Malaria is an infectious disease caused by a parasite; it is spread by the bite of an infected mosquito. Every year, 300 to 700 million people get infected. Malaria kills 1 million to 2 million people every year. 90% of the deaths occur in Africa.
- malaria
- infectious disease
- mosquito
1. Chronology
| Period | Event |
|---|---|
| Prehistory (from Jurassic period to Paleolithic) | The origin of malaria dates back to a very early time in a warm and humid Africa, being present long before the whole timeline of development of apes.[1] Malaria infection in humans from parasite plasmodium falciparum is thought to have been originally caught from gorillas.[2] |
| Ancient history | Malaria is already known throughout the era of the Roman Empire,[3] Ancient Egypt and the Indian subcontinent.[4] In Ancient Greece , Hippocrates already writes a description of the disease.[5] Malaria is also known to exist in Ancient China.[6] Antimalarial artemisinin is described.[7] |
| Middle Ages | In Europe, witchcraft and astrology thrive around the treatment during this period.[8] Malaria is attributed to a 'bad air', hence the term mal aria (from Medieval Italian).[9] |
| 1500s–1600s | Malaria reaches the Americas through Spanish colonization. The native population in Peru makes use of bark of the cinchona tree for treating fever.[10] After its discovery by the Spanish, the bark is brought to Europe where it comes into general use.[10][11][12][13] |
| 1700s | The cinchona bark from South America is established as a major cure for fever in the Western World.[14] |
| 1800s | Parasites are first identified as source of malaria.[15] |
| 1900s | Increasing scientific research leads to rapid advance in the knowledge of malarial parasites and the development of drugs, such as chloroquine, mefloquine and pyrimethamine. Antibiotics are also developed. DDT insecticidal properties are discovered.[16] Early eradications are achieved in the first half of the century.[17] |
| 1940s–1950s | Public health initiatives deploying use of DDT, mostly inside homes and other sites of transmission, and drainage of breeding sites frees Europe and North America from malaria.[18][19] |
| 1970s–1990s | The malaria situation deteriorates in the 70s. Reduced control measures between 1972 and 1976, due to financial constraints, lead to a massive 2–3 fold increases in malaria cases at a global level. Heavy overuse of DDT lead to increasingly common strains of DDT-resistant mosquitos.[20][21] |
| 1990s–2000s | The World Health Organization starts to investigate artemisinin and its derivatives, finally promoting them on a large scale in the 2000s.[22] |
| 2000–2015 | Malaria incidence among populations at risk (the rate of new cases) falls by 37% globally.[23] |
2. Full Timeline
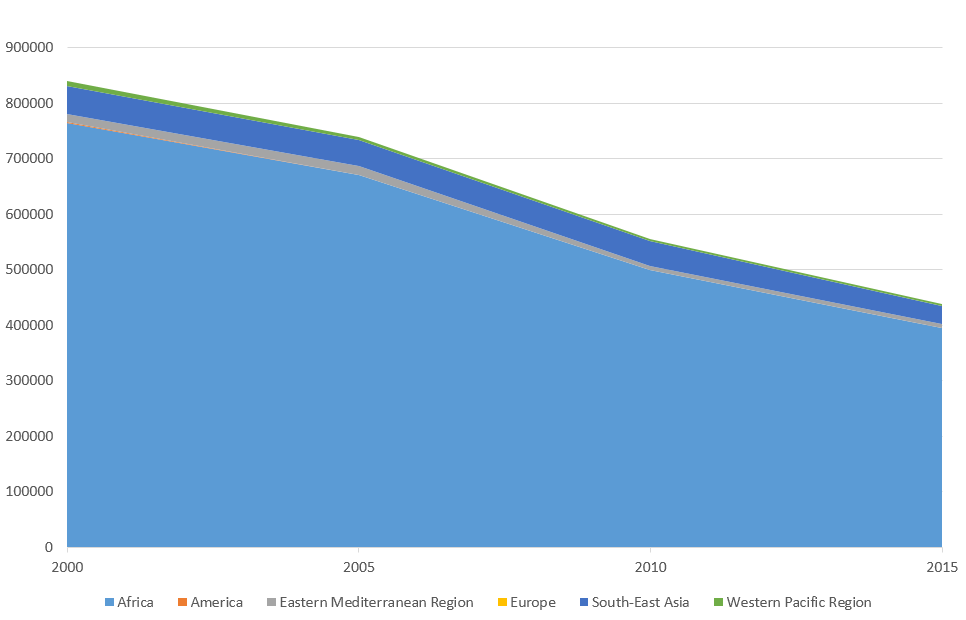
Malaria deaths per WHO region for period between 2000 and 2015.[24] All regions but South–East Asia show negligible levels compared to Africa, where the vast majority of malaria deaths occur. Cumulative.
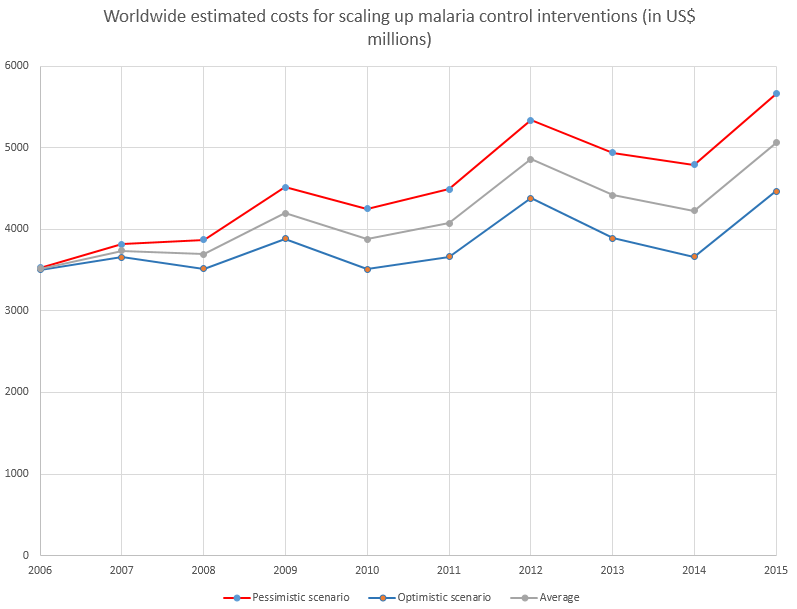
Worldwide estimated costs for scaling up malaria control interventions for the period 2006-2015 (in US$ millions)[25][26]
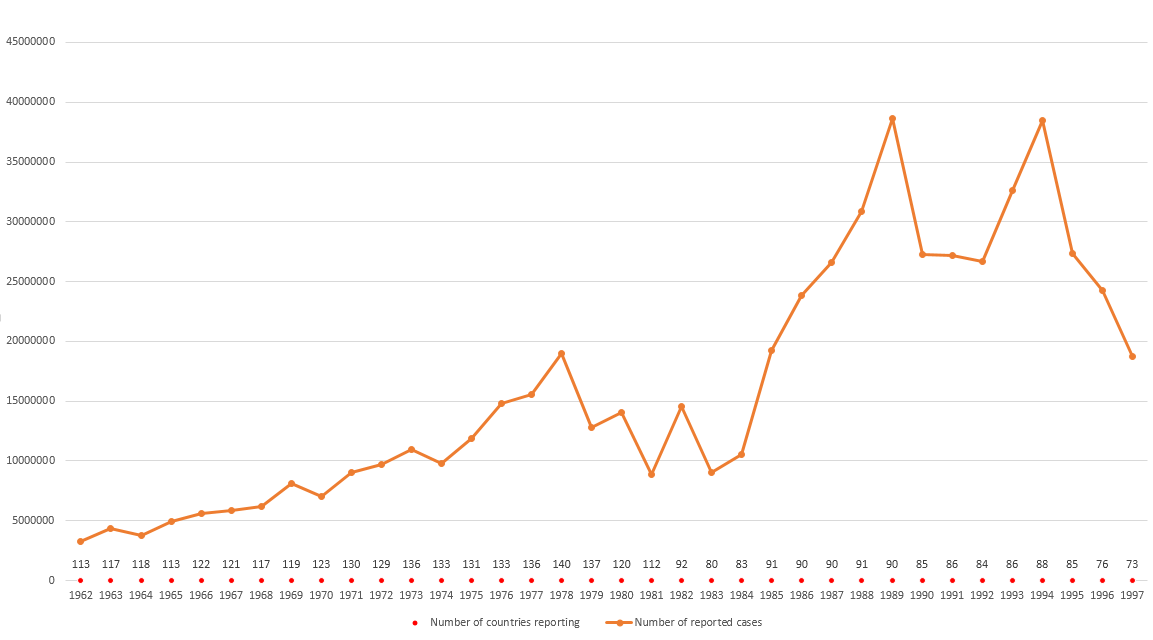
Global reported malaria cases by the WHO[27][28] for the period 1962–1997. The number of reporting countries is detailed below.
