cohn/102285/supreme-court-obamacare-mandate-severability-cbo. Cohn, Jonathan (December 26, 2011). "Was the Mandate a Mistake?". The New Republic. https://newrepublic.com/blog/jonathan-cohn/98928/individual-mandate-mistake-health-reform-starr-cbo-ppaca.
- "Cost Estimate for Pending Health Care Legislation". Congressional Budget Office. March 20, 2010. http://www.cbo.gov/sites/default/files/cbofiles/ftpdocs/113xx/doc11379/amendreconprop.pdf. Retrieved March 28, 2010.
- Chaikind, Hinda; Copeland, Curtis W.; Redhead, C. Stephen; Staman, Jennifer (March 2, 2011). PPACA: A Brief Overview of the Law, Implementation, and Legal Challenges. Congressional Research Service. R41664. http://www.nationalaglawcenter.org/wp-content/uploads/assets/crs/R41664.pdf. Retrieved December 22, 2013.
- Trumbull, Mark (March 23, 2010). "Obama signs health care bill: Who won't be covered?". The Christian Science Monitor. http://www.csmonitor.com/USA/2010/0323/Obama-signs-health-care-bill-Who-won-t-be-covered. Retrieved March 24, 2010.
- Fox, Emily Jane (July 24, 2012). "6 million will lose out on Medicaid expansion". CNNMoney. http://money.cnn.com/2012/07/23/news/economy/health-reform. Retrieved July 25, 2012.
- Hatch, Orrin (December 20, 2017). "Sen. Orrin Hatch: Repealing the individual mandate tax is the beginning of the end of the ObamaCare era". Fox News. http://www.foxnews.com/opinion/2017/12/20/sen-orrin-hatch-repealing-individual-mandate-tax-is-beginning-end-obamacare-era.html. Retrieved December 21, 2017.
- "The Effect of Eliminating the Individual Mandate Penalty and the Role of Behavioral Factors | Commonwealth Fund". https://www.commonwealthfund.org/publications/fund-reports/2018/jul/eliminating-individual-mandate-penalty-behavioral-factors.
- "Explaining Health Care Reform: Questions About Health Insurance Subsidies". Kaiser Family Foundation. July 1, 2012. http://kff.org/health-costs/issue-brief/explaining-health-care-reform-questions-about-health/. Retrieved July 1, 2012.
- Luhby, Tami (April 23, 2013). "Millions eligible for Obamacare subsidies, but most don't know it". CNNMoney. http://money.cnn.com/2013/04/23/news/economy/obamacare-subsidies/index.html. Retrieved June 22, 2013.
- "Explaining Health Care Reform". Kaiser Family Foundation. http://kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/.
- Fehr, Rachel; Mar 05, Gary Claxton Published; 2019 (March 5, 2019). "How Affordable are 2019 ACA Premiums for Middle-Income People?" (in en-US). https://www.kff.org/health-reform/issue-brief/how-affordable-are-2019-aca-premiums-for-middle-income-people/.
- Nov 20, Published; 2018 (November 20, 2018). "Explaining Health Care Reform: Questions About Health Insurance Subsidies" (in en-us). https://www.kff.org/health-reform/issue-brief/explaining-health-care-reform-questions-about-health/.
- Congress, United States. "Patient Protection and Affordable Care Act". https://en.wikisource.org/wiki/Patient_Protection_and_Affordable_Care_Act/Title_I/Subtitle_E/Part_I/Subpart_A.
- Patient Protection and Affordable Care Act: Title I: Subtitle E: Part I: Subpart A: Premium Calculation
- Research, UC Berkeley Center for Labor; Education (July 1, 2014). "Modified Adjusted Gross Income under the Affordable Care Act" (in en-US). http://laborcenter.berkeley.edu/modified-adjusted-gross-income-under-the-affordable-care-act/.
- "Small Business Health Care Tax Credit and the SHOP Marketplace". Internal Revenue Service. October 20, 2016. https://www.irs.gov/affordable-care-act/employers/small-business-health-care-tax-credit-and-the-shop-marketplace. Retrieved January 11, 2017.
- "Welcome to the Marketplace". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services. https://www.healthcare.gov/marketplace/individual/. "What is the Health Insurance Marketplace?". HealthCare.Gov, managed by the Centers for Medicare and Medicaid Services. https://www.healthcare.gov/what-is-the-health-insurance-marketplace.
- "Insurance Exchanges". American Public Health Association (APHA). Archived from the original on August 1, 2013. https://web.archive.org/web/20130801135757/http://www.apha.org/advocacy/Health+Reform/ACAbasics/insurance.htm.
- Cohn, Jonathan (April 29, 2013). "Obamacare Sticker Shock: Not Very Shocking". The New Republic. https://newrepublic.com/article/112259/obamacare-sticker-shock-not-very-shocking.
- "Paper MA ACA application (for the MA Health Connector, the state exchange)". August 10, 2019. https://www.mass.gov/files/documents/2019/06/28/aca-3-english.pdf.
- "MN ACA application (MNSURE, their state exchange)". August 10, 2019. https://edocs.dhs.state.mn.us/lfserver/Public/DHS-6696-ENG.
- "State Decisions For Creating Health Insurance Exchanges, as of May 28, 2013 – Notes". Kaiser Family Foundation. May 28, 2013. http://kff.org/health-reform/state-indicator/health-insurance-exchanges/#notes.
- "State Health Insurance Exchange Laws: The First Generation". The CommonWealth Fund. July 25, 2012. http://www.commonwealthfund.org/Publications/Issue-Briefs/2012/Jul/State-Health-Insurance-Exchange-Laws.aspx?omni.
- Adams, Rebecca (July 22, 2013). "The Question of Abortion Coverage in Health Exchanges". Roll Call. http://www.rollcall.com/news/the_question_of_abortion_coverage_in_health_exchanges-226547-1.html.
- "Federal Subsidies for Health Insurance Coverage for People Under Age 65: 2017 to 2027". Center on Budget and Policy Priorities. September 14, 2017. https://www.cbo.gov/publication/53091
- Legislative Attorneys, American Law Division (January 5, 2016), Lawsuits to Recover Payments under the Risk Corridors Program of the Affordable Care Act, Congressional Research Service, p. 6, http://www.rubio.senate.gov/public/_cache/files/1dc92ef8-c340-4cfd-95c0-67369a557f1e/2AA5EF8F125279800BFABC8B8BA37072.05.24.2016-crs-rubio-memo-risk-corridors-1-5-16-1-redacted.pdf, retrieved February 11, 2017
- Nicholas Bagley (November 24, 2016), "Trouble on the Exchanges – Does the United States Owe Billions to Health Insurers?", New England Journal of Medicine 375 (21): 2017–2019, doi:10.1056/NEJMp1612486, PMID 27959725 https://dx.doi.org/10.1056%2FNEJMp1612486
- Risk Corridors and Budget Neutrality, Washington, DC: Centers for Medicare & Medicaid Services (CMS), April 11, 2014, https://www.cms.gov/CCIIO/Resources/Fact-Sheets-and-FAQs/Downloads/faq-risk-corridors-04-11-2014.pdf Department of Health and Human Services
- "Yes, Marco Rubio Led The Effort To End Obamacare's Health", Forbes, December 15, 2015, https://www.forbes.com/.../yes-marco-rubio-led-the-effort-to-end-obamacares-health-insuran..., retrieved February 10, 2017
- Kessler, Glenn (December 23, 2015). "Rubio's inaccurate claim that he 'inserted' a provision restricting Obamacare 'bailout' funds". The Washington Post. https://www.washingtonpost.com/news/fact-checker/wp/2015/12/23/rubios-inaccurate-claim-that-he-inserted-a-provision-restricting-obamacare-bailout-funds/.
- Michael Hiltzik (February 10, 2017), With billions at stake, a federal judge just nullified the GOP's most cynical attack on Obamacare, LA Times, http://www.latimes.com/business/hiltzik/la-fi-hiltzik-risk-corridor-moda-20170210-story.html, retrieved February 10, 2017
- Moda Health Plan, Inc. v. The United States, US Courts, February 10, 2017, pp. 40, https://ecf.cofc.uscourts.gov/cgi-bin/show_public_doc?2016cv0649-23-0, retrieved February 10, 2017
- "Maine Community Health Options v. United States" (in en). https://www.scotusblog.com/case-files/cases/maine-community-health-options-v-united-states/.
- Semanskee, Ashley; Claxton, Gary; 2016 (August 17, 2016). "Explaining Health Care Reform: Risk Adjustment, Reinsurance, and Risk Corridors" (in en-US). https://www.kff.org/health-reform/issue-brief/explaining-health-care-reform-risk-adjustment-reinsurance-and-risk-corridors/.
- HHS Press Office (March 29, 2013). "HHS finalizes rule guaranteeing 100 percent funding for new Medicaid beneficiaries". Washington, D.C.: U.S. Department of Health & Human Services. https://www.hhs.gov/news/press/2013pres/03/20130329a.html. Retrieved April 23, 2013. "effective January 1, 2014, the federal government will pay 100 percent of defined cost of certain newly eligible adult Medicaid beneficiaries. These payments will be in effect through 2016, phasing down to a permanent 90 percent matching rate by 2020." Centers for Medicare & Medicaid Services (April 2, 2013). "Medicaid program: Increased federal medical assistance percentage changes under the Affordable Care Act of 2010: Final rule". Federal Register 78 (63): 19917–19947. "(A) 100 percent, for calendar quarters in calendar years (CYs) 2014 through 2016; (B) 95 percent, for calendar quarters in CY 2017; (C) 94 percent, for calendar quarters in CY 2018; (D) 93 percent, for calendar quarters in CY 2019; (E) 90 percent, for calendar quarters in CY 2020 and all subsequent calendar years.".
- "Archive-It - News Releases". https://www.hhs.gov/news/press/2013pres/03/20130329a.html.
- "How Health Reform's Medicaid Expansion Will Impact State Budgets". July 11, 2012. https://www.cbpp.org/research/how-health-reforms-medicaid-expansion-will-impact-state-budgets.
- "Medicaid Expansion". Is Medicaid eligibility expanding to 133 or 138 percent FPL, and what is MAGI?: American Public Health Association (APHA). http://www.apha.org/APHA/CMS_Templates/GeneralArticle.aspx?NRMODE=Published&NRNODEGUID=%7bD5E1C04A-0438-4FD4-A423-CEFDA0D9878D%7d&NRORIGINALURL=%2fadvocacy%2fHealth%2bReform%2fACAbasics%2fmedicaid%2ehtm. Retrieved July 24, 2013.
- "Affordable Care Act Update: Implementing Medicare Cost Savings". Centers for Medicare and Medicaid Services. August 2, 2010. Archived from the original on April 18, 2013. https://web.archive.org/web/20130418015959/http://www.cms.gov/apps/docs/aca-update-implementing-medicare-costs-savings.pdf. Retrieved October 7, 2013.
- Higher Spending Relative to Medicare Fee-for-Service May Not Ensure Lower Out-of-Pocket Costs for Beneficiaries. Government Accountability Office. February 8, 2008. http://www.gao.gov/products/GAO-08-522T. Retrieved October 7, 2013.
- "PPACA, section 9015 as modified by section 10906". http://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr/pdf/BILLS-111hr3590enr.pdf.
- "HCERA section 1402". http://www.gpo.gov/fdsys/pkg/BILLS-111hr4872enr/pdf/BILLS-111hr4872enr.pdf.
- Nowak, Sarah; Eibner, Christine (December 18, 2015). "Rethinking the Affordable Care Act's "Cadillac Tax": A More Equitable Way to Encourage "Chevy" Consumption". Commonwealth Fund. http://www.commonwealthfund.org/publications/issue-briefs/2015/dec/aca-cadillac-tax.
- "Briefing Book". Tax Policy Center. http://www.taxpolicycenter.org/briefing-book/what-are-major-federal-excise-taxes-and-how-much-money-do-they-raise.
- "Where are States Today? Medicaid and CHIP Eligibility Levels for Children and Non-Disabled Adults". Kaiser Family Foundation. March 28, 2013. http://kff.org/medicaid/fact-sheet/where-are-states-today-medicaid-and-chip.
- H.R. 3590 Enrolled, section 1001 (adding section 2714 to the Public Health Service Act): "A group health plan and a health insurance issuer offering group or individual health insurance coverage that provides dependent coverage of children shall continue to make such coverage available for an adult child (who is not married) until the child turns 26 years of age." https://www.gpo.gov/fdsys/pkg/BILLS-111hr3590enr
- "Young Adults and the Affordable Care Act". Archived from the original on November 11, 2016. https://web.archive.org/web/20161111074656/https://www.whitehouse.gov/sites/default/files/rss_viewer/fact_sheet_young_adults_may10.pdf.
- "Explaining Health Care Reform: What is Employer "Pay-or-Play" Requirement?". Kaiser Family Foundation. May 1, 2009. http://kff.org/health-costs/issue-brief/explaining-health-care-reform-what-is-an/. Retrieved January 9, 2012.
- McNamara, Kristen (March 25, 2010). "What Health Overhaul Means for Small Businesses". The Wall Street Journal. https://www.wsj.com/articles/SB10001424052748703312504575141533342803608.
