Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Health Care Sciences & Services
The increase in life expectancy and population ageing are currently significant societal concerns. Pharmacist intervention is a way to ensure the correct use of medicines and adherence to therapy, helping to prevent drug interactions and adverse drug reactions, thus improving health and preventing further medication-related problems in older adults.
- pharmacists
- older adults
- medication management
- healthy ageing
- disease prevention
1. Introduction
The increase in life expectancy and population ageing are currently significant societal concerns. The ageing process can be defined as an undergoing process of biological, psychological, and social change that occurs throughout each life cycle, starting before birth [1,2]. Although not consensual, a person aged 65 or older is referred to as an older adult, regardless of gender or physical condition [3]. According to the World Health Organization (WHO) [4], health status, autonomy, social participation, and level of independence may differ among each age group. These variations should be considered when developing policies and advisory programs for older adults.
According to data from the National Strategy for Active and Healthy Aging (ENEAS) [5], Portugal, likemost developed countries, has registered continuous demographic ageing in recent decades. An increase in the older adult population and longevity and the reductions in the younger population and birth rate are the main reasons for the current demographic situation.
In 2021, people aged 65 or more represented 23.4% of the population living in Portugal [6]. In the same year, the aging ratio (+65 per 100 < 15) was 182.1% compared to 27.3% in 1960 [7]. In the 2018–2020 triennium, life expectancy at birth was estimated at 78.07 years for men and 83.67 years for women [8]. OECD statistics regarding the health-related quality of life show that only 46% of the Portuguese population consider themselves in good health, a much lower percentage than the OECD average (69%). In 2019, Portugal had one of the lowest scores in perceived health status compared with other OECD countries [9], and 38% of the population had two or more chronic conditions [10]. In 2020, Eurostat concluded that although life expectancy at age 65 in Portugal was within the European Union (EU) average (EU, 21 years; Portugal, 21.6 years), expected healthy life years were below the EU average (EU, 9.8 years; Portugal 7.7 years). Furthermore, the discrepancy in expected healthy life years between sexes was larger in Portugal than in the EU. While in the EU, women had a higher number of healthy life years (10.1 vs 9.5 in men), in Portugal, the number of healthy life years for women was lower than for men (7.1 vs 8.4 years, respectively) [11]. These results justify the need for initiatives aimed at improving these indicators.
Increased demographic ageing, associated with the high prevalence of multimorbidity in older adults, strongly impacts society and threatens the sustainability of health care systems. In addition, physiological changes, multiple comorbidities, and a higher prevalence of chronic diseases can lead to polymedication in most elderly patients. Interventional strategies and policy frameworks should include multidisciplinary teams to increase health literacy, instigate active ageing and improve health outcomes [12].
Promoting active and healthy ageing can improve the well-being and the quality of life of older adults [5]. Community pharmacists, as highly qualified and accessible health professionals, play a pivotal role in promoting active and healthy ageing [13]. Acting at various levels and in articulation with other professionals, they contribute to achieving positive health outcomes. Pharmacist intervention to ensure the correct use of medicines and adherence to therapy helps to prevent drug interactions and adverse drug reactions, thus improving health and preventing further medication-related problems in older adults [14]. However, Portuguese health policies do not mention the importance of pharmacist intervention in the promotion of healthy ageing or the impact of their intervention in different care settings.
2. The Importance of the Pharmacist in the Follow-Up of Older Adults
Demographic ageing has increased the number of patients with multiple co-existing pathologies, which are inevitably associated with polymedication [66,67]. Therefore, pharmacies are pivotal in providing health care to older adults.
Pharmacists, as primary caregivers with privileged access to older adults, are highly qualified and trusted professionals that play a significant role in medication management [68]. Their intervention can help to reduce non-adherence, drug interactions, and other medication-related problems. They can also provide medication review services and contribute to simplifying medication regimens [69]. As public health agents, pharmacists are responsible for improving health literacy and the rational use of medicines [38].
In Portugal, Decree-Law n.0 307/2007 of 31 August [70] establishes the legal framework for community pharmacies. Ordinance No. 1429/2007 of 2 November [71] defines the pharmaceutical and other health and wellness promotion services that community pharmacies can provide. Domiciliary support, the administration of medicines and vaccines, early screening and testing, pharmaceutical care programs, health education programs, medication reconciliation and management, dose administration aids (DAAs), compounding, and emergency care are some services offered by Portuguese pharmacies. Disease prevention, the promotion of healthy lifestyles, and health literacy campaigns and programs are other valuable services undertaken by community pharmacists.