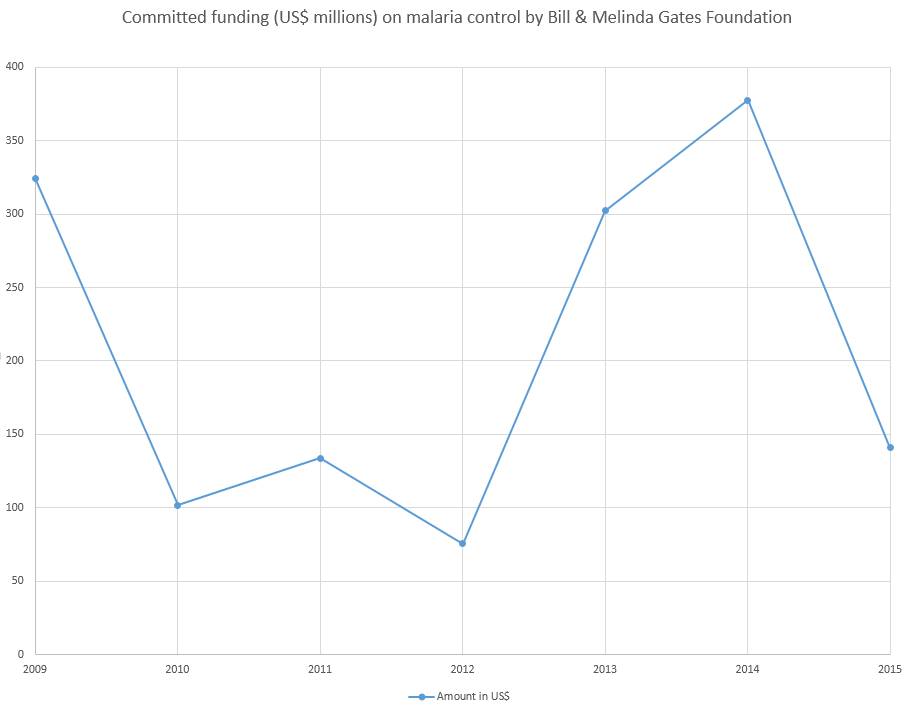
Committed funding (US$ millions) on malaria control by Bill & Melinda Gates Foundation for the period 2009–2015.[29]
| Year | Event type | Event | Geographic location |
|---|---|---|---|
| Palaeozoic era | Origin | Malaria–causing parasite plasmodium is thought to trace its origin back with the merge of the first insects.[30] | |
| 8000 BC | Epidemic | Malaria epidemic is thought to infect people, as the first big groups of population develop around the birth and expansion of agriculture.[31][32] | |
| 2000–1500 BC | Science development (symptoms) | Sumerian and Egyptian doctors describe symptoms resembling those of malaria.[4] | Middle East |
| 800 BC | Science development (vector) | Indian surgeon Sushruta indicates that malaria is caught from insect bites.[33][34] | India |
| 26 BC | Publication | Chinese text Nei Ching (The Canon of Medicine) is published. It describes several characteristic symptoms of what would later be named malaria.[35] | China |
| 340 | Science development (treatment) | The anti-fever properties of artemisinin are first described by Chinese official Ge Hong of the Jìn Dynasty.[36][37] | China |
| 1031–1095 | Science development (treatment) | Chinese polymath Shen Kuo suggests that plant species artemisia apiacea has striking antimalarial properties.[22] | China |
| 1000–1500 | Epidemic | Malaria reaches northern Europe.[4] | Europe |
| 1492 onwards | Epidemic | The arrival of Europeans introduces the malaria parasite for the first time into the Americas.[4] | Americas |
| 1632 | Jesuit missionary Bernabé Cobo brings cinchona bark from Perú to Spain .[36][38] | Spain | |
| 1633 | Science development (treatment) | Jesuit priest Antonio de la Calancha writes in his Chronicle of St Augustine about a "tree which they call the fever tree whose bark made into a powder amounting to the weight of two small silver coins and given as a beverage, cures the fevers and the tertians" (Tertians being the name for the three-day cycle of one form of malarial fever).[3][39] | South America |
| 1649 | Publication | The Schedula Romana is released. It is considered an early example of efficient anti-malaria recipe (using cinchona bark). The publication by Pietro Paolo Puccerini is attributed to the knowledge of Spanish cardinal Juan de Lugo and to have summarized trials that Lugo probably carried out.[14][40] | Italy (Rome) |
| 1663 | Publication | Italian physician Sebastiano Baldi writes the first compilation of the use of cinchona bark. His work is subsequently researched by numerous authors.[14] | Europe |
| 1712 | Science development (treatment) | Italian physician Francesco Torti writes Therapeutice Specialis, where he describes the therapeutic properties of the bark.[41] | Italy (Modena) |
| 1717 | Science development (vector) | Epidemiologist Giovanni Maria Lancisi publishes De noxiis paludum e zuviis, eorumque remediis where he suggests the possible role of mosquitoes in the transmission of malaria. Lancisi relates the prevalence of malaria in swampy areas to the presence of flies and recommends swamp drainage to prevent it.[42] | Italy (Rome) |
| 1821 | Science development (treatment) | French pharmacist Joseph Bienaimé Caventou and chemist Pierre Joseph Pelletier purify quinine (obtained from the cinchona tree) and other cinchona alkaloids. The quinine molecule is promptly tested in patients, and after numerous medical observations and case reports from all over the world, it is soon indicated that quinine is specific for ‘malarial’ (intermittent) fevers.[14] | France (Paris) |
| 1874 | Science development (prevention) | Austrian chemistry student Othmar Zeidler is credited with the first synthesis of DDT (Dichloro Diphenyl Trichloroethane). DDT is used in the second half of World War II to control malaria and typhus among civilians and troops. After the war, DDT is also used as an agricultural insecticide.[43] | Austria[44] |
| 1880 | Science development (parasite) | Charles Louis Alphonse Laveran observes parasites inside the red blood cells of infected people for the first time, proposing that malaria is caused by an organism. For this he receives the Nobel Prize in 1907.[15] | Algeria |
| 1881 | Science development (vector) | Carlos Finlay provides strong evidence that a mosquito later designated as Aedes aegypti transmits disease to and from humans.[45][46] The theory remains controversial for twenty years until confirmed in 1901 by Walter Reed.[47] | Cuba |
| 1886 | Science development (symptoms) | Italian neurophysiologist Camillo Golgi shows that there are at least two forms of malaria, one with tertian periodicity (fever every other day) and one with quartan periodicity (fever every third day). Golgi also observes that the two forms produce differing numbers of merozoites (new parasites) upon maturity and that fever coincide with the rupture and release of merozoites into the blood stream. Camillo Golgi is awarded the Nobel Prize in Physiology or Medicine in 1906.[35][38] | Italy |
| 1890 | Science development (parasite) | Italian physicians Giovanni Batista Grassi and Raimondo Feletti first introduce the names plasmodium vivax and plasmodium malariae for two of the malaria parasites that affect humans.[35] | Italy |
| 1895–1898 | Science development (vector) | British medical doctor Ronald Ross proves that malaria is transmitted by mosquitoes, and lays the foundation for the method of combating the disease. For this he receives the Nobel Prize in 1902.[15] | India |
| 1897 | Science development (parasite) | American bacteriologist William H. Welch names the malignant tertian malaria parasite plasmodium falciparum.[35] | United States |
| 1898 | Science development (vector) | An Italian team of scientists prove that anopheles claviger mosquitoes infect humans via the bite.[48] | Italy (Rome) |
| 1900–1907 | Program launch | In Italy, a series of laws establishes a national malaria control campaign (the first of its kind in the world).[49]:4 | Italy |
| 1903 | Organization | The American Society of Tropical Medicine and Hygiene is founded. Today it operates worldwide, yet it remains focused on developed countries. Research, health care and education are its main activities.[50][51][52] | United States (Philadelphia). Serves worldwide. |
| 1908 | Science development (treatment) | German chemist Paul Rabe provides the first evidence for the structure of quinine.[39][53] | Germany (Hamburg) |
| 1910 | The first case of malaria resistance against quinine is identified.[7][54][55] | ||
| 1913 | Organization | The Rockefeller Foundation is created, and through one of its branches, the International Health Division, it starts to conduct campaigns against malaria, in addition to yellow fever and hookworm.[56][57][58] | United States (New York City ) |
| 1922 | Science development (parasite) | British parasitologist John William Watson Stephens describes the fourth human malaria parasite, plasmodium ovale.[35] | United Kingdom (Liverpool)[59] |
| 1931 | Science development (parasite) | British parasitologist Robert Knowles and Bengali parasitologist Biraj Mohan Das Gupta first describe plasmodium knowlesi ( a primate malaria parasite commonly found in Southeast Asia).[35] | India (Kolkata)[60] |
| 1934–1935 | Epidemic | A malaria epidemic occurs in Sri Lanka (then known as Ceylon) that affects 27% of its population.[61][62]:4 | Sri Lanka |
| 1934 | Science development (prevention) | German scientist Hans Andersag discovers chloroquine at Bayer I.G. Farbenindustrie A.G. laboratories.[35] | Germany (Elberfeld) |
| 1939 | Science development (prevention) | Organochloride DDT's insecticidal properties are discovered by Paul Hermann Müller, who is awarded the 1948 Nobel Prize in Physiology and Medicine.[16] In the following decades, total eradication of malaria is achieved in most of the developed world due to application of DDT inside homes and other sites of transmission, and drainage programs.[18][63] | Europe, North America |
| 1940 | Achievement | Complete eradication of Anopheles gambiae from northeast Brazil and thus from the New World is achieved by the systematic application of the arsenic-containing compound Paris green to breeding places, and of pyrethrum spray-killing to adult resting places.[17] | Brazil |
| 1942 | Organization | The Office of Malaria Control in War Areas (MCWA) is established with the purpose of limiting the impact of malaria and other vector-borne diseases (such as murine typhus) during World War II around military training bases in the southern United States and its territories, where malaria is still problematic at the time.[64][65] | United States |