- Cohn, Jonathan (May 21, 2013). "Weaseling Out of Obamacare". The New Republic. https://newrepublic.com/article/113257/low-wage-employers-try-avoid-obamacare-mandate.
- Chait, Jonathan (May 29, 2013). "Yuval Levin Dissembles Madly". New York. http://nymag.com/daily/intelligencer/2013/05/yuval-levin-dissembles-madly.html.
- "Access". http://www.medscape.com/viewarticle/748502. Retrieved January 9, 2012. (registration required)
- "Key Healthcare Reform Initiatives: Medicare Bundled Payment Pilots". Huron Consulting Group. November 19, 2010. http://www.huronconsultinggroup.com/researchdetails.aspx?articleId=2577. Retrieved January 9, 2012.
- "More savings in the drug coverage gap coming through 2020". Centers for Medicare & Medicaid Services. http://www.medicare.gov/part-d/costs/coverage-gap/more-drug-savings-in-2020.html. Retrieved September 27, 2013.
- https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about.html
- "Accountable Care Organizations, Explained" (in en-US). Kaiser Health News. September 14, 2015. http://khn.org/news/aco-accountable-care-organization-faq/. Retrieved August 18, 2016.
- "What the Affordable Care Act means for prescription coverage". https://www.washingtonpost.com/sf/brand-connect/wp/2014/03/17/what-the-affordable-care-act-means-for-prescription-coverage/. Retrieved August 7, 2016.
- "Closing the Coverage Gap – Medicare Prescription Drugs Are Becoming More Affordable". CMS. January 2015. Archived from the original on May 23, 2013. https://web.archive.org/web/20130523191556/http://www.medicare.gov/Publications/Pubs/pdf/11493.pdf.
- "Public Law 111 – 148, section 1332". Government Printing Office. http://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm. Retrieved June 29, 2012.
- "Preparing for Innovation: Proposed Process for States to Adopt Innovative Strategies to Meet the Goals of the Affordable Care Act". U.S. Department of Health & Human Services. November 16, 2011. http://www.healthcare.gov/news/factsheets/stateinnovation03102011a.html. Retrieved April 1, 2012.
- Goldstein, Amy; Balz, Dan (March 1, 2011). "Obama offers states more flexibility in health-care law". The Washington Post. https://www.washingtonpost.com/wp-dyn/content/article/2011/02/28/AR2011022806535.html.
- Span, Paula (March 29, 2010). "Options Expand for Affordable Long-Term Care". The New York Times. https://www.nytimes.com/2010/03/30/health/30care.html. Retrieved March 29, 2010.
- PriceWaterHouseCoopers. "The CLASS Act". HRS Insight: Human Resource Services. 2010: 1–6. Web.
- Carney, Timothy (February 28, 2011) So, yeah, the health-care bill was really an awful piece of legislation that sent the revolving door spinning faster, Washington Examiner http://washingtonexaminer.com/blogs/beltway-confidential/2011/02/so-yeah-health-care-bill-was-really-awful-piece-legislation-sent-
- "Watchdogs: CLASS still dead". LifeHealthPro. January 2, 2013. http://www.lifehealthpro.com/2013/01/02/watchdogs-class-still-dead.
- Medicare, Centers for; Baltimore, Medicaid Services 7500 Security Boulevard; Usa, Md21244 (May 8, 2013). "Consumer Operated and Oriented Plan Program". https://www.cms.gov/CCIIO/Programs-and-Initiatives/Insurance-Programs/Consumer-Operated-and-Oriented-Plan-Program.html.
- "Montana CO-OP, 1 of just 4 left, returns from hiatus with high hopes" (in en). https://www.fiercehealthcare.com/payer/one-just-four-co-ops-left-montana-insurer-returns-from-hiatus-high-hopes.
- "Affordable Care Act's calorie count rules go into effect". May 7, 2018. https://wreg.com/2018/05/07/affordable-care-acts-calorie-count-rules-go-into-effect/.
- Roy, Avik (February 7, 2012). "The Tortuous History of Conservatives and the Individual Mandate". Forbes Magazine. https://www.forbes.com/sites/aroy/2012/02/07/the-tortuous-conservative-history-of-the-individual-mandate.
- Butler, Stuart M. (1989). "Assuring Affordable Healthcare for All Americans". The Heritage Foundation. http://healthcarereform.procon.org/sourcefiles/1989_assuring_affordable_health_care_for_all_americans.pdf.
- Cohn, Jonathan (April 9, 2010). "Common Sense". The New Republic. https://newrepublic.com/article/health-care/why-americans-should-support-individual-mandate.
- Cooper, Michael (February 14, 2012). "Conservatives Sowed Idea of Health Care Mandate, Only to Spurn It Later". The New York Times. https://www.nytimes.com/2012/02/15/health/policy/health-care-mandate-was-first-backed-by-conservatives.html. Retrieved July 2, 2012.
- Klein, Ezra (June 25, 2012). "Unpopular Mandate". The New Yorker. http://www.newyorker.com/reporting/2012/06/25/120625fa_fact_klein. Retrieved June 19, 2012.
- Cooper, Michael (February 14, 2012). "Conservatives Sowed Idea of Health Care Mandate, Only to Spurn It Later". The New York Times . Retrieved July 2, 2012. https://www.nytimes.com/2012/02/15/health/policy/health-care-mandate-was-first-backed-by-conservatives.html
- Cohn, Bob; Clift, Eleanor (September 18, 1994). "The Lost Chance". Newsweek. Retrieved July 2, 2012. http://www.newsweek.com/lost-chance-188330
- Fouhy, Beth (October 5, 2007). "Hillary Claims Credit for Child Program". Associated Press for NewsMax. Archived from the original on January 23, 2008. https://web.archive.org/web/20080123174618/http://www.newsmax.com/insidecover/hillary_health_care/2007/10/05/38601.html.
- "Chart: Comparing Health Reform Bills: Democrats and Republicans 2009, Republicans 1993". Kaiser Health News. February 23, 2010. http://www.kaiserhealthnews.org/Graphics/2010/022310-Bill-comparison.aspx. Retrieved July 29, 2012. "Summary Of A 1993 Republican Health Reform Plan". Kaiser Health News. February 23, 2010. http://www.kaiserhealthnews.org/Stories/2010/February/23/GOP-1993-health-reform-bill.aspx. Retrieved July 29, 2012.
- "In 1993, Republicans Proposed A Mandate First". NPR. March 31, 2012. https://www.npr.org/2012/03/31/149767150/in-1993-republicans-proposed-a-mandate-first.
- "History of the Individual Health Insurance Mandate, 1989–2010 Republican Origins of Democratic Health Care Provision". ProCon.org. February 9, 2012. http://healthcarereform.procon.org/view.resource.php?resourceID=004182.
- "AG Suthers couldn't be more wrong in his decision to file lawsuit". http://www.coloradostatesman.com/content/991732-ag-suthers-couldn%3Ft-be-more-wrong-his-decision-file-lawsuit. Retrieved July 29, 2012.
- "G.O.P. and Health Mandate". The New York Times. February 26, 2012. https://www.nytimes.com/2012/02/27/opinion/gop-and-health-mandate.html?_r=2&adxnnl=1&adxnnlx=1333652503-360xnkv/rpzNURZGZh5Vdw.
- "Romneycare's 98% Success Rate Defies Gripes on Obama Law". Bloomberg. March 26, 2012. https://www.bloomberg.com/news/2012-03-26/romneycare-s-98-success-rate-defies-gripes-on-obama-law.html.
- Ball, Molly (May 31, 2012). "Was Mitt Romney a Good Governor?". The Atlantic. https://www.theatlantic.com/politics/archive/2012/05/was-mitt-romney-a-good-governor/257942. Retrieved October 28, 2013.
- Lizza, Ryan (June 6, 2011). "Romney's dilemma". The New Yorker. http://www.newyorker.com/reporting/2011/06/06/110606fa_fact_lizza. Retrieved June 19, 2012.
- "Bill Summary & Status – S.334". Library of Congress THOMAS. http://thomas.loc.gov/cgi-bin/bdquery/z?d110:SN00334:@@@S. Retrieved September 24, 2013.
- Kuttner, Robert (June 28, 2011). "RomneyCare vs. ObamaCare". The Boston Globe. http://www.boston.com/bostonglobe/editorial_opinion/oped/articles/2011/06/28/romneycare_vs_obamacare. Retrieved September 23, 2013.
- Cline, Andrew. "How Obama Broke His Promise on Individual Mandates". The Atlantic. https://www.theatlantic.com/politics/archive/2012/06/how-obama-broke-his-promise-on-individual-mandates/259183/. Retrieved September 26, 2013.
- "CNN Democratic presidential debate". CNN. January 21, 2008. http://www.cnn.com/2008/POLITICS/01/21/debate.transcript2/. Retrieved September 26, 2013.
- "The First Presidential Debate". The New York Times. September 26, 2008. http://elections.nytimes.com/2008/president/debates/transcripts/first-presidential-debate.html.
- Rustgi, Sheila; Collins, Sara R.; Davis, Karen; Nicholson, Jennifer L. (in en). The 2008 Presidential Candidates' Health Reform Proposals: Choices for America. http://www.commonwealthfund.org/publications/fund-reports/2008/oct/the-2008-presidential-candidates-health-reform-proposals--choices-for-america.
- "Remarks of President Barack Obama – Address to Joint Session of Congress". The White House. February 24, 2009. Archived from the original on March 8, 2010. https://web.archive.org/web/20100308180312/http://www.whitehouse.gov/the-press-office/remarks-president-barack-obama-address-joint-session-congress. Retrieved March 24, 2010.
- "Timeline: Milestones in Obama's quest for healthcare reform". Reuters. March 22, 2010. https://www.reuters.com/article/idUSTRE62L0JA20100322. Retrieved March 22, 2010.
- Kruger, Mike (October 29, 2009). "Affordable Health Care for America Act". United States House Committee on Education and Labor. Archived from the original on January 6, 2010. https://web.archive.org/web/20100106013943/http://edlabor.house.gov/blog/2009/10/affordable-health-care.shtml. Retrieved March 24, 2010.
- "Health Care Reform from Conception to Final Passage". http://finance.senate.gov/issue/?id=32be19bd-491e-4192-812f-f65215c1ba65. Retrieved November 23, 2010.
- "Senate Finance Committee Hearings for the 111th Congress recorded by C-SPAN". C-SPAN. http://www.c-spanvideo.org/videoLibrary/search-results.php?organization=%22Finance%22&organization=%22Senate+Committee%22&date-from=01%2F06%2F2009&date-to=01%2F02%2F2011.
- "Senate Finance Committee hearings for 111th Congress". Finance.Senate.Gov. Archived from the original on January 11, 2013. https://web.archive.org/web/20130111185729/http://www.finance.senate.gov/hearings/index.cfm?PageNum_rs=1&maxrows=100. Retrieved April 1, 2012.
- "Jonathan Gruber (economist)". MIT Department of Economics. http://economics.mit.edu/faculty/gruberj. Retrieved September 2, 2013. "Jonathan Gruber: short biography". MIT Department of Economics. Archived from the original on September 28, 2013. https://web.archive.org/web/20130928032016/http://economics.mit.edu/files/7840. Retrieved September 2, 2013.
- Cohn, Jonathan (May 21, 2010). "How They Did It". The New Republic. https://newrepublic.com/article/75077/how-they-did-it.
- Cohn, Jonathan (September 4, 2009). "Party Is Such Sweet Sorrow". The New Republic. https://newrepublic.com/article/health-care/party-is-such-sweet-sorrow.
- Chait, Jonathan (April 22, 2010). "Obama's Moderate Health Care Plan". The New Republic. https://newrepublic.com/blog/jonathan-chait/obamas-moderate-health-care-plan. Chait, Jonathan (December 19, 2009). "The Republican Health Care Blunder". The New Republic. https://newrepublic.com/blog/the-plank/the-republican-health-care-blunder.
- Chait, Jonathan (December 19, 2009). "The Republican Health Care Blunder". The New Republic. https://newrepublic.com/blog/the-plank/the-republican-health-care-blunder.
- Eaton, Joe; Pell, M. B.; Mehta, Aaron (March 26, 2010). "Lobbying Giants Cash In On Health Overhaul". NPR. https://www.npr.org/templates/story/story.php?storyId=125170643. Retrieved April 9, 2012.
- Cohn, Jonathan (August 25, 2009). "Drug Deal". The New Republic. https://newrepublic.com/article/politics/drug-deal.
- Grim, Ryan (August 13, 2009). "Internal Memo Confirms Big Giveaways In White House Deal With Big Pharma". The Huffington Post. http://www.huffingtonpost.com/2009/08/13/internal-memo-confirms-bi_n_258285.html.
- "Visualizing The Health Care Lobbyist Complex". Sunlight Foundation. July 22, 2009. http://sunlightfoundation.com/projects/2009/healthcare_lobbyist_complex. Retrieved April 1, 2012.
- Horwitz, Sari; Pershing, Ben (April 9, 2010). "Anger over health-care reform spurs rise in threats against Congress members". The Washington Post. https://www.washingtonpost.com/wp-dyn/content/article/2010/04/08/AR2010040805476.html?nav=hcmodule. Retrieved April 9, 2010.