Interventions targeting older adults have been a major priority of the Portuguese National Health Plan (PNS) since 2004 [72]. Pharmaceutical activity should be articulated with the patients and their caregivers, as well as with other health professionals [73].
Some of the primary areas of pharmaceutical intervention in older-patient-oriented care may include: (i) promoting the correct, effective, and safe use of medicines while dispensing, providing medication review and reconciliation services, and through dose administration aid; (ii) promoting health literacy and informal caregiver training; (iii) medication management in long-term care facilities; (iv) domiciliary support; (v) identifying suspected at-risk patients; (vi) promoting active and healthy ageing.
Pharmaceutical activity is patient focused. The essential preventive and therapeutic services provided by pharmacists are crucial in maintaining/improving patients’ health and quality of life, reducing healthcare costs through therapeutical reconciliation and deprescription, and changing hospitalisation profiles (less frequent and less time in hospital care), since pharmacists can perform health management interventions across many disease states [74].
2.1. Promoting the Correct, Effective, and Safe Use of Medicines
The responsible use of medications is essential for the sustainability of healthcare systems. It bears benefits to individuals and society and provides economic gains. The global annual burden of medication-related problems is estimated to equal 42 billion USD [75].
To help overcome medication-related problems, the WHO [32,76] and many countries worldwide [77,78,79] have undertaken awareness campaigns to promote the rational use of medicines and encourage health professionals to develop public education programs to help ensure good health outcomes.
Among health professionals, pharmacists play an important role in this context. According to the current Portuguese legal framework, community pharmacies can implement “Pharmaceutical Care Programs”. In these programs, pharmacists review patient medication and evaluate their pharmacotherapeutic outcomes to improve medication use, reduce negative results, and enhance therapy safety and effectiveness [80,81,82]. The services rendered by pharmacies are in accordance with the Portuguese National Plan for the Safety of Patients 2015-2020 [83] and the Portuguese National Plan for the Safety of Patients 2021–2026 [84], which refer to the need to increase safety in the use of medication.
Pharmacotherapeutic follow-up, one of the most relevant areas of pharmaceutical care, is a patient-focused service that addresses health problems, health promotion, disease prevention, medication management, and health education [38]. This service may help improve patients’ quality of life, especially in older patients with complex therapeutic regimens due to simultaneous underlying health-related conditions [85].
Therefore, pharmacists have an active role in promoting the correct use of medicines, contributing to the success of the therapy, and reducing health-related costs [86].
In summary, Portuguese pharmacists can intervene in the following areas: (a) drug dispensation; (b) medication review; (c) medication reconciliation; and (d) dose administration aids.
2.1.1. Drug Dispensation
When dispensing any medicine, the pharmacist must provide the patient or their caregiver with all the information necessary to ensure their correct use. The importance of medication adherence must be explained, and the patient should be informed of the risks associated with therapeutic non-compliance. The pharmacist should also be available to clarify any doubts that occur during treatment, provide follow-up services and refer the patient to a physician when necessary [87]. The pharmacist should briefly review the medication to detect any drug-related problems (such as interactions or duplication) when dispensing medicines. In addition, pharmacists represent an important formal support, as being seen as health professionals they give credibility and confidence to the client [68].
2.1.2. Medication Review Service (RevM)
In 2018, Pharmaceutical Care Network Europe defined medication review as a “structured evaluation of patient’s medicines with the aim of optimising medicines use and improving health outcomes.” This entails detecting drug-related problems and recommending interventions [88]. Medication review thus correlates the Best Possible Medication History with the patient’s morbidities, preferences, or geriatric syndromes to produce a personalised medication strategy aligned with patient preferences and goals. This review can be performed whenever relevant, either in acute situations or periodically [89], to help patients to correctly manage, understand, and use their medicines [90].
Although RevM can be applied to all types of patients [89], those living in care homes, with complex therapeutic regimes, on medicines frequently related to medication errors, severely frail, or patients using potentially addictive medication should be prioritised [91]. RevM can also be performed at home and in long-term care facilities, always aiming to improve the quality of life of older adult patients.
Some situations can also prompt the need for a medication review, such as when patients are admitted to the hospital following a suspected adverse drug reaction, when they express concern with multiple medicine regimens, or when a health/care professional raises concerns regarding the patient’s capability to manage their medication [91].