| 1944 | Science development (treatment) | Chemists at Imperial Chemical Industries discover antimalarial proguanil.[66] Proguanil is introduced for use in 1948.[7][54][55] | United Kingdom |
| 1945 | Science development (drug) | Antimalarial drug chloroquine is introduced for use.[7][54][55] | |
| 1946 | Science development (treatment) | Camoquin is made available as new antimalarial drug. It is proved to be effective after administration of a single therapeutic dose.[36][67] | |
| United States | |||
| 1948 | Science development (parasite) | Belgian physician Ignace Vinke and entomologist Marcel Lips identify and isolate malaria parasite plasmodium berghei from wild rodents in Central Africa.[48][68] | Central Africa |
| 1948 | Science development (parasite) | Anglo-Indian protozoologist Henry Edward Shortt and British biologist Cyril Garnham discover that malaria parasites develop in the liver before entering the blood stream.[48] | United Kingdom |
| 1948 | Organization | The World Health Organization (WHO) forms.[69] | Switzerland (Geneva). Operates worldwide. |
| 1949 | The first case of malaria resistance against proguanil is identified.[7][54][55] | Malaysia[70] | |
| 1950 | Science development (treatment) | Primaquine is introduced as new antimalarial drug. It is proven to prevent relapse and sterilizes infectious sexual plasmodia.[71] | |
| 1952 | Science development (prevention) | Dr. Mario Pinotti introduces the strategy of putting chloroquine into common cooking salt for malaria suppression, as a way of distributing the drug as a prophylactic on a wide scale. This program (using either chloroquine or pyrimethamine) becomes known as "Pinotti's method" and is employed in South America as well as Asia and Africa.[41][72] | Brazil |
| 1955 | Program launch | WHO launches the Malaria Eradication Programme. The global malaria eradication campaign is adopted by the 8th World Health Assembly and based upon the widespread use of DDT against mosquitos and of antimalarial drugs to treat malaria and eliminate the parasite in humans. Within the next decade, this program succeeds in eradicating malaria from the developed world.[17][73] | Worldwide |
| 1957 | The first case of malaria resistance against chloroquine is identified.[7][54][55] | Thailand[74] | |
| 1955–1972 | Achievement | Bulgaria, Cyprus, Dominica, Grenada, Hungary, Italy, Jamaica, Netherlands, Poland, Romania, Saint Lucia, Spain, Taiwan, Trinidad and Tobago, United States and Venezuela are certified as malaria-free by the WHO within this period.[75] | Bulgaria, Cyprus, Dominica, Grenada, Hungary, Italy, Jamaica, Netherlands, Poland, Romania, Saint Lucia, Spain, Taiwan, Trinidad and Tobago, United States Venezuela |
| 1965 | Science development (parasite) | The first human infection with plasmodium knowlesi is documented.[35] | Malaysia |
| 1967 | Antimalarial sulfadoxine/pyrimethamine is introduced. The first case of malaria resistance against sulfadoxine/pyrimethamine is identified in the same year.[7][55] | Thailand | |
| 1967 | Achievement | Malaria is eradicated from all developed countries where the disease was endemic and large areas of tropical Asia and Latin America are freed from the risk of infection.[73] | |
| 1967–1981 | Program launch | The secret military Project 523 of the People's Republic of China is aimed at finding new drugs for malaria. Over 500 Chinese scientists are recruited. The project leads to the discovery of artemisinin and derivatives,[76] also pyronaridine, lumefantrine and naphthoquine. All these antimalarial drugs are used today in therapy.[77] | China, Vietnam |
| 1969 | WHO acknowledges failure of its goal of malaria eradication and changes its goal to malaria control.[62]:8[78] | ||
| 1970 | Organization | Population Services International is created as a nonprofit global health organization with programs targeting malaria, child survival, and reproductive health. PSI provides life-saving products, clinical services and behavior change communications.[79][80] | United States (Washington, D.C.). Operates worldwide. |
| 1971 | Science development (prevention) | Antimalarial mefloquine (sold under the brand names Lariam) is first synthesized at the Experimental Therapeutics Division of the Walter Reed Army Institute of Research (WRAIR). It is number 142,490 of over 500,000 chemical compounds investigated by the United States Armed Forces to combat the devastating consequences of malaria in Vietnam.[81] Mefloquine comes into use in the mid 1980s.[82] Mefloquine is introduced for use in 1977.[7][54][55] | United States |
| 1971 | Science development (treatment) | Chinese scientists isolate the active ingredient of traditional Chinese medical drug qinghao (the blue-green herb) by extracting the artemisinin.[22][36] | China |
| 1972 | Policy | Insecticide DDT is banned for agricultural usage in the United States. Many other countries follow suit. These bans make exceptions for the use of DDT for anti-malarial purposes.[63][83] | United States |
| 1972–1987 | Achievement | Australia, Brunei, Cuba, Mauritius, Portugal, Réunion, Singapore and Yugoslavia are certified as malaria-free by the WHO within this period.[75] | Australia, Brunei, Cuba, Mauritius, Portugal, Réunion, Singapore, Yugoslavia |
| 1974 | Achievement | Malaria is eradicated from 37 countries mainly in Europe and Americas.[84] | |
| 1982 | The first case of malaria resistance against mefloquine is identified.[7][54][55] | Thailand[85] | |
| 1983 | Policy | Insecticide DDT is banned in Thailand.[86] | Thailand |
| 1986 | Policy | DDT is outlawed in the United Kingdom.[87] | United Kingdom |
| 1987 | Science development (prevention) | Colombian biochemist Manuel Elkin Patarroyo develops the first synthetic vaccine against plasmodium falciparum, the parasite that causes malaria.[15] | Colombia |
| 1992 | Organization | Malaria Foundation International (MFI) is founded as a non-profit organization dedicated to the fight against malaria. The MFI’s goals are to support awareness, education, training, research, and leadership programs to develop and apply tools to combat the disease.[88][89] | |
| 1992 | Policy | Insecticide DDT is banned in Cambodia, Laos and Vietnam.[86] | Cambodia, Laos, Vietnam |
| 1992 | Program launch | New Global Malaria Control Strategy is launched. Endorsed by a ministerial conference on malaria control, it is later confirmed by the World Health Assembly in 1993. This new strategy is based largely upon the primary health care approach and requires flexible, cost-effective, sustainable, and decentralized programs based upon disease rather than parasite control, adapted to local conditions and responding to local needs. This approach becomes successful and has positive impact in a number of countries such as Brazil, China, Solomon Islands, Philippines, Vanuatu, Vietnam, and Thailand. Its success demonstrates that malaria can be controlled by locally and currently available tools.[73] | Worldwide |
| 1996 | Antimalarial drug atovaquone is introduced. The first case of malaria resistance against atovaquone is identified in the same year.[7][54][55] | United Kingdom [90] | |
| 1997 | Organization | Multilateral Initiative on Malaria (MIM), an alliance of organizations that facilitates research on malaria, is established. MIM would also collaborate with the Disease Control Priorities Project.[91][92] | Senegal (Dakar) |
| 1998 | Program launch | Malaria Research and Reference Reagent Resource Center (MR4) is launched to provide resources like malaria reagents, protocols and technical support to the international research community. It is funded by the (NIAID).[93][94] | United States |
| 1998 | Organization | Global framework Roll Back Malaria Partnership is launched as a partnership between WHO, UNICEF, UNDP and the World Bank, with the purpose of coordinating action against malaria.[95] In 2015 RBM launched a Global Call to Action to increase coverage with preventive treatment to protect pregnant women from the devastation caused by malaria during pregnancy.[96][97] | |
| 1983 | Policy | Insecticide DDT is banned in Malaysia.[86] | Malaysia |