- "Remarks by the President to a Joint Session of Congress on Health Care". The White House. September 10, 2009. Archived from the original on March 8, 2010. https://web.archive.org/web/20100308000433/http://www.whitehouse.gov/the-press-office/remarks-president-a-joint-session-congress-health-care. Retrieved March 24, 2010.
- U.S. Const. art. I, § 7, cl. 1.
- "Summary: H.R.3590—111th Congress (2009–2010)". Library of Congress. July 30, 2017. https://www.congress.gov/bill/111th-congress/house-bill/3590/summary/81.
- S.Amdt. 2786 https://www.congress.gov/amendment/111th-congress/senate-amendment/2786
- Cohn, Jonathan (September 7, 2009). "Why Reform Survived August". The New Republic. https://newrepublic.com/blog/the-treatment/why-reform-survived-august.
- Hacker, Jacob S. (December 20, 2009). "Why I Still Believe in This Bill". The New Republic. https://newrepublic.com/blog/the-treatment/why-i-still-believe-bill.
- Cohn, Jonathan (March 12, 2010). "The Public Option, Still Dead". The New Republic. https://newrepublic.com/blog/the-treatment/the-public-option-still-dead.
- Cohn, Jonathan (December 15, 2009). "What Public Option Supporters Won". The New Republic. https://newrepublic.com/blog/the-treatment/what-public-option-supporters-won.
- Cohn, Jonathan (December 17, 2009). "Ben Nelson, Still a Big Problem (Updated)". The New Republic. https://newrepublic.com/blog/the-treatment/ben-nelson-still-big-problem.
- Cohn, Jonathan (December 19, 2009). "Nelson Says Yes; That Makes 60". The New Republic. https://newrepublic.com/blog/the-treatment/breaking-nelson-says-yes-makes-60.
- "'Cornhusker' Out, More Deals In: Health Care Bill Gives Special Treatment". Fox News. March 19, 2010. http://www.foxnews.com/politics/2010/03/18/cornhusker-kickback-gets-boot-health. Retrieved April 26, 2010.
- "Roll Call vote No. 395 – On the Cloture Motion (Motion to Invoke Cloture on H.R. 3590)". U.S. Senate. https://www.senate.gov/legislative/LIS/roll_call_lists/roll_call_vote_cfm.cfm?congress=111&session=1&vote=00395. Retrieved July 20, 2017.
- "Roll Call vote No. 396 – On Passage of the Bill (H.R. 3590 as Amended)". U.S. Senate. https://www.senate.gov/legislative/LIS/roll_call_lists/roll_call_vote_cfm.cfm?congress=111&session=1&vote=00396. Retrieved January 9, 2012.
- "AARP, AMA Announce Support For Health Care Bill: Largest Doctors And Retiree Groups Backing Legislation". The Huffington Post, March 19, 2010. http://www.huffingtonpost.com/2010/03/19/aarp-ama-announce-support_n_506060.html
- Applewhite, J. Scott. "Senator-elect Scott Brown welcomed as Republican hero after upset victory in Massachusetts". Associated Press. McClatchy-Tribune News Service. http://www.cleveland.com/nation/index.ssf/2010/01/senator-elect_scott_brown_welc.html. Retrieved April 19, 2012.
- "Public Statements – Project Vote Smart" (Press release). Votesmart.org. January 13, 2010. Retrieved April 9, 2012. http://www.votesmart.org/public-statement/477580/scott-brown-responds-to-martha-coakleys-misleading-health-care-distortions
- Silver, Nate (January 21, 2010). "Will the Base Abandon Hope?". FiveThirtyEight. http://www.fivethirtyeight.com/2010/01/will-base-abandon-hope.html.
- Cohn, Jonathan (January 17, 2010). "How to Pass the Bill--Whatever Happens Tuesday". The New Republic. https://newrepublic.com/blog/the-treatment/what-do-if-coakley-loses-contd.
- Stolberg, Sheryl; Zeleny, Jeff; Hulse, Carl (March 20, 2010). "Health Vote Caps a Journey Back From the Brink". The New York Times. https://www.nytimes.com/2010/03/21/health/policy/21reconstruct.html. Retrieved March 23, 2010.
- Brown, Carrie; Thrush, Glenn (March 20, 2010). "Pelosi steeled W.H. for health push". Politico. http://www.politico.com/news/stories/0310/34753.html. Retrieved March 23, 2010.
- "White House Unveils Revamped Reform Plan, GOP And Industry React". Kaiser Health News. February 22, 2010. http://www.kaiserhealthnews.org/Daily-Reports/2010/February/22/President-Obama-Health-Care-Reform-Plan.aspx. Retrieved June 29, 2012.
- Chait, Jonathan (February 20, 2010). "A Brief Reconciliation Primer". The New Republic. https://newrepublic.com/blog/jonathan-chait/brief-reconciliation-primer.
- Silver, Nate (December 26, 2009). "For Pelosi, Many Paths to 218". FiveThirtyEight. http://www.fivethirtyeight.com/2009/12/in-house-many-paths-to-218.html.
- Silver, Nate (January 21, 2010). "1. Reconciliation! 2. ??? 3. Profit!". FiveThirtyEight. http://www.fivethirtyeight.com/2010/01/1-reconciliation-2-3-profit.html.
- Cohn, Jonathan (September 21, 2009). "Reconciliation: Why Most Dems Don't Want to Go There". The New Republic. https://newrepublic.com/blog/the-treatment/reconciliation-why-most-dems-dont-want-go-there.
- Executive Order 13535 of March 24, 2010—Ensuring Enforcement and Implementation of Abortion Restrictions in the Patient Protection and Affordable Care Act, Vol. 75, No. 59 75 FR 15599, March 29, 2010. https://www.federalregister.gov/citation/75-FR-15599
- Chait, Jonathan (March 21, 2010). "Stupak Makes A Deal, Reform To Pass". The New Republic. https://newrepublic.com/blog/jonathan-chait/stupak-makes-deal-reform-pass.
- "Roll Call vote No. 165: On Motion to Concur in Senate Amendments (Patient Protection and Affordable Care Act)". Office of the Clerk: House of Representatives. March 21, 2010. http://clerk.house.gov/evs/2010/roll165.xml. Retrieved April 9, 2012.
- Aro, Margaret; Mooney, Mark (March 22, 2010). "Pelosi Defends Health Care Fight Tactics". ABC News. https://abcnews.go.com/WN/Politics/house-speaker-nancy-pelosis-exclusive-interview-diane-sawyer/story?id=10172685. Retrieved March 23, 2010.
- Stolberg, Sheryl; Pear, Robert (March 23, 2010). "Obama Signs Health Care Overhaul Bill, With a Flourish". The New York Times. https://www.nytimes.com/2010/03/24/health/policy/24health.html. Retrieved March 24, 2010.
- Benen, Steve (February 2, 2016). "On Groundhog Day, Republicans vote to repeal Obamacare". MSNBC. http://www.msnbc.com/rachel-maddow-show/groundhog-day-republicans-vote-repeal-obamacare.
- Erb, Kelly Phillips (December 20, 2019). "Congress Passes Bill Chock-Full Of Extenders, Healthcare Tax Repeal & Retirement Plan Tweaks" (in en). https://www.forbes.com/sites/kellyphillipserb/2019/12/20/congress-passes-bill-chock-full-of-extenders-healthcare-tax-repeal--retirement-plan-tweaks/.
- "Federal Subsidies for Health Insurance Coverage for People Under Age 65:2016 to 2026". https://www.cbo.gov/publication/51385. Retrieved November 23, 2016.
- "National Health Interview Survey, January to June 2016". https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201611_01.pdf. Retrieved November 23, 2016.
- Barry-Jester, Anna Maria; Ben, Casselman (September 22, 2016). "Obamacare Has Increased Insurance Coverage Everywhere". FiveThirtyEight. http://fivethirtyeight.com/features/obamacare-has-increased-insurance-coverage-everywhere/. Retrieved October 12, 2016.
- "Health Insurance Coverage and the Affordable Care Act, 2010–2016". March 2, 2016. https://aspe.hhs.gov/pdf-report/health-insurance-coverage-and-affordable-care-act-2010-2016. Retrieved December 7, 2016.
- Garrett, Bowen (December 2016). "Who Gained Health Insurance Coverage Under the ACA, and Where Do They Live?". Urban Institute. pp. 2. http://www.urban.org/sites/default/files/publication/86761/2001041-who-gained-health-insurance-coverage-under-the-aca-and-where-do-they-live.pdf. Retrieved April 22, 2017.
- "Health Reform Monitoring Survey". http://hrms.urban.org/briefs/health-insurance-coverage-ACA-March-2016.html. Retrieved December 5, 2016.
- "Current Status of State Medicaid Expansion Decisions". http://kff.org/health-reform/slide/current-status-of-the-medicaid-expansion-decision/. Retrieved December 5, 2016.
- Griffith, Kevin; Evans, Leigh; Bor, Jacob (August 1, 2017). "The Affordable Care Act Reduced Socioeconomic Disparities In Health Care Access". Health Affairs 36 (8): 1503–1510. doi:10.1377/hlthaff.2017.0083. ISSN 0278-2715. PMID 28747321. https://dx.doi.org/10.1377%2Fhlthaff.2017.0083
- Slavitt, Andy (March 23, 2020). "Affordable Care Act at 10: Amid coronavirus, never more popular, threatened or necessary". USA Today. Archived from the original on March 31, 2020. https://web.archive.org/web/20200331233236/https://www.usatoday.com/story/opinion/2020/03/23/obamacare-10th-anniversary-amid-coronavirus-column/2888511001/. Retrieved March 31, 2020.
- Abby Goodnough, Reed Abelson, Margot Sanger-Katz and Sarah Kliff (March 23, 2020). "Obamacare Turns 10. Here's a Look at What Works and Doesn't.". The New York Times. Archived from the original on March 30, 2020. https://web.archive.org/web/20200330105840/https://www.nytimes.com/2020/03/23/health/obamacare-aca-coverage-cost-history.html. Retrieved March 31, 2020.
- Caplinger, Dan (January 7, 2018). "What the Individual Mandate Repeal Means for the Average American -". https://www.fool.com/taxes/2018/01/07/what-the-individual-mandate-repeal-means-for-the-a.aspx.
- "What tax changes did the Affordable Care Act make?". https://www.taxpolicycenter.org/briefing-book/what-tax-changes-did-affordable-care-act-make.
- "The Economic Record of the Obama Administration: Progress Reducing Inequality". Archived from the original on November 26, 2016. https://web.archive.org/web/20161126124328/https://www.whitehouse.gov/sites/default/files/page/files/20160923_record_inequality_cea.pdf. Retrieved December 6, 2016.
- Nussbaum, Alex (March 4, 2015). "Health Insurance Exchanges". https://www.bloomberg.com/view/quicktake/health-insurance-exchanges. Retrieved August 12, 2016.
- "The Marketplace in your state" (in en). https://www.healthcare.gov/marketplace-in-your-state/.
- "Status of State Action on the Medicaid Expansion Decision, as of September 1, 2015". Kaiser Family Foundation. June 22, 2015. https://www.kff.org/health-reform/slide/current-status-of-the-medicaid-expansion-decision/.
- "Health Insurance Coverage in the United States: 2018". September 10, 2019. https://www.census.gov/library/publications/2019/demo/p60-267.html.
- Robert Pear (May 24, 2013). "States' Policies on Health Care Exclude Some of the Poorest". The New York Times. https://www.nytimes.com/2013/05/25/us/states-policies-on-health-care-exclude-poorest.html. Retrieved May 25, 2013. "In most cases, [Sandy Praeger, Insurance Commissioner of Kansas], said adults with incomes from 32 percent to 100 percent of the poverty level ($6,250 to $19,530 for a family of three) "will have no assistance"."
- "Cost of Obamacare Medicaid Expansion 49% Higher Than Previously Estimated". August 12, 2016. http://www.cnsnews.com/news/article/medicaid-estimate-renews-cost-concerns-over-obamacare. Retrieved August 13, 2016.
- "The Impact of the Coverage Gap for Adultsin States not Expanding Medicaid". October 26, 2015. http://kff.org/disparities-policy/issue-brief/the-impact-of-the-coverage-gap-in-states-not-expanding-medicaid-by-race-and-ethnicity/.
- Kliff, Sarah (July 5, 2012). "What Happens if a State Opts Out of Medicaid, in One Chart". The Washington Post. https://www.washingtonpost.com/blogs/ezra-klein/wp/2012/07/05/what-happens-if-a-state-opts-out-of-medicaid-in-one-chart. Retrieved July 15, 2012.
- "Health Reform and MedicaidExpansion". HealthCare Reform Magazine. July 13, 2010. http://www.healthcarereformmagazine.com/article/health-reform-and-medicaid-expansion.html. Retrieved January 9, 2012.
- "Analyzing the Impact of State Medicaid Expansion Decisions". Kaiser Family Foundation. July 17, 2013. http://kff.org/medicaid/issue-brief/analyzing-the-impact-of-state-medicaid-expansion-decisions/.
- "Enrollment Policy Provisions in the Patient Protection and Affordable Care Act". Families USA. http://www.familiesusa.org/assets/pdfs/health-reform/Enrollment-Policy-Provisions.pdf. Retrieved April 1, 2012.