When performing a medication review, the pharmacist must consider all the medicines the patient is using, including not only prescription and over-the-counter medication but also vitamin/mineral supplements and herbal/traditional medicines [91]. Furthermore, the following should be considered: the patient’s and caregiver’s views, knowledge, and questions concerning their medications; the safety of each drug; compliance with use; the patient’s risk factors for developing adverse drug events; and the potential requirement for monitoring [89].
Drug-related problems represent the most common reasons for hospital admissions and mortality in primary care [92]. It is estimated that if all precautions were taken, 30% to 55% of these problems would be prevented [93].
The medicine review service allows one to identify and help to solve issues with adherence to therapy, dosing, unintentional duplications, adverse reactions, drug interactions, and incorrect dosage, among others [94]. By assisting patients in managing their therapeutic regimens, pharmacists can help to reduce medication errors and contribute to increased adherence to therapy. As integrated members of multidisciplinary teams, they can easily share patient-related information with other health professionals and help improve patient care [94,95].
Worldwide, there are already many programmes for medication management where pharmacists play important roles. In Australia, pharmacists are included in a programme called “Home Medicines Review”, where an accredited pharmacist reviews medication use, helps to minimise adverse reactions, and improves health literacy [96]. Canada’s health system provides a pharmacist consultation called “MedsCheck”, where pharmacists interview the patients and review the patients’ prescribed and non-prescription medicines [97]. In England, pharmacists perform structured medication review in patients with complex therapeutical regimens [98], and they are also allowed to prescribe medicines as independent prescribers [99]. From an economic point of view, pharmacists have an impact on decreasing total health expenditures, decreasing unnecessary care, and decreasing societal costs, although further research is needed to support future payment models [100].
Portugal has already some health policies that highlight pharmacists’ skills, although no specific mention is made of these professionals [101,102]. Félix and colleagues estimated that community pharmacy services in Portugal provide a quality-of-life gain of 8.3%, resulting in savings of over 800 million EUR [38], despite the fact that most services performed by pharmacists are not remunerated and are paid by their users [101]. A study from Paiva et al. showed that of 88 polymedicated participants, 92.2% were willing to pay for a pharmacotherapy management service, such as medication review and pharmacotherapy follow-up [14]. Medication review remains to be fully implemented in Portugal, despite the existence of national and international guidelines. The lack of communication between pharmacists and other healthcare professionals, the fact that pharmacists do not have access to the full clinical information of patients, and a lack of support by the Portuguese health authorities are some of the reasons that may help to explain the delayed implementation of this pharmaceutical service [103].
2.1.3. Medication Reconciliation Service (RecM)
RecM is a process that aims to obtain the Best Possible Medication History of a patient, gathering all medicines information provided by the patient, their family/caregiver, general practitioner, and community pharmacist. Therefore, the health professional, preferably the pharmacist, documents all medicines (prescribed and over the counter), supplements, and herbal products [104]. The main goal is to identify and correct drug discrepancies such as omissions, duplications, or dosing errors [89], updating the patient’s information through all health care services [104].
Both RecM and RevM are processes with the purpose of increasing not only patient safety but also therapeutic effectiveness and efficiency. While RevM is a structured evaluation of a patient’s medications with the stated goal of detecting and solving drug-related problems, RecM is defined as the formal process of collecting a complete and accurate list of each patient ’s current medications with the objective of detecting and solving discrepancies. Therefore, medication reconciliation can be considered an automatic pre-requisite for a medication review, as the medication list should be as accurate as possible before it can be critically appraised.
According to Directorate-General of Health (DGS—Direção-Geral da Saúde) Standard 018/2016 [102], “medication reconciliation is a process that helps to keep each patient’s list of medication up-to-date, as well as other important information, including adverse reactions to medications and allergies, avoiding discrepancies between their usual medication and the medication instituted at each time of care transition”. In 2021, the International Pharmaceutical Federation (FIP) launched a toolkit for pharmacists regarding medicines reconciliation [105]. In this document, aligned with international evidence, the FIP demonstrates the economic impact of RecM and supplies key elements to provide this service (templates, tools, and step-by-step process).
This service is patient-centred [106] and involves a multidisciplinary team. It is carried out mainly during the transition of care, such as admission, hospital discharge, and after transfers between health care institutions, thus differing from the medication review service [102]. Medication reconciliation services may prevent 75–80% of clinically relevant medication variances in patient care [104].
Pharmacists may play a significant role in RecM. Their technical and scientific skills ensure that an up-to-date therapeutic regimen is maintained for each patient, enabling the detection of discrepancies; the reduction in possible medication errors, such as omissions or duplications of therapy; and the detection of problems when transitions of care occur. The pharmacist should promote information sharing regarding the medication and its discrepancies with other health professionals who follow the older adult so that they can correct them together [107]. A systematic review [104] concluded that pharmacy-led medication reconciliation reduced by 68% the proportion of patients with at least one discrepancy and by 88% the number of medication discrepancies.