| 1999 | Program launch | The Research Initiative on Traditional Antimalarial Methods (RITAM) is launched as a collaboration between WHO, the Global Initiative for Traditional Systems of Health (GIFTS), the University of Oxford, and researchers and others throughout the world who are investigating or interested in the antimalarial properties of plants, with the purpose of developing or validating local herbal medicines to prevent and/or treat malaria.[98] | Tanzania (Moshi) (inaugural meeting) |
| 1999 | Organization | Medicines for Malaria Venture (MMV) is founded to reduce the burden of malaria by facilitating the discovery, development, and delivery of antimalarial medicines.[99][100] The Bill & Melinda Gates Foundation would be one of its major funders in subsequent years,[101] and it would partner with drug company Novartis.[102] | Switzerland (Geneva) |
| 2000 | The African Summit on Roll Back Malaria takes place in Abuja, Nigeria, on April 25. Signatories committed to an intensive effort to halve mortality from malaria in Africa by 2010.[103][104] | Abuja, Nigeria | |
| 2000 | Organization | Africa Fighting Malaria is founded as an NGO. It conducts research into the social and economic aspects of malaria.[105][106] | South Africa |
| 2000 | Organization | The Bill & Melinda Gates Foundation is founded by Bill and Melinda Gates with the aims of enhancing healthcare and reduce extreme poverty at a global level. Today it is the largest private foundation in the world, having donated over one billion dollars on malaria alone.[107][108] | United States (Seattle). Operates worldwide. |
| 2000 | Science development (treatment) | Roll Back Malaria Partnership launches new artemisinin combination therapy ACT.[36][109] | |
| 2001 | Policy | DDT is banned as a pesticide worldwide under the Stockholm Convention on Persistent Organic Pollutants after it is discovered to be dangerous to wildlife and the environment.[87] | Sweden (Stockholm), worldwide |
| 2001 | Organization | The Amazon Malaria Initiative is launched with the goal of preventing and controlling malaria in the Amazon basin. With support from the U.S. Agency for International Development, it has expanded into eleven countries.[110][111] | Brazil, Colombia, Ecuador, Guyana, Peru, Suriname, Bolivia, Venezuela (ceased participation), Belize, Guatemala, Honduras, Nicaragua, and Panama. |
| 2002 | Organization | The Global Fund to Fight AIDS, Tuberculosis and Malaria is founded as an international financing institution dedicated to attract and fund additional resources to stop and treat those diseases.[112] | Switzerland (Geneva) |
| 2002 | Organization | The African Malaria Network Trust (AMANET) is established. Its main goal is vaccine development, although it has expanded its aims, including other intervention measures such as antimalaria drugs and vector control.[113][114] | Tanzania (Dar es Salaam). Operates in Africa. |
| 2002 | The Malaria Journal, a peer-reviewed open access medical journal published by BioMed Central, is established.[115] | United Kingdom | |
| 2003 | Organization | The Malaria Consortium is founded as a non-profit organization dedicated to the control of malaria.[116] | United Kingdom (London). Operates in Africa and Asia. |
| 2004 | Organization | Against Malaria Foundation is set up with the aim of handling money and raising funds. Much of the funds raised by it are used to purchase bednets. | United Kingdom (London). Operates in Africa. |
| 2004 | Organization | MalariaWorld is launched as a project between the Multilateral Initiative on Malaria and the National Library of Medicine with the aim of facilitating free and unrestricted access to information on malaria. MalariaWorld has collaborated with the Malaria Eradication Scientific Alliance.[117][118] | United States (Washington, DC.) |
| 2005 | Organization | South African Malaria Initiative is launched with aims at finding new ways to prevent and treat malaria.[119][120][121] | South Africa |
| 2005 | Organization | The Innovative Vector Control Consortium is established as a research consortium. It focuses on the development of new insecticides for public health vector control and also information systems and tools in order to enable new and existing pesticides to be used more effectively.[122][123] | United Kingdom, United States, South Africa |
| 2005 | Program launch | The Malaria Atlas Project is founded.[124] Its website would launch on May 1, 2006.[125] | United Kingdom (Oxford) |
| 2006 | Organization | Malaria No More is founded. It has partnerships and focuses in advocacy to elevate malaria on the global health agenda.[126][127] | United States (Seattle). Operates worldwide. |
| 2006 | Organization | The United Nations Foundation creates the Nothing But Nets campaign to prevent malaria deaths by purchasing, distributing, and teaching the proper use of mosquito bed nets.[128] | Sub-Saharan Africa |
| 2006 | Publication | The second edition of Disease Control Priorities in Developing Countries, commonly referred to as DCP2, is published.[129] Chapter 21 of the publication is entitled "Conquering Malaria".[130] | |
| 2007–2015 | Achievement | Armenia, Maldives, Morocco, Turkmenistan and the United Arab Emirates are certified as malaria-free by the WHO within this period.[75] | Armenia, Maldives, Morocco, Turkmenistan, United Arab Emirates |
| 2008 | Organization | The Millennium Foundation for Innovative Finance for Health is established. Its project MassiveGood is meant to collect funds for combating HIV/AIDS, malaria and tuberculosis.[131][132] | United States, United Kingdom, Germany, Austria, Switzerland and Spain. Serves worldwide. |
| 2008 | Program launch | The United Methodist Church launches comprehensive anti-malaria campaign Imagine No Malaria, with aims at raising $75 million "to empower the people of Africa to overcome malaria’s burden".[133][134] | United States |
| 2008 | Program launch | The Global Malaria Action Plan (GMAP), developed by the Roll Back Malaria Partnership, is launched at the 2008 MDG Malaria Summit on September 25.[135]:2[136] | United States (New York City ) |
| 2009 | Organization | The African Leaders Malaria Alliance (ALMA) is founded by African Heads of State to use their individual and collective power to keep malaria high on the political and policy agenda.[137][138] | Africa |
| 2012 | Organization | The Malaria Eradication Scientific Alliance (MESA) is formed to conduct research on malaria elimination.[139][140] | Spain |
| 2014 | Organization | EVIMalaR is conducted as a malaria research network. Funded by the European Commission and involving at least 62 partners from 51 institutes.[141][142][143] | Europe, Africa, India and Australia. |
| 2019 | Program launch | A pilot project testing the RTS,S vaccine is launched in Malawi, Ghana, and Kenya.[144] | |
| 2020 | Science development (prevention) | Scientists discovered the Microsporidia MB microbe completely protects mosquitoes from being infected with malaria.[145] | Kenya |
The content is sourced from: https://handwiki.org/wiki/Medicine:Timeline_of_malaria
References
- Loy, Dorothy E.; Liu, Weimin; Li, Yingying; Learn, Gerald H.; Plenderleith, Lindsey J.; Sundararaman, Sesh A.; Sharp, Paul M.; Hahn, Beatrice H. (2017). "Out of Africa: origins and evolution of the human malaria parasites Plasmodium falciparum and Plasmodium vivax". International Journal for Parasitology 47 (2–3): 87–97. doi:10.1016/j.ijpara.2016.05.008. PMID 27381764. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=5205579
- Liu W; Li Y; Learn GH; Rudicell RS; Robertson JD; Keele BF; Ndjango J-BN; Sanz CM et al. (2010). "Origin of the human malaria parasite Plasmodium falciparum in gorillas". Nature 467 (7314): 420–5. doi:10.1038/nature09442. PMID 20864995. Bibcode: 2010Natur.467..420L. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2997044
- null
- Niaz Arifin, S. M.; Madey, Gregory R.; Collins, Frank H. (2016-04-11). Spatial Agent-Based Simulation Modeling in Public Health: Design .... ISBN 9781118964354. https://books.google.com/?id=UvelCgAAQBAJ&pg=PA8&lpg=PA8&dq=%22sumerian%22+%22egyptian%22+%22malaria%22+%22symptoms%22#v=onepage&q=%22sumerian%22%20%22egyptian%22%20%22malaria%22%20%22symptoms%22&f=false. Retrieved 15 December 2016.
- Gibson, M.; Nye, E. (1997-06-15). Ronald Ross: Malariologist and Polymath: A Biography. p. 23. ISBN 9780230377547. https://books.google.com/?id=oDNaCwAAQBAJ&pg=PA22&lpg=PA22&dq=%22malaria%22+%22ancient+greece%22+%22roman+empire%22#v=onepage&q=%22malaria%22%20%22ancient%20greece%22%20%22roman%20empire%22&f=false. Retrieved 15 December 2016.
- Unschuld, Paul U.. Huang Di Nei Jing Su Wen: Nature, Knowledge, Imagery in an Ancient Chinese ....