- Cohn, Jonathan (July 19, 2013). "We Don't Know Everything About Obamacare. But We Know Who's Trying to Sabotage It". The New Republic. https://newrepublic.com/article/113947/obamacare-implementation-and-role-state-officials.
- Tami Luhby (July 1, 2013). "States forgo billions by opting out of Medicaid expansion". CNN. http://money.cnn.com/2013/07/01/news/economy/medicaid-expansion-states/index.html.
- "Is Medicaid Expansion Good for the States?". U.S. News & World Report. n.d.. https://www.usnews.com/debate-club/is-medicaid-expansion-good-for-the-states.
- Evan Soltas (June 4, 2013). "Wonkbook: The terrible deal for states rejecting Medicaid". The Washington Post. https://www.washingtonpost.com/blogs/wonkblog/wp/2013/06/04/wonkbook-the-terrible-deal-for-states-rejecting-medicaid.
- Rutkin, Aviva. "Obamacare has already improved health of low-income Americans" (in en-US). https://www.newscientist.com/article/2100311-obamacare-has-already-improved-health-of-low-income-americans. Retrieved August 15, 2016.
- "Medicaid expansion under ACA linked with better health care, improved health for low-income adults | News | Harvard T.H. Chan School of Public Health". August 8, 2016. https://www.hsph.harvard.edu/news/press-releases/medicaid-expansion-aca-lbetter-health-care-improved-health-low-income-adults/. Retrieved August 30, 2016.
- Sanger-katz, Margot (August 25, 2016). "How Expanding Medicaid Can Lower Insurance Premiums for All". The New York Times. ISSN 0362-4331. https://www.nytimes.com/2016/08/26/upshot/how-expanding-medicaid-may-lower-insurance-premiums.html. Retrieved September 4, 2016.
- Miller, Sarah; Altekruse, Sean; Johnson, Norman; Wherry, Laura (July 2019). Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data. NBER Working Paper No. 26081. Cambridge, MA: National Bureau of Economic Research. doi:10.3386/w26081. https://dx.doi.org/10.3386%2Fw26081
- Matt Broaddus, Aviva Aron-Dine, "Medicaid Expansion Has Saved at Least 19,000 Lives, New Research Finds. State Decisions Not to Expand Have Led to 15,000 Premature Deaths", Center on Budget and Policy Priorities, November 6, 2019. https://www.cbpp.org/research/health/medicaid-expansion-has-saved-at-least-19000-lives-new-research-finds#_ftn1
- "NationalHealthAccountsProjected". February 15, 2017. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/NationalHealthAccountsProjected.html.
- Mali, Meghashyam (August 11, 2016). "Next president faces possible ObamaCare meltdown". http://thehill.com/policy/healthcare/291056-next-president-faces-possible-obamacare-meltdown. Retrieved August 15, 2016.
- "2017 Premium Changes and Insurer Participation in the Affordable Care Act's Health Insurance Marketplaces". November 2016. http://kff.org/health-reform/issue-brief/2017-premium-changes-and-insurer-participation-in-the-affordable-care-acts-health-insurance-marketplaces/. Retrieved November 23, 2016.
- "Employer Health Benefits 2015". http://files.kff.org/attachment/summary-of-findings-2015-employer-health-benefits-survey. Retrieved November 19, 2016.
- "Average Annual Workplace Family Health Premiums Rise Modest 3%". September 14, 2016. http://kff.org/health-costs/press-release/average-annual-workplace-family-health-premiums-rise-modest-3-to-18142-in-2016-more-workers-enroll-in-high-deductible-plans-with-savings-option-over-past-two-years/. Retrieved November 23, 2016.
- "New Analysis of Health Insurance Premium Trends in the Individual Market Finds Average Yearly Increases of 10 Percent or More Prior to the Affordable Care Act". June 5, 2014. http://www.commonwealthfund.org/publications/press-releases/2014/jun/new-analysis-of-health-insurance-premium-trends.
- Lowrey, Annie (May 7, 2013). "Slowdown in Rise of Healthcare Costs May Persist". The New York Times. https://www.nytimes.com/2013/05/07/business/slowdown-in-rise-of-health-care-costs-may-persist.html. Retrieved June 10, 2013.
- Chait, Jonathan (May 10, 2013). "The Facts Are In and Paul Ryan Is Wrong". New York. http://nymag.com/daily/intelligencer/2013/05/facts-are-in-and-paul-ryan-is-wrong.html.
- Chait, Jonathan (September 26, 2013). "Someone Tell Ted Cruz the Obamacare War Is Over". New York. http://nymag.com/daily/intelligencer/2013/09/someone-tell-ted-cruz-the-obamacare-war-is-over.html.
- Wayne, Alex (June 18, 2013). "Health Cost Growth Slows Further Even as Economy Rebounds". Bloomberg L.P.. https://www.bloomberg.com/news/print/2013-06-18/health-cost-growth-slows-further-even-as-economy-rebounds.html.
- "Assessing the Effects of the Economy on the Recent Slowdown in Health Spending". Kaiser Family Foundation. April 22, 2013. http://kff.org/health-costs/issue-brief/assessing-the-effects-of-the-economy-on-the-recent-slowdown-in-health-spending-2.
- Krawzak, Paul (June 14, 2013). "In Spending Debate, Baby Boomer Issue Remains a Headache for Legislators". Roll Call. http://www.rollcall.com/news/in_spending_debate_baby_boomer_issue_remains_a_headache_for_legislators-225650-1.html.
- Obama B (2016). "United States Health Care Reform – Progress to Date and Next Steps". JAMA 316: 525–32. doi:10.1001/jama.2016.9797. PMID 27400401. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=5069435
- Johnson, Carolyn Y. (September 14, 2016). "How companies are quietly changing your health plan to make you pay more". https://www.washingtonpost.com/news/wonk/wp/2016/09/14/the-quiet-change-to-insurance-plans-thats-making-health-care-more-expensive-for-patients/. Retrieved September 14, 2016.
- "Survey of Non-Group Health Insurance Enrollees, Wave 3". Kaiser Family Foundation. May 20, 2016. http://kff.org/health-reform/poll-finding/survey-of-non-group-health-insurance-enrollees-wave-3/. Retrieved September 14, 2016.
- "Obama's claim the Affordable Care Act was a 'major reason' in preventing 50,000 patient deaths". https://www.washingtonpost.com/news/fact-checker/wp/2015/04/01/obamas-claim-the-affordable-care-act-was-a-major-reason-in-preventing-50000-patient-deaths/. Retrieved November 10, 2016.
- "Repealing the Affordable Care Act will kill more than 43,000 people annually". https://www.washingtonpost.com/posteverything/wp/2017/01/23/repealing-the-affordable-care-act-will-kill-more-than-43000-people-annually/.
- "The Coverage Gap: Uninsured Poor Adults in States that Do Not Expand Medicaid". March 21, 2019. https://www.kff.org/medicaid/issue-brief/the-coverage-gap-uninsured-poor-adults-in-states-that-do-not-expand-medicaid/.
- Bureau of Economic Research, August 2019, "Medicaid and Mortality: New Evidence from Linked Survey and Administrative Data" https://www.nber.org/papers/w26081
- Truthout, July 25, 2019 Republicans' Refusal to Expand Medicaid Resulted in Over 15,000 Deaths https://truthout.org/articles/republicans-refusal-to-expand-medicaid-resulted-in-over-15000-deaths/
- Fonarow, Gregg C.; Yancy, Clyde W.; Matsouaka, Roland A.; Peterson, Eric D.; Hernandez, Adrian F.; Heidenreich, Paul A.; DeVore, Adam D.; Cox, Margueritte et al. (January 1, 2018). "Association of the Hospital Readmissions Reduction Program Implementation With Readmission and Mortality Outcomes in Heart Failure" (in en). JAMA Cardiology 3 (1): 44–53. doi:10.1001/jamacardio.2017.4265. ISSN 2380-6583. PMID 29128869. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=5833526
- Yeh, Robert W.; Shen, Changyu; Haneuse, Sebastien; Wasfy, Jason H.; Maddox, Karen E. Joynt; Wadhera, Rishi K. (December 25, 2018). "Association of the Hospital Readmissions Reduction Program With Mortality Among Medicare Beneficiaries Hospitalized for Heart Failure, Acute Myocardial Infarction, and Pneumonia" (in en). JAMA 320 (24): 2542–2552. doi:10.1001/jama.2018.19232. ISSN 0098-7484. PMID 30575880. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=6583517
- "It Sure Looks Like This Obamacare Program Has Led to More People Dying" (in en-US). December 27, 2018. https://reason.com/2018/12/27/it-sure-looks-like-this-obamacare-progra/.
- Pines, Jesse M.; Thode, Henry C.; Singer, Adam J. (April 5, 2019). "US Emergency Department Visits and Hospital Discharges Among Uninsured Patients Before and After Implementation of the Affordable Care Act" (in en). JAMA Network Open 2 (4): e192662. doi:10.1001/jamanetworkopen.2019.2662. PMID 31002327. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=6481443
- Kliff, Sarah (December 10, 2019). "The I.R.S. Sent a Letter to 3.9 Million People. It Saved Some of Their Lives." (in en-US). The New York Times. ISSN 0362-4331. https://www.nytimes.com/2019/12/10/upshot/irs-letter-health-insurance-fine-study.html.
- Goldin, Jacob; Lurie, Ithai Z; McCubbin, Janet (2019). Health Insurance and Mortality: Experimental Evidence from Taxpayer Outreach. http://www.nber.org/papers/w26533.
- Blanc, Justin M. Le; Heller, Danielle R.; Friedrich, Ann; Lannin, Donald R.; Park, Tristen S. (2020-07-01). "Association of Medicaid Expansion Under the Affordable Care Act With Breast Cancer Stage at Diagnosis" (in en). JAMA Surgery. doi:10.1001/jamasurg.2020.1495. https://jamanetwork.com/journals/jamasurgery/fullarticle/2767686.
- "The Distribution of Household Income, 2014 | Congressional Budget Office". https://www.cbo.gov/publication/53597.
- "Budgetary and Economic Effects of Repealing the Affordable Care Act". Congressional Budget Office. June 18, 2015. https://www.cbo.gov/publication/50252. Retrieved June 19, 2015.
- "CBO's Analysis of the Major Health Care Legislation Enacted in March 2010". Congressional Budget Office. March 30, 2011. http://www.cbo.gov/publication/22077. Retrieved April 6, 2012.
- "Another Comment on CBO's Estimates for the Insurance Coverage Provisions of the Affordable Care Act". Congressional Budget Office. March 16, 2012. http://www.cbo.gov/publication/43104. Retrieved April 6, 2012.
- "H.R. 4872, Reconciliation Act of 2010". Congressional Budget Office. March 18, 2010. http://www.cbo.gov/ftpdocs/113xx/doc11355/hr4872.pdf. Retrieved March 22, 2010.
- Dennis, Steven (March 18, 2010). "CBO: Health Care Overhaul Would Cost $940 Billion". Roll Call. http://www.rollcall.com/news/44347-1.html. Retrieved March 22, 2010.
- Klein, Ezra (March 22, 2010). "What does the health-care bill do in its first year?". The Washington Post. http://voices.washingtonpost.com/ezra-klein/2010/03/what_does_the_health-care_refo.html.
- "Correction Regarding the Longer-Term Effects of the Manager's Amendment to the Patient Protection and Affordable Care Act". Congressional Budget Office. December 19, 2009. http://www.cbo.gov/ftpdocs/108xx/doc10868/12-19-Reid_Letter_Managers_Correction_Noted.pdf. Retrieved March 22, 2010.
- Judith Solomon; Paul N. Van de Water (April 18, 2012). "Letter: Improving the Strength and Solvency of Medicare". The Center on Budget and Policy Priorities. http://www.cbpp.org/cms/?fa=view&id=3746.
- Pecquet, Julian (March 13, 2012). "CBO: Obama's health law to cost less, cover fewer people than first thought". The Hill. http://thehill.com/blogs/healthwatch/health-reform-implementation/215795-cbo-health-law-to-cost-less-cover-fewer-people-than-first-thought. Retrieved June 29, 2012.
- "CBO's Estimates for the Insurance Coverage Provisions of the Affordable Care Act Updated for the Recent Supreme Court Decision". Congressional Budget Office. July 24, 2012. http://www.cbo.gov/publication/43472. Retrieved August 6, 2012.
- Sahadi, Jeanne (March 13, 2012). "Health reform coverage cost falls slightly". CNN. http://money.cnn.com/2012/03/13/news/economy/health-reform-costs. Retrieved June 29, 2012.
- "Where does health care reform stand?". CNN. March 18, 2010. http://www.cnn.com/2010/POLITICS/03/18/health.care.latest/index.html. Retrieved May 12, 2010.
- Farley, Robert (March 18, 2010). "Pelosi: CBO says health reform bill would cut deficits by $1.2 trillion in second decade". PolitiFact.com. http://www.politifact.com/truth-o-meter/statements/2010/mar/18/nancy-pelosi/pelosi-cbo-says-health-reform-bill-would-cut-defic. Retrieved April 7, 2010.