Portugal has taken some steps toward implementing medication reconciliation, mainly in medical institutions such as hospital settings [108]. According to Oliveira et al. [109], pharmacist-led medication reconciliation in a psychiatric hospital in Portugal reported that one in three discrepancies required further clarifications and that 80% of them were unintentional. Another study by Costa e Silva et al. [110] in a Portuguese Internal Medicine Department reported that 95.7% of the discrepancies were unintentional and that almost half of them (49.1%) were not documented. Yet, as with most EU countries, this service is implemented with unclear and heterogeneous rules [110]. Several obstacles to the successful implementation of RecM have been identified. For this service to be successful, it is essential to increase the presence of pharmacists in multidisciplinary teams. An effective IT system that allows healthcare professionals to record information during the various phases of patient care transition and a proper articulation between the hospital and health centres, as well as between the hospital and community pharmacies, isalso needed [106]. It is also necessary to increase the health literacy of patients (the centre of this intervention), their caregivers, and the institutions that receive the older adult after hospital discharge [107]. To achieve better outcomes, it is also essential to promote clinical training amongst pharmacists [82] and further comprehensive research.
2.1.4. Dose Administration Aids (DAAs)
Dose administration aids are personalised medication devices that organise oral solid dosage forms according to the prescribed dose and schedule [111]. Tablets and capsules are repacked into individually sealed compartments according to how they must be taken [112]. These devices help simplify medication management and improve adherence in polymedicated patients suffering from chronic diseases [112,113]. DAAs can help reduce medication-related hospitalisations and, consequently, the costs associated with drug-related problems [114]. There are many dose administration aid devices, and the pharmacist has to choose which one is appropriate for the patient’s therapeutic regimen, using their expertise and considering the patient’s needs. With this in mind, the pharmacist should perform a medication review before implementing a DAA [112].
Despite the above-mentioned advantages, there are few studies concerning the effectiveness of DAAs in therapeutical adherence [115] and their costs compared to not using this service over extended periods. In addition, not all medicines are stable enough to be included in these devices, whereas in others, this information is not clear in product labelling. Therefore, the pharmacist should evaluate the stability of each dosage form (which medicines and how long they can be stored in the DAA) [112] to ensure optimal patient care.
In Portugal, DAAs are regulated through Ordinance No. 455-A/2010 of 30 June [116], and pharmacists must follow the General Standard for Dose Administration Aids [117]. This document contains the safety rules that must be followed and the selection criteria that must be observed when implementing this service, such as flowcharts of DAA implementation and warnings regarding all steps of the process. A study among Portuguese pharmacies [115] analysed DAA characteristics, preferences, and impact on patients’ life. It concluded that most patients indicated fewer drug-related problems associated with forgetfulness and incorrect drug use, contributing to greater therapeutic adherence.
This area of pharmaceutical intervention contributes to the promotion of the correct, effective, and safe use of medicines in older adults, facilitates adherence to therapy, and minimises medication errors, thus improving older adults’ quality of life.
Figure 1 summarises possible/desired pharmacist interventions in older adult medication management.
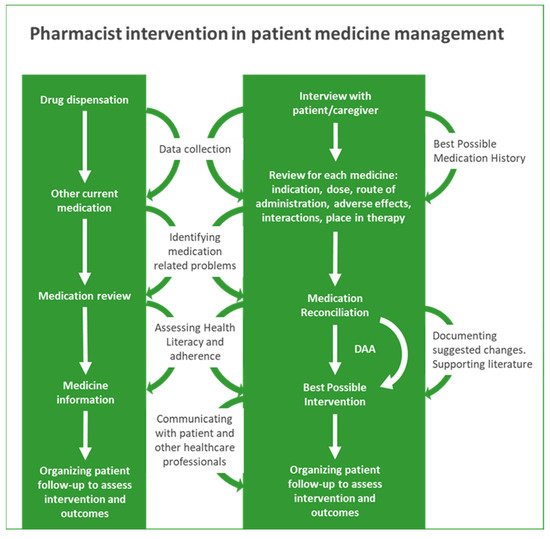
Figure 1. Pharmacist intervention in patient medication management.
This entry is adapted from the peer-reviewed paper 10.3390/healthcare10101833
This entry is offline, you can click here to edit this entry!