- "History of antimalarials". Medicines for Malaria Venture. http://www.mmv.org/malaria-medicines/history-antimalarials. Retrieved 16 December 2016.
- "Bad air, amulets and mosquitoes: 2,000 years of changing perspectives on malaria". Malar. J. 12 (1): 213. 2013. doi:10.1186/1475-2875-12-232. PMID 23835014. PMC 3723432. http://www.malariajournal.com/content/pdf/1475-2875-12-232.pdf.
- Wahlgren, Mats; Bejarano, Maria Teresa (August 1999). "Malaria A blueprint of 'bad air'". Nature 400 (6744): 506–507. doi:10.1038/22880. PMID 10448849. Bibcode: 1999Natur.400..506W. https://dx.doi.org/10.1038%2F22880
- "A brief history of malaria chemotherapy". J R Coll Physicians Edinb 40 (2): 172–7. 2010. doi:10.4997/JRCPE.2010.216. PMID 20695174. https://dx.doi.org/10.4997%2FJRCPE.2010.216
- Bruce-Chwatt LJ (1988). "Three hundred and fifty years of the Peruvian fever bark". Br Med J (Clin Res Ed) 296 (6635): 1486–7. doi:10.1136/bmj.296.6635.1486. PMID 3134079. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2546010
- "Was malaria present in the Amazon before the European conquest? Available evidence and future research agenda". J. Archaeol. Sci. 32 (3): 337–340. 2005. doi:10.1016/j.jas.2004.10.004. https://dx.doi.org/10.1016%2Fj.jas.2004.10.004
- "Multiple independent introductions of Plasmodium falciparum in South America". PNAS 109 (2): 511–6. 2011. doi:10.1073/pnas.1119058109. PMID 22203975. PMC 3258587. Bibcode: 2012PNAS..109..511Y. http://www.pnas.org/content/early/2011/12/19/1119058109.
- "Evaluation of Cinchona bark in the 17th and 18th centuries". The James Lind Library. http://www.jameslindlibrary.org/articles/evaluating-cinchona-bark-and-quinine-for-treating-and-preventing-malaria/. Retrieved 18 November 2016.
- "Journey of Scientific Discoveries". Malaria Site. 2015-02-25. http://www.malariasite.com/history-science/. Retrieved 15 December 2016.
- "The Nobel Prize in Physiology or Medicine 1948". Nobelprize. https://www.nobelprize.org/nobel_prizes/medicine/laureates/1948/. Retrieved 16 December 2016.
- "WHO in 60 years: a chronology of public health milestones". World Health Organization. http://www.who.int/features/history/WHO_60th_anniversary_chronology.pdf. Retrieved April 2, 2016.
- "The end of malaria in Europe: an eradication of the disease by control measures". Parassitologia 40 (1–2): 245–6. June 1998. PMID 9653750. http://www.ncbi.nlm.nih.gov/pubmed/9653750
- "Elimination of Malaria in the United States (1947–1951)". 2018-11-14. https://www.cdc.gov/malaria/about/history/elimination_us.html.
- "Malaria: Past and Present". https://www.nobelprize.org/educational/medicine/malaria/readmore/history.html. Retrieved 28 November 2016.
- Souder, William (September 4, 2012). "Rachel Carson Didn't Kill Millions of Africans". Slate. http://www.slate.com/articles/health_and_science/science/2012/09/silent_spring_turns_50_biographer_william_souder_clears_up_myths_about_rachel_carson_.html. Retrieved September 5, 2012.
- Hsu, E (June 2006). "Reflections on the 'discovery' of the antimalarial qinghao". Br J Clin Pharmacol 61 (6): 666–70. doi:10.1111/j.1365-2125.2006.02673.x. PMID 16722826. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1885105
- "Malaria Fact sheet N°94". World Health Organization. http://www.who.int/mediacentre/factsheets/fs094/en/. Retrieved 2 February 2016.
- Roser, Max (2013-11-12). "Deaths Due to Malaria". Our World in Data. https://ourworldindata.org/malaria/. Retrieved 18 November 2016.
- Nafo-Traoré, Fatoumata; Teklehaimanot, Awash; Ameneshewa, Birkinesh; Tan-Torres, Tessa; Crowell, Valerie; Delacollette, Charles; Schapira, Allan; Johns, Benjamin et al. (August 2007). "Estimated global resources needed to attain international malaria control goals". Bulletin of the World Health Organization 85: 623–630. doi:10.1590/S0042-96862007000800015. PMID 17768521. http://www.scielosp.org/scielo.php?script=sci_arttext&pid=S0042-96862007000800015. Retrieved 6 December 2016.
- "Table". SciELO. http://www.scielosp.org/img/revistas/bwho/v85n8/a15tab01.gif. Retrieved 6 December 2016.
- "Weekly epidemiological record". World Health Organization. http://www.who.int/malaria/publications/1982-1997_data_in_wer_1999_74.pdf?ua=1. Retrieved 18 November 2016.
- "World health statistics annual". World Health Organization. http://www.who.int/malaria/publications/1962-1981_data_in_world_health_statistics_1983.pdf?ua=1. Retrieved 18 November 2016.
- "Bill & Melinda Gates Foundation". IATI Registry. https://iatiregistry.org/publisher/bmgf. Retrieved 7 December 2016.
- Manguin, Sylvie; Mouchet, Jean; Carnevale, Pierre (2008-01-01). Biodiversity of Malaria in the world. ISBN 9782742009633. https://books.google.com/?id=Sk0JBAAAQBAJ&pg=PA12&lpg=PA12&dq=%22malaria%22+%22jurassic%22+%22reptiles%22#v=onepage&q=%22malaria%22%20%22jurassic%22%20%22reptiles%22&f=false. Retrieved 15 December 2016.
- Connor, Steve. "Deadly Malaria May Have Arisen With Spread of Agriculture". National Geographic. http://news.nationalgeographic.com/news/2001/06/0625_wiresmalaria.html. Retrieved 15 December 2016.
- Cliff, Andrew David; Smallman-Raynor, Matthew (2009). Infectious Diseases: Emergence and Re-emergence : a Geographical Analysis. p. 14. ISBN 9780199244737. https://books.google.com/?id=Xa4SDAAAQBAJ&pg=PA14&lpg=PA14&dq=%228000+BC%22+%22malaria%22#v=onepage&q=%228000%20BC%22%20%22malaria%22&f=false. Retrieved 15 December 2016.
- Western Journal of Surgery, Obstetrics and Gynecology, Volume 47. 1939. p. 495. https://books.google.com/?id=WQ5EAAAAYAAJ&q=%22sushruta%22+%22malaria%22&dq=%22sushruta%22+%22malaria%22. Retrieved 15 December 2016.
- Singh, J; Desai, MS; Pandav, CS; Desai, SP (2012-01-01). "Contributions of ancient Indian physicians – Implications for modern times". Journal of Postgraduate Medicine 58 (1): 73–8. doi:10.4103/0022-3859.93259. PMID 22387655. https://dx.doi.org/10.4103%2F0022-3859.93259
- "The History of Malaria, an Ancient Disease". Centers for Disease Control and Prevention. https://www.cdc.gov/malaria/about/history/. Retrieved 23 November 2016.
- "Saga of Malaria Treatment". Malaria Site. http://www.malariasite.com/tag/jesuit-bark/. Retrieved 23 November 2016.
- Rao, Yi; Zhang, Daqing; Li, Runhong (2016-09-28). Tu Youyou and the Discovery of Artemisinin: 2015 Nobel Laureate in .... ISBN 9789813109919. https://books.google.com/?id=nmZtDQAAQBAJ&pg=PA109&lpg=PA109&dq=%22340%22+%22ge+hong%22+%22artemisinin%22#v=onepage&q=%22340%22%20%22ge%20hong%22%20%22artemisinin%22&f=false. Retrieved 16 December 2016.
- Parker, Steve (2013-11-01). Kill or Cure: An Illustrated History of Medicine. ISBN 9781465422279. https://books.google.com/?id=vWwrAQAAQBAJ&pg=PA388&lpg=PA388&dq=%221632%22+%22cobo%22+%22cinchona%22#v=onepage&q=%221632%22%20%22cobo%22%20%22cinchona%22&f=false. Retrieved 23 November 2016.
- null
- Lane Furdell, Elizabeth (2001). The Royal Doctors, 1485-1714: Medical Personnel at the Tudor and Stuart Courts. p. 141. ISBN 9781580460514. https://books.google.com/?id=FTQYQ1xx6qsC&pg=PA141&lpg=PA141&dq=%221649%22+%22schedula+romana%22#v=onepage&q=%221649%22%20%22schedula%20romana%22&f=false. Retrieved 16 December 2016.