- Haberkorn, Jennifer. "CBO: Obamacare mandate repeal would cut deficit by $338 billion" (in en). http://politi.co/2hdAFBI.
- "Sen. Tom Coburn: Obamacare PR campaign anchored in spin, not reality". The Washington Examiner. July 8, 2006. Archived from the original on July 17, 2012. https://archive.today/20120717095633/http://washingtonexaminer.com/opinion/op-eds/2010/06/sen-tom-coburn-obamacare-pr-campaign-anchored-spin-not-reality/32134. Retrieved April 1, 2012.
- James Capretta. "Obamacare's Cooked Books and the 'Doc Fix'". National Review. http://www.nationalreview.com/critical-condition/55996/obamacare-s-cooked-books-and-doc-fix/james-c-capretta.
- Hogberg, David (November 22, 2010). "GOP Might Target ObamaCare As Part Of A Medicare 'Doc Fix'". Investor's Business Daily. http://www.investors.com/NewsAndAnalysis/Article/554579/201011221909/GOP-Might-Target-ObamaCare-As-Part-Of-A-Medicare-Doc-Fix.aspx. Retrieved April 1, 2012.
- "Responses to Questions About CBO's Preliminary Estimate of the Direct Spending and Revenue Effects of H.R. 4872, the Reconciliation Act of 2010". Congressional Budget Office. March 19, 2010. http://www.cbo.gov/ftpdocs/113xx/doc11376/RyanLtrhr4872.pdf. Retrieved April 1, 2012.
- Chait, Jonathan (March 24, 2010). "The Doc Fix Myth And The Right's Misinformation Feedback Loop". The New Republic. https://newrepublic.com/blog/jonathan-chait/the-doc-fix-myth.
- Van de Water, Peter (January 7, 2011). "Debunking False Claims About Health Reform, Jobs, and the Deficit". Center for Budget and Policy Priorities. http://www.cbpp.org/cms/index.cfm?fa=view&id=3366.
- "Congress Has Good Record of Implementing Medicare Savings". CBPP. December 4, 2009. http://www.cbpp.org/cms/index.cfm?fa=view&id=3021. Retrieved March 28, 2010.
- "Can Congress cut Medicare costs?". The Washington Post. http://voices.washingtonpost.com/ezra-klein/2009/12/can_congress_cut_medicare_cost.html. Retrieved March 28, 2010.
- Ezra Klein (June 26, 2010). "What to do about the doc fix?" The Washington Post Accessed July 27, 2011. http://voices.washingtonpost.com/ezra-klein/2010/06/what_to_do_about_the_doc_fix.html
- Uwe Reinhardt (March 24, 2010). "Wrapping Your Head Around the Health Bill". The New York Times. https://economix.blogs.nytimes.com/2010/03/24/wrapping-your-head-around-the-health-bill. Retrieved October 9, 2010.
- Holtz-Eakin, Douglas (March 21, 2010). "The Real Arithmetic of Health Care Reform". The New York Times. https://www.nytimes.com/2010/03/21/opinion/21holtz-eakin.html.
- Cohn, Jonathan (January 21, 2011). "The GOP's Trick Play". The New Republic. http://www.tnr.com/blog/jonathan-cohn/81941/trick-play.
- Scheiber, Noam (September 17, 2009). "Is the CBO Biased Against Health Care Reform?". The New Republic. http://www.tnr.com/blog/the-stash/the-cbo-biased-against-health-care-reform.
- "Electronic Medical Records Deadline". https://www.medicalrecords.com/emr-buyers-guide/electronic-medical-records-deadline.
- James, Frank (March 19, 2010). "Health Overhaul Another Promise U.S. Can't Afford: Expert". NPR. https://www.npr.org/blogs/thetwo-way/2010/03/health_overhaul_another_promis.html. Retrieved April 7, 2010.
- Government Printing Office. "Title 26 – Internal Revenue Code". http://www.gpo.gov/fdsys/pkg/USCODE-2011-title26/pdf/USCODE-2011-title26-subtitleD-chap43-sec4980H.pdf.
- Chait, Jonathan (July 3, 2013). "Obama Employer Mandate Delay Train Wreck! Or Not". New York. http://nymag.com/daily/intelligencer/2013/07/obama-employer-mandate-delay-train-wreck-or-not.html.
- Sarah Kliff (May 6, 2013). "Will Obamacare lead to millions more part-time workers? Companies are still deciding". The Washington Post. https://www.washingtonpost.com/blogs/wonkblog/wp/2013/05/06/will-obamacare-lead-to-millions-more-part-time-workers-companies-are-still-deciding.
- Ungar, Rick. "The Real Numbers On 'The Obamacare Effect' Are In-Now Let The Crow Eating Begin". Forbes. https://www.forbes.com/sites/rickungar/2014/03/10/the-real-numbers-on-the-obamacare-effect-are-in-now-let-the-crow-eating-begin/. Retrieved November 11, 2014.
- "Employment Situation Summary". Bureau of Labor Statistics. http://www.bls.gov/news.release/empsit.nr0.htm. Retrieved November 11, 2014.
- Conover, Chris. "Who Can Deny It? Obamacare Is Accelerating U.S. Towards A Part-Time Nation". Forbes. https://www.forbes.com/sites/theapothecary/2013/07/31/who-can-deny-it-obamacare-is-accelerating-u-s-towards-a-part-time-nation/. Retrieved November 11, 2014.
- Moriya, A. S.; Selden, T. M.; Simon, K. I. (January 5, 2016). "Little Change Seen In Part-Time Employment As A Result Of The Affordable Care Act". Health Affairs 35 (1): 119–123. doi:10.1377/hlthaff.2015.0949. PMID 26733709. https://dx.doi.org/10.1377%2Fhlthaff.2015.0949
- Bill Sizemore (February 8, 2013). "Va. workers' part-time hours capped due to health law". The Virginian-Pilot. http://hamptonroads.com/2013/02/state-workers-parttime-hours-capped-due-health-law. Annie-Rose Strasser (February 11, 2013). "Virginia Cuts State Employees' Hours To Avoid Providing Obamacare Coverage". http://thinkprogress.org/health/2013/02/11/1568291/virginia-employees-obamacare.
- Ned Resnikoff (January 14, 2013). "Colleges roll back faculty hours in response to Obamacare". MSNBC. http://tv.msnbc.com/2013/01/14/colleges-roll-back-faculty-hours-in-response-to-obamacare. Sy Mukherjee (January 14, 2013). "Four Public Colleges Will Cut Adjunct Faculty Hours To Avoid Providing Health Coverage Under Obamacare". http://thinkprogress.org/health/2013/01/14/1445301/four-public-colleges-obamacare.
- "As Health Law Changes Loom, A Shift To Part-Time Workers". NPR. April 29, 2013. https://www.npr.org/2013/04/29/179864601/as-health-law-changes-loom-a-shift-to-part-time-workers.
- Jared Bernstein (September 4, 2013). "Stop Blaming Obamacare for Part-Time Workers". Teagan Goddard's Wonkwire. Archived from the original on July 15, 2014. https://web.archive.org/web/20140715044934/http://wonkwire.rollcall.com/2013/09/04/stop-blaming-obamacare-part-time-workers/.
- Matthew Yglesias (July 15, 2013). "Obamacare's Not To Blame For Increasing Part-time Work". Slate. http://www.slate.com/blogs/moneybox/2013/07/15/obamacare_part_time_work.html.
- Timothy Jost (July 2, 2013). "Implementing Health Reform: A One-Year Employer Mandate Delay". Health Affairs. http://healthaffairs.org/blog/2013/07/02/implementing-health-reform-a-one-year-employer-mandate-delay.
- Cohn, Jonathan (July 2, 2013). "Some Bad News About Obamacare That Isn't Bogus". The New Republic. https://newrepublic.com/article/113745/obamacare-employer-mandate-delayed-not-what-doctor-ordered.
- "Finance Committee Makes Flawed Employer Requirement in Health Reform Bill Still More Problematic". Center on Budget and Policy Priorities. July 3, 2013. http://www.cbpp.org/cms/index.cfm?fa=view&id=2921.
- Ezra Klein (July 2, 2013). "Will Obamacare lead to millions more part-time workers? Companies are still deciding". The Washington Post. https://www.washingtonpost.com/blogs/wonkblog/wp/2013/07/02/obamacares-employer-mandate-shouldnt-be-delayed-it-should-be-repealed.
- Matthew Yglesias (July 3, 2013). "Delaying Employer Responsibility Fines Is a Good Idea—the Real Problem Comes Later". Slate. http://www.slate.com/blogs/moneybox/2013/07/03/obamacare_delayed_a_good_idea_covering_up_a_big_problem.html.
- Chait, Jonathan (July 3, 2013). "Obamacare Haters Struggling to Understand What 'Nonessential' Means". New York. http://nymag.com/daily/intelligencer/2013/07/obamacare-haters-struggle-to-get-nonessential.html. Chait, Jonathan (July 3, 2013). "Obamacare Still Not Collapsing". New York. http://nymag.com/daily/intelligencer/2013/07/obamacare-still-not-collapsing.html.
- Cohn, Jonathan (July 15, 2013). "Obamacare's Individual Mandate Can't Wait". The New Republic. https://newrepublic.com/article/113851/obamacare-individual-mandate-republicans-push-delay.
- "Union Letter: Obamacare Will 'Destroy The Very Health and Wellbeing' of Workers", The Wall Street Journal, July 12, 2013. https://blogs.wsj.com/corporate-intelligence/2013/07/12/union-letter-obamacare-will-destroy-the-very-health-and-wellbeing-of-workers/
- O'Donnell, Jayne; Ungar, Laura; Hoyer, Meghan (November 12, 2014). "Rural hospitals in critical condition". USA Today. https://www.usatoday.com/longform/news/nation/2014/11/12/rural-hospital-closings-federal-reimbursement-medicaid-aca/18532471/. Retrieved January 28, 2015. Hamada, Omar L. (November 18, 2014). "Obamacare has detrimental effect on rural hospitals". The Tennessean. http://www.tennessean.com/story/opinion/contributors/2014/11/19/obamacare-detrimental-effect-rural-hospitals/19087985/. Retrieved January 28, 2015.
- Howell, Tom Jr. (May 4, 2015). "ER visits up under Obamacare despite promises, doctors' poll finds". The Washington Times. http://www.washingtontimes.com/news/2015/may/4/er-visits-under-obamacare-doctors-say/#ixzz3ZH4xpm5H. Retrieved May 6, 2015.
- "The Affordable Care Act and Employers". https://www.randstadusa.com/workforce360/workforce-insights/the-affordable-care-act-and-employers/91/. Retrieved August 11, 2016.
- "Is the Affordable Care Act a Hidden Jobs Killer?". CEPR. http://www.cepr.net/blogs/cepr-blog/is-the-affordable-care-act-a-hidden-jobs-killer. Retrieved August 26, 2015.
- Cohn, Jonathan (February 11, 2011). "Sorry, The CBO Did Not Say Health Reform Kills 800,000 Jobs". The New Republic. https://newrepublic.com/blog/jonathan-chait/83310/sorry-the-cbo-did-not-say-health-reform-kills-800000-jobs.
- Cohn, Jonathan (June 13, 2012). "Obamacare, Good for the Economy". The New Republic. https://newrepublic.com/blog/plank/104035/obamacare-romney-economy-benefit-job-regulation-noam.
- "CNN Opinion Research Poll". CNN. March 22, 2010. http://i2.cdn.turner.com/cnn/2010/images/03/22/rel5a.pdf.
- Rasmussen, Scott; Schoen, Doug (March 9, 2010). "Why Obama Can't Move the Health-Care Numbers". The Wall Street Journal. https://www.wsj.com/articles/SB10001424052748704784904575111993559174212.
- Zengerle, Patricia (June 24, 2012). "Reuters-Most Americans Oppose Health Law But Like the Provisions". Reuters. https://www.reuters.com/article/2012/06/24/us-usa-campaign-healthcare-idUSBRE85N01M20120624. Retrieved June 28, 2012.
- Ezra Klein (June 26, 2012). "Republicans hate 'Obamacare', but like most of what it does". The Washington Post. https://www.washingtonpost.com/blogs/ezra-klein/wp/2012/06/26/poll-republicans-hate-obamacare-but-like-most-of-what-it-does. Retrieved June 28, 2012.
- Greg Sargent (June 25, 2012). "Republicans Support Obama's Health Reforms – As Long As His Name Isn't On Them". The Washington Post. https://www.washingtonpost.com/blogs/plum-line/post/republicans-support-obamas-health-reforms--as-long-as-his-name-isnt-on-them/2012/06/25/gJQAq7E51V_blog.html. Retrieved June 28, 2012.
- Chait, Jonathan (June 13, 2013). "Obamacare, Public Opinion, and Conservative Self-Delusion". New York Magazine. http://nymag.com/daily/intelligencer/2013/06/obamacare-and-conservative-self-delusion.html.
- Jackson, David. "Poll: Most oppose blocking Obama health care law". USA Today. Retrieved July 8, 2012. http://content.usatoday.com/communities/theoval/post/2012/07/poll-most-oppose-blocking-obama-health-care-law/1#.T_m-ZJGmW_J
- "Obama and Democrats' Health Care Plan". RealClearPolitics. October 13, 2013. Retrieved March 26, 2014. http://www.realclearpolitics.com/epolls/other/obama_and_democrats_health_care_plan-1130.html#polls
- Swanson, Emily (July 30, 2009). "Health Care Plan: Favor/Oppose". Pollster.com. http://www.huffingtonpost.com/2009/07/30/healthplan_n_725503.html
- "As Health Care Law Proceeds, Opposition and Uncertainty Persist". Pew Research Center. September 16, 2013. http://www.people-press.org/files/legacy-pdf/9-16-13%20Health%20Care%20Release.pdf.
- Page, Susan (March 24, 2010). "Poll: Health care plan gains favor". USA Today. https://www.usatoday.com/news/washington/2010-03-23-health-poll-favorable_N.htm. Retrieved March 24, 2010.
- "AP-GfK Poll: Obama's health care fails to gain support". Associated Press. March 28, 2014. http://bigstory.ap.org/article/poll-obama-health-law-fails-gain-support. Retrieved March 30, 2014.
- "RAND Health Reform Opinion Study". RAND Health. May 1, 2014. https://www.rand.org/health/projects/health-reform-opinion.html. Retrieved May 10, 2014.
- "The ObamaCare 8%". April 30, 2014. https://online.wsj.com/news/articles/SB10001424052702303678404579533362696579096. Retrieved May 1, 2014.
- Alan Colmes, "Poll: Voters No Longer Want To Repeal Obamacare", Liberaland, December 1, 2014. http://www.alan.com/2014/12/01/poll-voters-no-longer-want-to-repeal-obamacare/#
- "Poll: Obamacare and the Supreme Court". CBS News. http://www.cbsnews.com/news/poll-obamacare-and-the-supreme-court/. Retrieved June 23, 2015.
- "After the Election, the Public Remains Sharply Divided on Future of the Affordable Care Act". Kaiser Family Foundation. December 3, 2016. http://kff.org/health-reform/press-release/after-the-election-the-public-remains-sharply-divided-on-future-of-the-affordable-care-act/.
- "Obamacare More Popular Than Ever, Now That It May Be Repealed". NYT. February 1, 2017. https://www.nytimes.com/interactive/2017/02/01/us/politics/100000004904286.mobile.html?.
- Dropp, Kyle; Nyhan, Brendan (February 7, 2017). "One-Third Don't Know Obamacare and Affordable Care Act Are the Same". The New York Times. ISSN 0362-4331. https://www.nytimes.com/2017/02/07/upshot/one-third-dont-know-obamacare-and-affordable-care-act-are-the-same.html.
- Lerman, Amy E.; McCabe, Katherine T. (January 24, 2017). "Personal Experience and Public Opinion: A Theory and Test of Conditional Policy Feedback". The Journal of Politics 79 (2): 624–641. doi:10.1086/689286. ISSN 0022-3816. https://dx.doi.org/10.1086%2F689286
- Wallace, Gregory (June 25, 2012). "'Obamacare': The word that defined the health care debate". CNN. http://www.cnn.com/2012/06/25/politics/obamacare-word-debate/. Retrieved September 4, 2012.
- Amanda Cox; Alicia Desantis; Jeremy White (March 25, 2012). "Fighting to Control the Meaning of 'Obamacare'". The New York Times. https://www.nytimes.com/interactive/2012/03/25/us/politics/fighting-to-control-the-meaning-of-obamacare.html. Retrieved June 29, 2012.
- Baker, Peter (August 3, 2012). "Democrats Embrace Once Pejorative 'Obamacare' Tag". The New York Times. https://www.nytimes.com/2012/08/04/health/policy/democrats-embrace-once-pejorative-obamacare-tag.html?_r=1. Retrieved August 6, 2012.
- Madison, Lucy (August 15, 2011). "On bus tour, Obama embraces 'Obamacare', says 'I do care'". CBS News. http://www.cbsnews.com/news/on-bus-tour-obama-embraces-obamacare-says-i-do-care/. Retrieved April 28, 2012.
- "Sarah Palin falsely claims Barack Obama runs a "death panel"". PolitiFact. August 10, 2009. http://www.politifact.com/truth-o-meter/statements/2009/aug/10/sarah-palin/sarah-palin-barack-obama-death-panel.
- "Seniors Beware". August 23, 2012. http://snopes.com/politics/medical/over75.asp.
- Beutler, Brian (August 13, 2013). "A new kind of birther and death panel insanity explodes". Salon. http://www.salon.com/2013/08/13/republicans_still_pander_to_birthers_and_death_panelists/. Retrieved December 3, 2013.
- Ebeler, Jack; Neuman, Tricia; Cubanski, Juliette (April 13, 2011). "The Independent Payment Advisory Board: A New Approach to Controlling Medicare Spending". Kaiser Family Foundation. p. 3. http://kff.org/health-reform/issue-brief/the-independent-payment-advisory-board-a-new/. Retrieved November 27, 2013.
- Cohn, Jonathan (April 20, 2011). "Here We Go Again, With the Death Panels". The New Republic. https://newrepublic.com/blog/jonathan-cohn/87102/ipab-medicare-commission-repeal-ryan-schwartz.
- Cohn, Jonathan (August 13, 2009). "Mandatory Death Counseling – exposed!". The New Republic. https://newrepublic.com/blog/the-treatment/mandatory-death-counseling-exposed.
- Parsons, Christi; Zajac, Andrew (August 14, 2009). "Senate committee scraps healthcare provision that gave rise to 'death panel' claims; Though the claims are widely discredited, the Senate Finance Committee is withdrawing from its bill the inclusion of advance-care planning consultations, calling them too confusing". Los Angeles Times. http://articles.latimes.com/2009/aug/14/nation/na-health-end-of-life14.
- Nyhan, Brendan (2010). "Why the "Death Panel" Myth Wouldn't Die: Misinformation in the Health Care Reform Debate". The Forum 8 (1). doi:10.2202/1540-8884.1354. http://www.dartmouth.edu/~nyhan/health-care-misinformation.pdf.
- Drobnic Holan, Angie (December 19, 2009). "PolitiFact's Lie of the Year: 'Death panels'". PolitiFact. http://politifact.com/truth-o-meter/article/2009/dec/18/politifact-lie-year-death-panels. Retrieved November 19, 2010.
- Henig, Jess; Robertson, Lori (July 29, 2010). "False Euthanasia Claims". FactCheck.org. http://www.factcheck.org/2009/07/false-euthanasia-claims.
- Lori Robertson (December 24, 2009). "Whoppers of 2009—We review the choicest falsehoods from a year that kept us busy". FactCheck.org. http://www.factcheck.org/2009/12/whoppers-of-2009. Retrieved April 28, 2011.
- "'Tweet' 2009 Word of the Year, 'Google' Word of the Decade, as voted by American Dialect Society". American Dialect Society. January 8, 2010. http://www.americandialect.org/2009-Word-of-the-Year-PRESS-RELEASE.pdf. Retrieved October 8, 2010.
- "Euthanasia Counseling". August 13, 2009. http://snopes.com/politics/medical/euthanasia.asp.
- Public Law 111 – 148, section 1312: "... the only health plans that the Federal Government may make available to Members of Congress and congressional staff with respect to their service as a Member of Congress or congressional staff shall be health plans that are (I) created under this Act (or an amendment made by this Act); or (II) offered through an Exchange established under this Act (or an amendment made by this Act)." https://www.gpo.gov/fdsys/pkg/PLAW-111publ148/html/PLAW-111publ148.htm
- Robertson, Lori (January 20, 2010). "Congress Exempt from Health Bill?". FactCheck.org. http://www.factcheck.org/2010/01/congress-exempt-from-health-bill.
- Farley, Robert (January 21, 2010). "The Democrats' health care bills would provide 'free health care for illegal immigrants'". PolitiFact. http://www.politifact.com/truth-o-meter/statements/2010/jan/21/chain-email/chain-e-mail-claims-health-care-bills-congress-wou. Retrieved August 19, 2013.
- "The Once and Future Obamacare Death Spiral". Bloomberg. January 18, 2017. https://www.bloomberg.com/view/articles/2017-01-18/the-once-and-future-obamacare-death-spiral.
- "Number of Insurers Participating in the Individual Health Insurance Marketplaces". Kaiser Family Foundation. January 30, 2017. http://kff.org/other/state-indicator/number-of-issuers-participating-in-the-individual-health-insurance-marketplace/?currentTimeframe=0.
- "A Town Hall, and a Health Care Model, in Green Bay". The White House Blog. http://www.whitehouse.gov/blog/A-Town-Hall-and-a-Health-Care-Model-in-Green-Bay. Retrieved November 9, 2013.
- Jacobson, Louis. "Barack Obama says that what he'd said was you could keep your plan 'if it hasn't changed since the law passed'". PolitiFact. http://www.politifact.com/truth-o-meter/statements/2013/nov/06/barack-obama/barack-obama-says-what-hed-said-was-you-could-keep/. Retrieved November 9, 2013.
- "After the big Obamacare apology: where things stand". CNN. November 8, 2013. http://www.cnn.com/2013/11/08/politics/obama-obamacare-apology. Retrieved November 9, 2013.
- "Obama apologizes for insurance cancellations due to Obamacare". CNN. http://www.cnn.com/2013/11/07/politics/obama-obamacare-apology. Retrieved July 29, 2014.
- Sealover, Ed (November 8, 2013). "Health insurers say they're canceling plans because of federal law". Denver Business Journal. http://www.bizjournals.com/denver/news/2013/11/08/health-insurers-canceling-plans-say.html. Retrieved November 9, 2013.
- "Lie of the Year: "If you like your health care plan, you can keep it". Politifact. December 12, 2014. http://www.politifact.com/truth-o-meter/article/2013/dec/12/lie-year-if-you-like-your-health-care-plan-keep-it/. Retrieved April 5, 2018.
- Weigel, David (November 8, 2013). "The White House's Website Still Says If You Like Your Plan You Can Keep It". Slate. http://www.slate.com/blogs/weigel/2013/11/08/the_white_house_s_web_site_still_says_if_you_like_your_plan_you_can_keep.html. Retrieved November 9, 2013.
- "Obamacare: The debacle". The Economist. November 2, 2013. https://www.economist.com/news/united-states/21588951-congress-hears-tales-baffling-ineptitude-debacle. Retrieved November 8, 2013.
- Schoof, Renee (November 8, 2013). "Congress weighing laws to let people keep health insurance". McClatchyDC. http://www.mcclatchydc.com/2013/11/08/207999/congress-weighing-laws-to-let.html. Retrieved November 14, 2013.
- Drobnic Holan, Angie (December 12, 2013). "Lie of the Year: 'If you like your health care plan, you can keep it'" (in en). https://www.politifact.com/truth-o-meter/article/2013/dec/12/lie-year-if-you-like-your-health-care-plan-keep-it/.
- "Labor leaders' letter to Harry Reid and Nancy Pelosi". The Washington Post. January 27, 2014. https://apps.washingtonpost.com/g/page/politics/labor-leaders-letter-to-harry-reid-and-nancy-pelosi/785/. Retrieved February 13, 2014.
- "Union Letter: Obamacare Will 'Destroy The Very Health and Wellbeing' of Workers". The Wall Street Journal. July 12, 2013. https://blogs.wsj.com/corporate-intelligence/2013/07/12/union-letter-obamacare-will-destroy-the-very-health-and-wellbeing-of-workers/. Retrieved October 7, 2013.
- Stolberg, Sheryl Gay (October 18, 2013). "States Are Focus of Effort to Foil Health Care Law". The New York Times. https://www.nytimes.com/2013/10/19/us/politics/states-are-focus-of-effort-to-foil-health-care-law.html. Retrieved October 19, 2013.
- The Editorial Board (January 25, 2014). "The Koch Party". The New York Times. https://www.nytimes.com/2014/01/26/opinion/sunday/the-koch-party.html. Retrieved January 25, 2014.
- Peters, Jeremy (January 20, 2011). "Conservatives' Aggressive Ad Campaign Seeks to Cast Doubt on Health Law". The New York Times. https://www.nytimes.com/2013/07/07/us/politics/conservatives-aggressive-ad-campaign-seeks-to-cast-doubt-on-health-law.html.
- Chait, Jonathan (July 23, 2013). "Conservatives Brace for the Possibility Obamacare Won't Totally Suck". The New Republic. https://newrepublic.com/article/113994/obamacare-implementation-conservatives-brace-it-working.
- Michael Cannon (July 6, 2007). "The Anti-Universal Coverage Club Manifesto". Cato Institute. http://www.cato.org/blog/anti-universal-coverage-club-manifesto.
- Chait, Jonathan (June 25, 2012). "Health Care As a Privilege: What the GOP Won't Admit". New York. http://nymag.com/daily/intelligencer/2012/06/health-care-as-privilege-what-gop-wont-admit.html.
- Schoen, John W. (November 9, 2016). "Here's what's coming from the Trump administration". https://www.cnbc.com/2016/11/09/trumps-first-100-day-agenda-may-be-stymied-by-his-own-party.html. Retrieved November 16, 2016.