- Rosenthal, Philip J. (2001-04-01). Antimalarial Chemotherapy: Mechanisms of Action, Resistance, and New .... ISBN 9781592591114. https://books.google.com/?id=P_0qBgAAQBAJ&pg=PA16&lpg=PA16&dq=%221712%22+%22francesco+torti%22+%22bark%22#v=onepage&q=%221712%22%20%22francesco%20torti%22%20%22bark%22&f=false. Retrieved 24 November 2016.
- "Perceptions of malaria transmission before Ross' discovery in 1897". Postgrad Med J 76 (901): 738–40. 2000. doi:10.1136/pmj.76.901.738. PMID 11060174. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1741788
- Eckinger, Julie (2008-09-19). The Ethics of Intensification: Agricultural Development and Cultural Change. ISBN 9781402087226. https://books.google.com/?id=0K8qkYZdx7cC&pg=PA66&lpg=PA66&dq=%22Othmar+Zeidler%22+%221874%22+%22synthesis%22+%22DDT%22#v=onepage&q=%22Othmar%20Zeidler%22%20%221874%22%20%22synthesis%22%20%22DDT%22&f=false. Retrieved 25 November 2016.
- Jones, Richard (2013-02-15). Mosquito. ISBN 9781861899477. https://books.google.com/?id=d2N9Mxztdu4C&pg=PA152&lpg=PA152&dq=%22Othmar+zeidler%22+%22DDT%22+%22Austria%22#v=onepage&q=%22Othmar%20zeidler%22%20%22DDT%22%20%22Austria%22&f=false. Retrieved 22 December 2016.
- Faerstein, Eduardo; Winkelstein, Warren Jr (January 2010). "Carlos Juan Finlay: Rejected, Respected, and Right". Epidemiology 21 (1): 158. doi:10.1097/EDE.0b013e3181c308e0. PMID 20010221. https://dx.doi.org/10.1097%2FEDE.0b013e3181c308e0
- Finlay CJ. (1881). "El mosquito hipotéticamente considerado como agente de transmision de la fiebre amarilla". Anales de la Real Academia de Ciencias Médicas Físicas y Naturales de la Habana (18): 147–169.
- "The Etiology of Yellow Fever". JAMA 36 (7): 431–440. 1901. doi:10.1001/jama.1901.52470070017001f. https://zenodo.org/record/1447271.
- Cox, FE (2010). "History of the discovery of the malaria parasites and their vectors". Parasit Vectors 3 (1): 5. doi:10.1186/1756-3305-3-5. PMID 20205846. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2825508
- Snowden, Frank M. (2006). The Conquest of Malaria: Italy, 1900–1962. Yale University Press.
- "Who We Are". American Society of Tropical Medicine and Hygiene. http://www.astmh.org/about-astmh/about-us. Retrieved 28 November 2016.
- Le Duc, James W.; DeAcetis, Judy (2011). "Review and Assessment of the American Society of Tropical Medicine and Hygiene Travel Awards Program, 1991–2010". Am J Trop Med Hyg 85 (3): 409–13. doi:10.4269/ajtmh.2011.11-0323. PMID 21896796. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3163858
- "University's Stephen Higgs named tropical medicine society president-elect, honored for vaccine research". K-State News. http://www.k-state.edu/media/newsreleases/dec14/higgsaward12214.html. Retrieved 15 December 2016.
- "Quinine". Chemical & Engineering News. https://pubs.acs.org/cen/coverstory/83/8325/8325quinine.html. Retrieved 24 November 2016.
- Gyang, Kofi Oteng (September 2009). A Killer Called Malaria: The Disease That Kills Two People Every Minute. p. 52. ISBN 9781449019198. https://books.google.com/?id=ctMM3XTnUU0C&pg=PA52&lpg=PA52&dq=sulfadoxine%E2%80%93pyrimethamine+1967#v=onepage&q=sulfadoxine%E2%80%93pyrimethamine%201967&f=false. Retrieved 16 December 2016.
- Global Defence Against the Infectious Disease Threat. World Health Organization. 2003. ISBN 9789241590297.
- Parmar, Inderjeet (2012-04-03). Foundations of the American Century: The Ford, Carnegie, and Rockefeller. ISBN 9780231517935. https://books.google.com/?id=yR_q5sTQyloC&pg=PA40&lpg=PA40&dq=%22Rockefeller+Foundation%22+%22founded+in+1913%22#v=onepage&q=%22Rockefeller%20Foundation%22%20%22founded%20in%201913%22&f=false. Retrieved 15 December 2016.
- "International Health Division". Rockefeller Foundation. http://rockefeller100.org/exhibits/show/health/international-health-division. Retrieved 15 December 2016.
- Stapleton, Darwin H. (2004). "Lessons of history? Anti-malaria strategies of the International Health Board and the Rockefeller Foundation from the 1920s to the era of DDT.". Public Health Rep 119 (2): 206–15. doi:10.1177/003335490411900214. PMID 15192908. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1497608
- Grove, David (2014). Tapeworms, Lice, and Prions: A Compendium of Unpleasant Infections. ISBN 9780199641024. https://books.google.com/?id=FHo9AgAAQBAJ&pg=PA126&lpg=PA126&dq=%22+John+William+Watson+Stephens%22+%22liverpool%22#v=onepage&q=%22%20John%20William%20Watson%20Stephens%22%20%22liverpool%22&f=false. Retrieved 22 December 2016.
- Onder Ergonul; Can, Fusun; Akova, Murat; Madoff, Lawrence (2014-05-13). Emerging Infectious Diseases: Clinical Case Studies. ISBN 9780124201095. https://books.google.com/?id=GjdOAwAAQBAJ&pg=PA338&lpg=PA338&dq=%22+Robert+Knowles%22+%22kolkata%22#v=onepage&q=%22%20Robert%20Knowles%22%20%22kolkata%22&f=false. Retrieved 22 December 2016.
- Jones M (April 2000). "The Ceylon malaria epidemic of 1934-35: a case study in colonial medicine". Soc Hist Med 13 (1): 87–109. doi:10.1093/shm/13.1.87. PMID 11624427. https://dx.doi.org/10.1093%2Fshm%2F13.1.87
- Palmer, Michael (March 26, 2016). "The ban of DDT did not cause millions to die from malaria". http://www.science.uwaterloo.ca/~mpalmer/stuff/DDT-myth.pdf. Retrieved December 22, 2016. "failure of eradication was officially acknowledged by the WHO, and the goal restated as "control" rather than eradication, already in 1969, that is, three years before environmental concerns culminated in the ban on DDT in the United States"
- "DDT: From miracle chemical to banned pollutant". http://www.swissinfo.ch/eng/ddt--from-miracle-chemical-to-banned-pollutant/3253684. Retrieved 28 November 2016.
- "Elimination of Malaria in the United States (1947 — 1951)". Centers for Disease Control and Prevention. https://www.cdc.gov/malaria/about/history/elimination_us.html. Retrieved 24 November 2016.
- Dumenil, Lynn (2012). The Oxford Encyclopedia of American Social History. p. 171. ISBN 9780199743360. https://books.google.com/?id=N-RMAgAAQBAJ&pg=RA1-PA171&lpg=RA1-PA171&dq=%22Office+of+Malaria+Control+in+War+Areas+was%22#v=onepage&q=%22Office%20of%20Malaria%20Control%20in%20War%20Areas%20was%22&f=false. Retrieved 15 December 2016.
- Rappoport, Zvi (2007-03-13). The Chemistry of Anilines, Part 1. ISBN 9780470871720. https://books.google.com/?id=wckakYtwttMC&pg=PA54&lpg=PA54&dq=%22proguanil%22+%221944%22#v=onepage&q=%22proguanil%22%20%221944%22&f=false. Retrieved 25 November 2016.
- "Camoquin". American Journal of Tropical Medicine and Hygiene. http://www.ajtmh.org/content/s1-31/2/212.extract. Retrieved 25 November 2016.
- Vanderberg, Jerome P. (January 2009). "Reflections on Early Malaria Vaccine Studies, the First Successful Human Malaria Vaccination, and Beyond". Vaccine 27 (1): 2–9. doi:10.1016/j.vaccine.2008.10.028. PMID 18973784. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2637529
- Markel, Howard (January 7, 2014). "Worldly approaches to global health: 1851 to the present". Public Health 128 (2): 124–8. doi:10.1016/j.puhe.2013.08.004. PMID 24412079. Archived from the original on April 18, 2016. https://web.archive.org/web/20160418174941/http://s2.medicina.uady.mx/observatorio/docs/ee/ac/EE2014_Ac_Markel.pdf. Retrieved April 5, 2016.
- Peters, Wallace (2013-11-09). Antimalarial Drugs I: Biological Background, Experimental Methods, and Drug .... ISBN 9783662353264. https://books.google.com/?id=K2vwCAAAQBAJ&pg=PA435&lpg=PA435&dq=%221949%22+resistance+against+proguanil+is+identified#v=onepage&q=%221949%22%20resistance%20against%20proguanil%20is%20identified&f=false. Retrieved 22 December 2016.
- "Primaquine Therapy for Malaria". Oxford Journal. http://cid.oxfordjournals.org/content/39/9/1336.full.pdf. Retrieved 25 November 2016.
- Giglioli, G; Rutten, FJ; Ramjattan, S (1967). "Interruption of Malaria Transmission by Chloroquinized Salt in Guyana". Bull World Health Organ 36 (2): 283–301. PMID 4864651. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2476374
- Trigg, PI; Kondrachine, AV. (1998). "Commentary: malaria control in the 1990s.". Bull World Health Organ 76 (1): 11–6. PMID 9615492. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2305627
- M. Packard, Randall (2014). "The Origins of Antimalarial-Drug Resistance". The New England Journal of Medicine 371 (5): 397–399. doi:10.1056/NEJMp1403340. PMID 25075832. https://dx.doi.org/10.1056%2FNEJMp1403340
- "Malaria Free countries". World Health Organization. http://www.who.int/malaria/areas/elimination/overview/en/. Retrieved 25 November 2016.
- Dondorp, Arjen M.; Day, Nick P.J. (2007). "The treatment of severe malaria". Transactions of the Royal Society of Tropical Medicine and Hygiene 101 (7): 633–634. doi:10.1016/j.trstmh.2007.03.011. PMID 17434195. https://dx.doi.org/10.1016%2Fj.trstmh.2007.03.011
- Cui, Liwang; Su, Xin-zhuan (2009). "Discovery, mechanisms of action and combination therapy of artemisinin". Expert Review of Anti-infective Therapy 7 (8): 999–1013. doi:10.1586/eri.09.68. PMID 19803708. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2778258
- Tanner, Marcel; de Savigny, Don (February 2008). Malaria eradication back on the table. World Health Organization. PMID 18297155. http://www.who.int/bulletin/volumes/86/2/07-050633/en/. Retrieved December 23, 2016. "When the aspiration of global eradication was abandoned in 1969".
- "PSI at a Glance". Population Services International. 2014-09-25. http://www.psi.org/about/at-a-glance/. Retrieved September 2, 2016.
- "Population Services International: Funding Growth". Bridgespan Group. http://www.bridgespan.org/getattachment/d7e46705-2a3b-47a5-a531-3634b19963d6/Profile-Population-Services-International.aspx. Retrieved September 2, 2016.
- "The Strange History of Lariam". http://rxisk.org/the-strange-history-of-lariam/. Retrieved 24 November 2016.
- Croft, Ashley M (April 2007). "A lesson learnt: the rise and fall of Lariam and Halfan". J R Soc Med 100 (4): 170–4. doi:10.1258/jrsm.100.4.170. PMID 17404338. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1847738
- Erik M. Conway, Naomi Oreskes, Merchants of Doubt, 2010, p. 217
- Gupte, Suraj (1999). Recent advances in pediatrics. ISBN 9788171796564. https://books.google.com/?id=P1gMTqdo1boC&pg=PA143&lpg=PA143&dq=%22malaria+was+eradicated%22+%22in+1900..2015%22#v=onepage&q=%22malaria%20was%20eradicated%22%20%22in%201900..2015%22&f=false. Retrieved 24 November 2016.
- Mehlhorn, Heinz (2008-01-02). Encyclopedia of Parasitology: A-M. p. 596. ISBN 9783540489948. https://books.google.com/?id=Jpg1ysgVn-AC&pg=PA596&lpg=PA596&dq=%221982%22+resistance+against+mefloquine#v=onepage&q=%221982%22%20resistance%20against%20mefloquine&f=false. Retrieved 22 December 2016.
- "DDT". Canadian POPs Trust Fund. http://www.popstoolkit.com/about/chemical/ddt.aspx. Retrieved 28 November 2016.
- null
- "Against Malaria Foundation Charity In Stone Mountain Georgia". Charity Vault. http://www.charity-charities.org/Georgia-charities/StoneMountain-1661483.html. Retrieved 28 November 2016.
- Dziedzic, Nancy G. (2010). Perspectives on Diseases and Disorders. Greenhaven Press/Gale Cengage Learning. ISBN 9780737743791. https://books.google.com/?id=-wJaAAAAYAAJ&q=%22Malaria+Foundation+International+is+a%22&dq=%22Malaria+Foundation+International+is+a%22. Retrieved 15 December 2016.
- "Atovaquone/proguanil". http://adisinsight.springer.com/drugs/800009014. Retrieved 22 December 2016.
- "About MIM". Multilateral Initiative on Malaria. http://www.mimalaria.org/eng/aboutmim.asp. Retrieved May 19, 2016.
- "Multilateral Initiative on Malaria (MIM)". World Health Organization. http://www.who.int/tdr/grants/workplans/mim_bis/en/. Retrieved May 19, 2016.
- "Malaria Research and Reference Reagent Resource Center". ATCC. https://www.atcc.org/en/About/Grants_and_Contracts/Malaria_Research_and_Reference_Reagents.aspx. Retrieved 28 November 2016.
- Wu, Y; Fairfield, AS; Oduola, A; Cypess, RH (2001). "The Malaria Research and Reference Reagent Resource (MR4) Center--creating African opportunities.". Afr J Med Med Sci 30 Suppl: 52–4. PMID 14513940. http://www.ncbi.nlm.nih.gov/pubmed/14513940
- "The Global Partnership for a Malaria-free World". http://www.rollbackmalaria.org/microsites/wmd2012/pr2011-09-12.html. Retrieved 23 November 2016.
- "Africa: Roll Back Malaria Partnership Launches Global Call to Action to Increase Coverage of Preventive Treatment for Malaria During Pregnancy Throughout Sub-Saharan Africa.". http://allafrica.com/stories/201504241864.html. Retrieved 23 November 2016.
- "Rolling Back Malaria". World Health Organization. http://www.who.int/whr/1999/en/whr99_ch4_en.pdf. Retrieved 15 December 2016.
- "Essential Medicines and Health Products Information Portal". World Health Organization. http://apps.who.int/medicinedocs/en/d/Js2297e/7.6.html. Retrieved 29 November 2016.
- "About us". Medicines for Malaria Venture. http://www.mmv.org/about-us. Retrieved September 2, 2016.
- "Medicines for Malaria Venture (MMV)". World Health Organization. http://www.who.int/phi/documents/medicines_for_malaria_venture.pdf. Retrieved September 2, 2016.
- "Gates Foundation Commits $258.3 Million for Malaria Research and Development". Bill & Melinda Gates Foundation. October 1, 2015. http://www.gatesfoundation.org/Media-Center/Press-Releases/2005/10/Gates-Foundation-Commits-2583-Million-for-Malaria-Research. Retrieved September 2, 2016.
- "Novartis expands partnership with Medicines for Malaria Venture to develop next-generation antimalarial treatment". June 15, 2016. https://www.novartis.com/news/media-releases/novartis-expands-partnership-medicines-malaria-venture-develop-next-generation. Retrieved September 2, 2016.
- "The Abuja Declaration and the Plan of Action". http://www.rollbackmalaria.org/microsites/wmd2011/abuja_declaration_final.html. Retrieved January 19, 2017.
- "The Abuja Declaration and the plan of action. An extract from the African Summit on Roll Back Malaria". World Health Organization. http://www.who.int/malaria/publications/atoz/whocdsrbm200346/en/. Retrieved January 19, 2017.
- "Africa Fighting Malaria". https://www.devex.com/organizations/africa-fighting-malaria-52449. Retrieved 24 November 2016.
- Appiah, Anthony; Gates, Henry Louis (2010). Encyclopedia of Africa, Volume 1. p. 117. ISBN 9780195337709. https://books.google.com/?id=A0XNvklcqbwC&pg=RA1-PA117&lpg=RA1-PA117&dq=%22Africa+Fighting+Malaria%22#v=onepage&q=%22Africa%20Fighting%20Malaria%22&f=false. Retrieved 15 December 2016.
- The Challenge of Global Health Foreign Affairs, January/February 2007 http://www.foreignaffairs.org/20070101faessay86103/laurie-garrett/the-challenge-of-global-health.html
- Donald G. McNeil Jr., Gates Foundation's Influence Criticized, N.Y. Times, Feb 16, 2008 https://www.nytimes.com/2008/02/16/science/16malaria.html?_r=0
- "Artemisinin combination therapy for the treatment of childhood malaria in Sub-Saharan Africa: Efficacy, safety and policy considerations". ResearchGate. https://www.researchgate.net/publication/288172588. Retrieved 25 November 2016.
- "Amazon Malaria Initiative". United States Agency for International Development. http://www.usaidami.org/#sthash.lwwx7Hzp.dpbs. Retrieved 28 November 2016.