- Haberman, Maggie; Pear, Robert (January 10, 2017). "Trump Tells Congress to Repeal and Replace Health Care Law 'Very Quickly'". The New York Times. https://www.nytimes.com/2017/01/10/us/repeal-affordable-care-act-donald-trump.html. Retrieved January 25, 2017.
- "Resolution 54: AFL-CIO Convention Resolution on the Affordable Care Act". AFL-CIO. September 11, 2013. http://www.aflcio.org/About/Exec-Council/Conventions/2013/Resolutions-and-Amendments/Resolution-54-AFL-CIO-Convention-Resolution-on-the-Affordable-Care-Act. Retrieved October 7, 2013.
- Pradhan, Rachana (October 12, 2016). "Democratic governor: Obamacare 'no longer affordable' for many". Politico. http://www.politico.com/story/2016/10/minnesota-mark-dayton-obamacare-not-affordable-229690.
- Demko, Paul (October 21, 2016). "Democratic governor expresses regret over Obamacare comments, requests emergency relief for rate hikes". Politico. http://www.politico.com/story/2016/10/mark-dayton-obamacare-comments-affordable-230156.
- Cauchi, Richard (November 15, 2013). "State Legislation and Actions Challenging Certain Health Reforms". National Conference of State Legislatures. http://www.ncsl.org/research/health/state-laws-and-actions-challenging-ppaca.aspx. Retrieved November 28, 2013.
- "Health Care Lawsuit Case Challenges". Independent Women's Forum. November 26, 2013. http://www.healthcarelawsuits.org/cases.php. Retrieved November 28, 2013.
- "Analysis: U.S. Supreme Court Upholds the Affordable Care Act: Roberts Rules?". The National Law Review. von Briesen & Roper, S.C.. June 29, 2012. http://www.natlawreview.com/article/analysis-us-supreme-court-upholds-affordable-care-act-roberts-rules. Retrieved July 2, 2012.
- "March 14, 2012 Statement on Religious Freedom and HHS Mandate". United States Conference of Catholic Bishops. March 14, 2012. http://www.usccb.org/issues-and-action/religious-liberty/march-14-statement-on-religious-freedom-and-hhs-mandate.cfm. Retrieved April 28, 2012.
- Goodstein, Laurie (May 21, 2012). "Catholics File Suits on Contraceptive Coverage". The New York Times. https://www.nytimes.com/2012/05/22/us/catholic-groups-file-suits-on-contraceptive-coverage.html?_r=0.
- News, A. B. C.. "Supreme Court allows Trump to exempt employers from Obamacare birth control mandate" (in en). https://abcnews.go.com/Politics/supreme-court-trump-exempt-employers-obamacare-birth-control/story?id=71254754&cid=clicksource_4380645_2_heads_hero_live_headlines_hed. Retrieved July 8, 2020.
- Taylor, Audrey; Seanz, Arlette; Levine, Mike (June 25, 2015). "Supreme Court Upholds Obamacare Subsidies, President Says ACA 'Is Here to Stay'". ABC News. https://abcnews.go.com/Politics/supreme-court-upholds-obama-health-care-subsidies/story?id=31931412. Retrieved June 25, 2015.
- "Eliminating Cost-Sharing Reductions in ACA" (in en). https://www.commonwealthfund.org/publications/explainer/2017/apr/essential-facts-about-health-reform-alternatives-eliminating-cost.
- (in en) More Insurers Win Lawsuits Seeking Cost-Sharing Reduction Payments | Health Affairs. doi:10.1377/hblog20190217.755658. https://www.healthaffairs.org/do/10.1377/hblog20190217.755658/full/. Retrieved December 1, 2019.
- Haberkorn, Jennifer (May 12, 2016). "House GOP wins Obamacare lawsuit". Politico. http://www.politico.com/story/2016/05/house-gop-wins-obamacare-lawsuit-223121. Retrieved August 21, 2016.
- Sargent, Greg (May 26, 2017), "Trump's latest tantrum will hurt hundreds of thousands of people. Here's how.", The Washington Post, https://www.washingtonpost.com/blogs/plum-line/wp/2017/05/26/trumps-latest-tantrum-will-hurt-hundreds-of-thousands-of-people-heres-how/?tid=hybrid_collaborative_1_na, retrieved May 29, 2017
- Denniston, Lyle (2016-05-12). "Judge: Billions spent illegally on ACA benefits". http://www.scotusblog.com/2016/05/judge-billions-spent-illegally-on-aca-benefits/.
- [1]
- de Vogue, Ariane; Luhby, Tami (December 14, 2018). "Federal judge in Texas strikes down Affordable Care Act". CNN. https://www.cnn.com/2018/12/14/politics/texas-aca-lawsuit/index.html. Retrieved December 14, 2018.
- Sullivan, Peter (December 14, 2018). "Federal judge in Texas strikes down ObamaCare" (in en). https://thehill.com/policy/healthcare/421511-federal-judge-in-texas-strikes-down-obamacare.
- Armour, Stephanie (December 14, 2018). "Federal Judge Rules Affordable Care Act Is Unconstitutional Without Insurance-Coverage Penalty". https://www.wsj.com/articles/federal-judge-rules-affordable-care-act-is-unconstitutional-11544838743.
- "Federal Judge in Texas Strikes Down "Obamacare"". https://lawshelf.com/blog/post/federal-judge-in-texas-strikes-down-obamacare.
- Biskupic, Joan (July 8, 2019). "Affordable Care Act gears up for momentous test in court". CNN. https://www.cnn.com/2019/07/08/politics/affordable-care-act-court/index.html. Retrieved July 8, 2019.
- Goldstein, Amy (December 14, 2018). "Federal judge in Texas rules entire Obama health-care law is unconstitutional". The Washington Post. https://www.washingtonpost.com/national/health-science/federal-judge-in-texas-rules-obama-health-care-law-unconstitutional/2018/12/14/9e8bb5a2-fd63-11e8-862a-b6a6f3ce8199_story.html. Retrieved December 14, 2018.
- Sullivan, Kate; Luhby, Tami (December 30, 2018). "Judge says Affordable Care Act will remain in effect during appeal". CNN. https://www.cnn.com/2018/12/30/politics/judge-affordable-care-act-remain-in-effect-appeal/index.html. Retrieved December 31, 2018.
- Goodnough, Abby (July 9, 2019). "Obamacare in Jeopardy as Appeals Court Hears Case Backed by Trump". The New York Times. https://www.nytimes.com/2019/07/09/health/obamacare-appeals-court.html. Retrieved July 9, 2019.
- Goodnough, Abby (July 9, 2019). "Appeals Court Seems Skeptical About Constitutionality of Obamacare Mandate". The New York Times. https://www.nytimes.com/2019/07/09/health/obamacare-appeals-court.html. Retrieved July 9, 2019.
- Demko, Paul (December 18, 2019). "Court voids Obamacare mandate—but not the whole law". Politico. https://www.politico.com/news/2019/12/18/court-finds-obamacare-mandate-unconstitutional-sends-case-back-to-lower-court-087389.
- Liptak, Adam (March 2, 2020). "Supreme Court to Hear Obamacare Appeal". The New York Times. https://www.nytimes.com/2020/03/02/us/supreme-court-obamacare-appeal.html. Retrieved March 2, 2020.
- Ollstein, Alice Miranda; Arkin, James (December 26, 2019), "Democrats seize on anti-Obamacare ruling to steamroll GOP in 2020", Politico, https://www.politico.com/news/2019/12/26/democrats-anti-o0bamacare-2020-elections-089765, retrieved February 6, 2020
- Somashekhar, Sandhya (August 29, 2013). "States find new ways to resist health law". The Washington Post. https://www.washingtonpost.com/national/health-science/states-find-new-ways-to-resist-health-law/2013/08/28/c63f8498-0a93-11e3-8974-f97ab3b3c677_story.html.
- Ornstein, Norm (July 24, 2013). "The Unprecedented and Contemptible Attempts to Sabotage Obamacare". National Journal. http://www.nationaljournal.com/columns/washington-inside-out/the-unprecedented-and-contemptible-attempts-to-sabotage-obamacare-20130724.
- Pear, Robert (August 2, 2013). "Missouri Citizens Face Obstacles to Coverage". The New York Times. https://www.nytimes.com/2013/08/03/us/missouri-citizens-face-obstacles-to-coverage.html. Retrieved August 3, 2013.
- Cohn, Jonathan (July 25, 2013). "The Right's Latest Scheme to Sabotage Obamacare". The New Republic. https://newrepublic.com/article/114028/obamacare-sabotage-watch-conservative-campaign-gets-real.
- Kliff, Sarah (August 1, 2013). "Inside the Obamacare Resistance". The Washington Post. https://www.washingtonpost.com/blogs/wonkblog/wp/2013/08/01/inside-the-obamacare-resistance.
- O'Brien, Michael (March 22, 2010). "GOP quick to release 'repeal' bills". The Hill. http://thehill.com/blogs/blog-briefing-room/news/88323-house-and-senate-republicans-quick-to-release-repeal-bills. Retrieved April 1, 2012.
- "Bill Summary & Status – 112th Congress (2011–2012) – H.R. 2". THOMAS. January 19, 2011. http://thomas.loc.gov/cgi-bin/bdquery/z?d112:HR00002:.
- "Final Vote Results for passage of Repealing the Job-Killing Health Care Law Act (H.R. 2)". THOMAS. January 19, 2011. http://clerk.house.gov/evs/2011/roll014.xml.
- "Motion to Waive All Applicable Budgetary Discipline Re: McConnell Amdt. No. 13". U.S. Senate. February 2, 2011. https://www.senate.gov/legislative/LIS/roll_call_lists/roll_call_vote_cfm.cfm?congress=112&session=1&vote=00009. Retrieved April 1, 2012.
- "House Passes Health Care Repeal 245–189". C-SPAN. January 19, 2011. http://c-span.com/Events/House-Passes-Health-Care-Repeal-245-189/10737418994.
- Deirdre Walsh (February 3, 2015). "House votes -again-to repeal Obamacare". Reuters. http://www.cnn.com/2015/02/03/politics/obamacare-repeal-vote-house/index.html. Retrieved February 4, 2015.
- Jonathan Weisman; Robert Pear (May 26, 2013). "Partisan Gridlock Thwarts Effort to Alter Health Law". The New York Times. https://www.nytimes.com/2013/05/27/us/politics/polarized-congress-thwarts-changes-to-health-care-law.html. Retrieved May 27, 2013. "we cannot use any of the normal tools to resolve ambiguities or fix problems"
- Lipton, Eric (March 19, 2013). "In Shift, Lobbyists Look for Bipartisan Support to Repeal a Tax". The New York Times. https://www.nytimes.com/2013/03/20/us/politics/lobbyists-look-for-bipartisan-support-to-repeal-a-tax.html?pagewanted=all&_r=0.
- Chait, Jonathan (July 3, 2013). "Obamacare Still Not Collapsing". New York. http://nymag.com/daily/intelligencer/2013/07/obamacare-still-not-collapsing.html.
- Cohn, Jonathan (December 23, 2010). "What Defunding Health Reform Would Do". The New Republic. https://newrepublic.com/blog/jonathan-cohn/80411/what-defunding-health-reform-would-do.
- Lori Montgomery; Paul Kane (October 1, 2013). "Shutdown begins: Stalemate forces first U.S. government closure in 17 years". The Washington Post. https://www.washingtonpost.com/politics/washington-braces-for-the-first-shutdown-of-the-national-government-in-17-years/2013/09/30/977ebca2-29bd-11e3-97a3-ff2758228523_story.html. Blake, Aaron (September 19, 2013). "McCain: Efforts to repeal and defund Obamacare 'not rational'". The Washington Post. https://www.washingtonpost.com/blogs/post-politics/wp/2013/09/19/mccain-efforts-to-repeal-and-defund-obamacare-not-rational. Retrieved September 24, 2013.
- Beutler, Brian (September 19, 2013). "New test could expose GOP's pack of charlatans". Salon. http://www.salon.com/2013/09/19/john_boehner_just_made_ted_cruz_life_a_living_hell. Retrieved September 24, 2013.
- Cohn, Jonathan (August 7, 2013). "Tea Party to Republicans: Shut Down the Government, or You're a Sellout". The New Republic. https://newrepublic.com/article/114229/tea-party-wants-government-shutdown-over-obamacare.
- Kaplan, Thomas; Pear, Robert (January 12, 2017). "Senate Takes Major Step Toward Repealing Health Care Law". The New York Times. https://www.nytimes.com/2017/01/12/us/politics/health-care-congress-vote-a-rama.html?_r=0.
- "GOP Senate to Move Forward on ObamaCare Repeal". Fox News Politics. January 11, 2017. http://www.foxnews.com/politics/2017/01/11/gop-senate-to-move-forward-on-obamacare-repeal.html.
- Lee, MJ; Barrett, Ted; LoBianco, Tom (January 12, 2017). "Senate Opens Obamacare Repeal Drive with Overnight Marathon". CNN. http://www.cnn.com/2017/01/11/politics/senate-obamacare-repeal/.
- Caldwell, Leigh Ann (January 12, 2017). "Senate Approves First Step Toward Repealing Obamacare in Late-Night Session". NBC News. http://www.nbcnews.com/politics/congress/senate-vote-obamacare-repeal-measure-late-night-session-n705816.