- "THE AMAZON MALARIA INITIATIVE". World Health Organization. http://apps.who.int/medicinedocs/documents/s21966en/s21966en.pdf. Retrieved 15 December 2016.
- "The Global Fund Overview". The Global Fund to Fight AIDS, Tuberculosis and Malaria. http://www.theglobalfund.org/en/overview/. Retrieved 28 November 2016.
- Kilama, WL; Chilengi, R; Wanga, CL (December 2007). "Towards an African-driven malaria vaccine development program: history and activities of the African Malaria Network Trust (AMANET).". Am. J. Trop. Med. Hyg. 77 (6 Suppl): 282–8. doi:10.4269/ajtmh.2007.77.282. PMID 18165504. https://dx.doi.org/10.4269%2Fajtmh.2007.77.282
- "African Malaria Network Trust". Health Systems Trust. http://www.hst.org.za/category/social-tags/african-malaria-network-trust. Retrieved 15 December 2016.
- Hommel, Marcel (2010). "10 years of Malaria Journal: how did Open Access change publication patterns?". Malaria Journal 9: 284. doi:10.1186/1475-2875-9-284. ISSN 1475-2875. PMID 20946649. "BioMed Central which is now part of the Springer Group, publishes 206 peer-reviewed Open Access journals, including Malaria Journal, started in 2002, and Parasite & Vectors, started in 2008.". http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3020680
- "Malaria Consortium 2003-2013: a decade in communicable disease control and child health". Malaria Consortium. http://www.malariaconsortium.org/resources/pubdev/287/malaria-consortium-2003-2013-a-decade-in-communicable-disease-control-and-child-health. Retrieved 28 November 2016.
- "About Us". Malaria Eradication Scientific Alliance. http://www.malariaeradication.org/about-us. Retrieved 15 December 2016.
- "MalariaWorld". https://malariaworld.org/about. Retrieved 28 November 2016.
- "South Africa Launches Collaborative Malaria Initiative That Aims To Develop New Treatment, Prevention Methods". 2009-06-11. http://khn.org/morning-breakout/dr00035289/. Retrieved 24 November 2016.
- "Malaria Foundation International". http://www.malaria.org/index.php?option=com_search&Itemid=99999999&searchword=initiative&searchphrase=any&ordering=newest&limit=25&limitstart=0. Retrieved 15 December 2016.
- Chibale, Kelly; Davies-Coleman, Mike; Masimirembwa, Collen (2012-08-09). Drug Discovery in Africa: Impacts of Genomics, Natural Products, Traditional .... ISBN 9783642281754. https://books.google.com/?id=4gsSO4B_2ekC&pg=PA8&lpg=PA8&dq=%22South+African+Malaria+Initiative%22#v=onepage&q=%22South%20African%20Malaria%20Initiative%22&f=false. Retrieved 15 December 2016.
- Hemingway, J. (2014). "The role of vector control in stopping the transmission of malaria: threats and opportunities". Philosophical Transactions of the Royal Society B: Biological Sciences 369 (1645): 20130431. doi:10.1098/rstb.2013.0431. PMID 24821917. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4024224
- Knapp, Jennifer; Malone, David; Hamon, Nicholas; Richardson, Jason H.; Macdonald, Michael (2015). "Disruptive technology for vector control: the Innovative Vector Control Consortium and the US Military join forces to explore transformative insecticide application technology for mosquito control programmes". Malar J 14: 371. doi:10.1186/s12936-015-0907-9. PMID 26409879. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4583753
- "MAP Researchers". Malaria Atlas Project. http://www.map.ox.ac.uk/about-map/map-team/. Retrieved January 9, 2017. "The Malaria Atlas Project (MAP) was founded in 2005"
- Hay, Simon I; Snow, Robert W (December 5, 2006). "The Malaria Atlas Project: Developing Global Maps of Malaria Risk". PLOS Medicine 3 (12): e473. doi:10.1371/journal.pmed.0030473. PMID 17147467. "The MAP Web site (http://www.map.ox.ac.uk) was launched on May 1, 2006, to further the aims and ambitions of MAP.". http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=1762059
- "Malaria No More". United Nations Foundation. http://www.unfoundation.org/what-we-do/partners/organizations/malaria-no-more.html. Retrieved 28 November 2016.
- "Malaria No More". Nothing But Nets. http://www.nothingbutnets.net/partners/malaria-no-more.html. Retrieved 15 December 2016.
- "About us". Nothing But Nets. http://www.nothingbutnets.net/new/about-us.html. Retrieved 16 December 2016.
- "About the Project". http://dcp-3.org/about-project. Retrieved March 30, 2016.
- "DCP2 – Chapters". http://dcp-3.org/dcp2/chapters. Retrieved January 17, 2017.
- "Taskforce on Innovative International Financing for Health Systems: showing the way forward". http://www.who.int/bulletin/volumes/88/6/09-075507/en/. Retrieved 4 September 2016.
- "PR Newswire: Millennium Foundation Announces Massive Good – Solidarity Movement to Help Finance Health Care for World's Poor". World Health Organization. http://www.who.int/pmnch/events/2009/20090923millenniumfoundationpr.pdf. Retrieved 15 December 2016.
- "Imagine No Malaria". http://www.umcmission.org/explore-our-work/global-health/imagine-no-malaria. Retrieved 24 November 2016.
- Elliott, Stuar (18 April 2011). "Campaign Seeks to Take a 'Bite' Out of Disease". New York Times. https://www.nytimes.com/2011/04/18/business/media/18adnewsletter1.html. Retrieved 15 December 2016.
- "2008 MDG Malaria Summit: World Leaders Unite – Summary Report". 2008. Archived from the original on July 18, 2011. https://web.archive.org/web/20110718134619/http://www.rollbackmalaria.org/docs/mdg2008SummaryReport.pdf. "Dr. Coll-Seck, Executive Director of the Roll Back Malaria Partnership, opened the Summit by formally launching the Global Malaria Action Plan (GMAP)"
- "2008 Millennium Development Goals Malaria Summit – Kaiser Network webcast of the event". Henry J. Kaiser Family Foundation. September 25, 2008. Archived from the original on April 10, 2010. https://web.archive.org/web/20100410223014/http://www.kaisernetwork.org/health_cast/hcast_index.cfm?display=detail&hc=2996.
- "Who we are". African Leaders Malaria Alliance. http://alma2030.org/sites/default/files/reference-document/alma_infosheet_0.pdf. Retrieved 28 November 2016.
- McCrea, Jennifer; Walker, Jeffrey C.; Weber, Karl (2013-09-24). The Generosity Network: New Transformational Tools for Successful Fund-Raising. ISBN 9780770437800. https://books.google.com/?id=cAv8hlyew6oC&pg=PA94&dq=%22African+Leaders+Malaria+Alliance%22#v=onepage&q=%22African%20Leaders%20Malaria%20Alliance%22&f=false. Retrieved 15 December 2016.
- "Iniciativa Agenda de investigación para la erradicación de la malaria (malERA)". Instituto de Salud Global Barcelona. http://www.isglobal.org/-/malaria-eradication-research-agenda-malera-initiative. Retrieved 28 November 2016.
- "Malaria Eradication Scientific Alliance". MalariaWorld. https://malariaworld.org/blog/malaria-eradication-scientific-alliance. Retrieved 15 December 2016.
- "Evimalar". http://conservativeeurope.com/downloads/publications/aVicky%20Ford%20Research%20Oct%202012.pdf. Retrieved 28 November 2016.
- Waters, Andrew P. (2013). "EVIMalaR — a model for international cooperation in scientific research". Nature 11 (8): 505–506. doi:10.1038/nrmicro3079. https://dx.doi.org/10.1038%2Fnrmicro3079
- "Final Report Summary – EVIMALAR (Towards the establishment of a permanent European Virtual Institute dedicated to Malaria Research". CORDIS. http://cordis.europa.eu/result/rcn/176027_en.html. Retrieved 15 December 2016.
- "Malaria vaccine launched in Kenya: Kenya joins Ghana and Malawi to roll out landmark vaccine in pilot introduction" (Press release). Homa Bay: World Health Organization. 13 September 2019. Retrieved 2019-10-22. https://www.afro.who.int/news/malaria-vaccine-launched-kenya-kenya-joins-ghana-and-malawi-roll-out-landmark-vaccine-pilot
- Herren, Jeremy K.; Mbaisi, Lilian; Mararo, Enock; Makhulu, Edward E.; Mobegi, Victor A.; Butungi, Hellen; Mancini, Maria Vittoria; Oundo, Joseph W. et al. (2020-05-04). "A microsporidian impairs Plasmodium falciparum transmission in Anopheles arabiensis mosquitoes". Nature Communications (Springer Science and Business Media LLC) 11 (1). doi:10.1038/s41467-020-16121-y. ISSN 2041-1723. https://dx.doi.org/10.1038%2Fs41467-020-16121-y