- Golstein, Amy; DeBonis, Mike; Snell, Kelsey. "House Republicans release long-awaited plan to repeal and replace Obamacare". Washington Post. https://www.washingtonpost.com/powerpost/new-details-emerge-on-gop-plans-to-repeal-and-replace-obamacare/2017/03/06/04751e3e-028f-11e7-ad5b-d22680e18d10_story.html. Retrieved March 7, 2017.
- Pear, Robert (March 24, 2017). "Push to Repeal Health Law Fails". New York Times. https://www.nytimes.com/2017/03/24/us/politics/health-care-affordable-care-act.html. Retrieved March 24, 2017.
- "House Republicans pass bill to repeal and replace Obamacare". CNN. May 4, 2017. http://edition.cnn.com/2017/05/04/politics/health-care-vote/. Retrieved May 4, 2017.
- Bryan, Bob (May 4, 2017). "Senate Republicans signal they plan to scrap bill the House just passed and write their own". https://www.businessinsider.com/senate-plan-for-healthcare-bill-ahca-2017-5.
- Kaplan, Thomas; Pear, Robert (June 15, 2017). "Secrecy Surrounding Senate Health Bill Raises Alarms in Both Parties". New York Times. Archived from the original on June 18, 2017. https://web.archive.org/web/20170618182849/https://www.nytimes.com/2017/06/15/us/politics/secrecy-surrounding-senate-health-bill-raises-alarms-in-both-parties.html.
- Bump, Philip (June 13, 2017). "The remarkable steps Republicans are taking to obscure what's in their health-care bill". Washington Post. Archived from the original on June 20, 2017. https://web.archive.org/web/20170620082523/https://www.washingtonpost.com/news/politics/wp/2017/06/13/the-remarkable-steps-republicans-are-taking-to-obscure-whats-in-their-health-care-bill/.
- Sarlin, Benjy; Caldwell, Leigh Ann (June 15, 2017). "The Senate's Health Care Bill Remains Shrouded in Secrecy". NBC News. Archived from the original on June 19, 2017. https://web.archive.org/web/20170619162148/http://www.nbcnews.com/politics/congress/senate-s-health-care-bill-remains-shrouded-secrecy-n772456.
- "H.R. 1628, Better Care Reconciliation Act of 2017, discussion draft ERN17282". Senate Budget Committee. June 22, 2017. https://www.budget.senate.gov/imo/media/doc/SENATEHEALTHCARE.pdf.
- "McCain returns as Senate advances health bill". Archived from the original on July 25, 2017. https://web.archive.org/web/20170725204952/http://www.cnn.com/2017/07/25/politics/senate-health-care-vote/index.html.
- Klein, Ezra (July 28, 2017), The GOP's massive health care failures, explained, Vox, https://www.vox.com/health-care/2017/7/28/16055284/gop-massive-health-care-failures-explained, retrieved August 3, 2017
- Rattner, Steven (December 29, 2017). "Opinion | 2017: The Year in Charts". https://www.nytimes.com/interactive/2017/12/29/opinion/2017-the-year-in-charts.html,%20https://www.nytimes.com/interactive/2017/12/29/opinion/2017-the-year-in-charts.html.
- "American Healthcare Act Cost Estimate". Congressional Budget Office. March 13, 2017. https://www.cbo.gov/sites/default/files/115th-congress-2017-2018/costestimate/americanhealthcareact_0.pdf.
- Edsall, Thomas B. (July 27, 2017). "Opinion | Killing Obamacare Softly". https://www.nytimes.com/2017/07/27/opinion/health-care-obamacare.html.
- Kliff, Sarah (September 14, 2017). "CBO: Trump is making Obamacare premiums more expensive". https://www.vox.com/policy-and-politics/2017/9/14/16308502/cbo-trump-obamacare-premiums.
- Scott, Dylan (October 18, 2017). "Obamacare premiums were stabilizing. Then Trump happened". Vox. https://www.vox.com/policy-and-politics/2017/10/18/16458316/obamacare-premiums-trump
- Kliff, Sarah (October 18, 2017). "Sarah Kliff-Trump's stance on insurance 'bailouts' is completely incoherent" Vox. https://www.vox.com/health-care/2017/10/18/16499806/trump-insurance-bailouts-completely-incoherent
- "The Effects of Terminating Payments for Cost-Sharing Reductions". Center on Budget and Policy Priorities. August 15, 2017. https://www.cbo.gov/publication/53009
- Keith, Katie (September 6, 2018). "Insurer Wins First CSR Payment Decision; Updates On BHP And Risk Corridors Litigation". Health Affairs. Archived from the original on August 17, 2019. https://web.archive.org/web/20190817032812/https://www.healthaffairs.org/do/10.1377/hblog20180906.295628/full/. Retrieved March 31, 2020.
- Keith, Katie (February 17, 2019). "More Insurers Win Lawsuits Seeking Cost-Sharing Reduction Payments". Health Affairs. Archived from the original on February 8, 2020. https://web.archive.org/web/20200208052713/https://www.healthaffairs.org/do/10.1377/hblog20190217.755658/full/. Retrieved March 31, 2020.
- Pear, Robert (December 9, 2015). "Marco Rubio Quietly Undermines Affordable Care Act". https://www.nytimes.com/2015/12/10/us/politics/marco-rubio-obamacare-affordable-care-act.html.
- Timothy S. Jost. "Supreme Court to Hear Case on Affordable Care Act's Risk Corridors" (in en). Commonwealth Fund. https://www.commonwealthfund.org/blog/2019/supreme-court-hear-case-affordable-care-acts-risk-corridors.
- Galewitz, Phil (December 9, 2010). "ACA Insurers In The Supreme Court: Why Consumers Should Pay Attention". National Public Radio. Archived from the original on March 31, 2020. https://web.archive.org/web/20200331224050/https://www.npr.org/sections/health-shots/2019/12/09/786315240/aca-insurers-in-the-supreme-court-why-consumers-should-pay-attention?t=1585694181108. Retrieved March 31, 2020.
- Ian Millhiser (December 10, 2019). "Obamacare had an unusually good day at the Supreme Court". Vox. Archived from the original on December 30, 2019. https://web.archive.org/web/20191230061526/https://www.vox.com/2019/12/10/21004821/obamacare-supreme-court-risk-corridors-maine-community. Retrieved March 31, 2020.
- Ehley, Brianna; Lorenzo, Aaron. "Trump still enforcing Obamacare mandate". https://www.politico.com/story/2017/05/03/trump-obamacare-mandate-enforcement-237937.
- Kliff, Sarah (August 31, 2017). "Trump is slashing Obamacare's advertising budget by 90%". https://www.vox.com/2017/8/31/16236280/trump-obamacare-outreach-ads.
- Board, The Editorial (November 4, 2017). "Opinion | Obamacare vs. the Saboteurs". https://www.nytimes.com/2017/11/04/opinion/obamacare-vs-the-saboteurs.html.
- "10 ways the GOP sabotaged Obamacare". May 17, 2017. https://www.healthinsurance.org/blog/2017/05/17/10-ways-the-gop-sabotaged-obamacare/.
- "History of the Affordable Care Act (ACA)". October 22, 2014. https://resources.ehealthinsurance.com/affordable-care-act/history-timeline-affordable-care-act-aca.
- Enzi, Michael B. (August 2, 2011). "Health Care Reforrm Law's Impact on Child-Only Health Insurance Policies". http://www.help.senate.gov/imo/media/doc/Child-Only%20Health%20Insurance%20Report%20Aug%202,%202011.pdf. Retrieved August 10, 2016.
- Liptak, Adam (September 30, 2012). "Supreme Court justices face important rulings in upcoming term September". The New York Times. Pittsburgh Post-Gazette. http://www.post-gazette.com/stories/news/us/supreme-court-justices-face-important-rulings-in-upcoming-term-655566/. Retrieved September 30, 2012.
- "Status of State Action on the Medicaid Expansion Decision" (in en-US). Kaiser Family Foundation. http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/. Retrieved August 12, 2016.
- Walton, Alice G.. "How To Explain The Obamacare Ruling To A Five-Year-Old". https://www.forbes.com/sites/alicegwalton/2012/07/02/how-to-explain-the-obamacare-ruling-to-a-five-year-old/#23e103e723e1. Retrieved May 5, 2017.
- "A Cruel Blow to American Families". The New York Times. February 2, 2013. https://www.nytimes.com/2013/02/03/opinion/sunday/a-cruel-blow-to-american-families.html.
- Cohn, Jonathan (February 5, 2013). "Not-So-Universal Health Care". The New Republic. https://newrepublic.com/article/112327/obamacare-not-universal-you-thought.
- Mazur, Mark. "Continuing to Implement the ACA in a Careful, Thoughtful Manner". United States Department of the Treasury. http://www.treasury.gov/connect/blog/Pages/Continuing-to-Implement-the-ACA-in-a-Careful-Thoughtful-Manner-.aspx. Retrieved July 16, 2013.
- Madara, Matthew R. (February 11, 2014). "ACA Employer Shared Responsibility Delay Included in Final Regs". Tax Notes Today 2014 TNT 28–1.
- Kennedy, Kelly (December 1, 2013). "White House claims success on HealthCare.gov repairs". USA Today. https://www.usatoday.com/story/news/politics/2013/12/01/federalexchangmeetsgoal/3795523/. Retrieved December 1, 2013.
- Cohen, Tom (October 23, 2013). "Rough Obamacare rollout: 4 reasons why". CNN. http://www.cnn.com/2013/10/22/politics/obamacare-website-four-reasons. Retrieved November 5, 2013.
- Holland, Steve; Rampton, Roberta (November 6, 2013). "Senate Democrats frustrated with botched rollout of Obamacare". The Christian Science Monitor. Reuters. http://www.csmonitor.com/USA/Latest-News-Wires/2013/1106/Senate-Democrats-frustrated-with-botched-rollout-of-Obamacare. Retrieved November 19, 2013.
- Alonso-Zaldivar, Ricardo (July 31, 2014). "Probe exposes flaws behind HealthCare.gov rollout". AP News. http://apnews.excite.com/article/20140731/us-health-overhaul-de4c72c273.html. Retrieved July 31, 2014.
- Burwell v. Hobby Lobby, 573 U.S. (United States Supreme Court 2014). https://www.supremecourt.gov/opinions/13pdf/13-354_olp1.pdf
- Tracer, Zachary. "Obamacare Sign-Ups Decline to 10.2 Million as Some Don't Pay". https://www.bloomberg.com/news/articles/2015-06-02/obamacare-dropouts-lead-to-enrollment-decline-of-1-5-million. Retrieved August 21, 2016.
- "December 31, 2015 Effectuated Enrollment Snapshot". March 11, 2016. https://www.cms.gov/Newsroom/MediaReleaseDatabase/Fact-sheets/2016-Fact-sheets-items/2016-03-11.html.
- COOK, NANCY (December 16, 2015). "How the White House lost on the Cadillac Tax". Politico. http://www.politico.com/story/2015/12/white-house-obamacare-cadillac-tax-216881. Retrieved August 21, 2016.
- Mathews, Anna Wilde (August 16, 2016). "Aetna to Drop Some Affordable Care Act Markets". Wall Street Journal. ISSN 0099-9660. https://www.wsj.com/articles/aetna-to-drop-some-affordable-care-act-markets-1471311737. Retrieved August 16, 2016.
- Ip, Greg (August 17, 2016). "The Unstable Economics in Obama's Health Law". Wall Street Journal. ISSN 0099-9660. https://www.wsj.com/articles/the-unstable-economics-in-obamas-health-law-1471452938. Retrieved August 23, 2016.
- "Affordable Care Act signups dip amid uncertainty and Trump attacks". February 3, 2017. https://www.nytimes.com/2017/02/03/us/politics/affordable-care-act-obama-care-sign-up.html?.
- Morton, Victor (February 14, 2017). "IRS weakens enforcement of Obamacare individual mandate: Report" (in en-US). The Washington Times. http://www.washingtontimes.com/news/2017/feb/14/irs-weakens-enforcement-obamacare-individual-manda/.
- "House Passes Bill to Repeal Obamacare: Live Updates". WSJ. https://www.wsj.com/livecoverage/house-gop-obamacare-repeal-bill-vote. Retrieved May 5, 2017.
- Epstein, Reid J. (May 5, 2017). "Analyst Sees Danger for House Republicans After Health Bill Vote". WSJ. https://blogs.wsj.com/washwire/2017/05/05/analyst-sees-danger-for-house-republicans-after-health-bill-vote/. Retrieved May 5, 2017.
- O'Brien, Elizabeth (December 2, 2017). "The Senate's Tax Bill Eliminates the Individual Mandate for Health Insurance. Here's What You Need to Know". Money. http://time.com/money/5043622/gop-tax-reform-bill-individual-mandate/.
- Thomas Kaplan and Robert Pear. "2 Senators Strike Deal on Health Subsidies That Trump Cut Off". https://www.nytimes.com/2017/10/17/us/politics/alexander-murray-deal-obamacare-subsidies.html?_r=0.
- "Where the states stand on Medicaid expansion". February 6, 2019. https://www.advisory.com/daily-briefing/resources/primers/medicaidmap.
