Antibiotic misuse, sometimes called antibiotic abuse or antibiotic overuse, refers to the misuse or overuse of antibiotics, with potentially serious effects on health. It is a contributing factor to the development of antibiotic resistance, including the creation of multidrug-resistant bacteria, informally called "super bugs": relatively harmless bacteria (such as staphylococcus, enterococcus and acinetobacter) can develop resistance to multiple antibiotics and cause life-threatening infections.
- multiple antibiotics
- health
- antibiotic abuse
1. History of Antibiotic Regulation
Antibiotics have been around since 1928 when penicillin was discovered by Alexander Fleming. In the 1980s, antibiotics that were determined medically important for treatment of animals could be approved under veterinary oversight. In 1996, the National Antimicrobial Resistance Monitoring System (NARMS) was established.[1] Starting in 2010, publications regarding antimicrobial drugs in food become an annual report. Starting in 2012, there was publicly solicited input on how data is to be collected and reported for matters relating to the use of antimicrobials for food-producing animals. Resulting from this, the FDA revised its sampling structure within NARMS with the goal of obtaining more representative livestock data for the key organisms under surveillance.[1] “NARMS partners at CDC and USDA have published over 150 peer-reviewed research articles examining the nature and magnitude of antimicrobial resistance hazards associated with antibiotic use in food-producing animals.” In 2014, the FDA began working with the United States Department of Agriculture (USDA) and the Centers of Disease Control and Prevention (CDC) to explore additional mechanisms to obtain data that is representative of antibiotic use in food-producing animals. In 2015, the FDA issues the Veterinary Feed Directive (VFD) final rule. Under this rule veterinarians must authorize the use of antimicrobials within feed for the animals they serve.[1]
2. Instances of Antibiotic Misuse
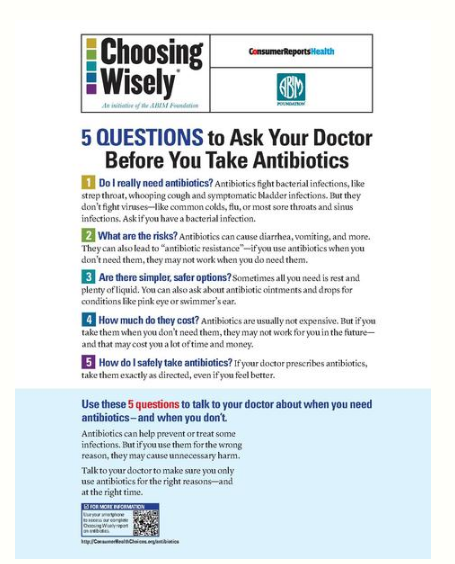
Common situations in which antibiotics are overused include the following:
- Apparent viral respiratory illness in children should not be treated with antibiotics. If there is a diagnosis of bacterial infection, then antibiotics may be used.[2]
- When children with ear tubes get ear infections, they should have antibiotic eardrops put into their ears to go to the infection rather than having oral antibiotics which are more likely to have unwanted side effects.[3]
- Swimmer's ear should be treated with antibiotic eardrops, not oral antibiotics.[4]
- Sinusitis should not be treated with antibiotics because it is usually caused by a virus, and even when it is caused by a bacteria, antibiotics are not indicated except in atypical circumstances as it usually resolves without treatment.[5]
- Viral conjunctivitis should not be treated with antibiotics. Antibiotics should only be used with confirmation that a patient has bacterial conjunctivitis.[6]
- Older persons often have bacteria in their urine which is detected in routine urine tests, but unless the person has the symptoms of a urinary tract infection, antibiotics should not be used in response.[7]
- Eczema should not be treated with oral antibiotics. Dry skin can be treated with lotions or other symptom treatments.[8]
- The use of topical antibiotics to treat surgical wounds does not reduce infection rates in comparison with non-antibiotic ointment or no ointment at all.[8]
3. Social and Economic Impact
Antibiotics can cause severe reactions and add significantly to the cost of care.[9] In the United States, antibiotics and anti-infectives are the leading cause of adverse effect from drugs. In a study of 32 States in 2011, antibiotics and anti-infectives accounted for nearly 24 percent of ADEs that were present on admission, and 28 percent of those that occurred during a hospital stay.[10]
If antimicrobial resistance continues to increase from current levels, it is estimated that by 2050 ten million people would die every year due to lack of available treatment and the world’s GDP would be 2 - 3.5% lower in 2050.[11] If worldwide action is not taken to combat antibiotic misuse and the development of antimicrobial resistance, from 2014 - 2050 it is estimated that 300 million people could die prematurely due to drug resistance and $60 – 100 trillion of economic output would be lost.[11] If the current worldwide development of antimicrobial resistance is delayed by just 10 years, $65 trillion of the world’s GDP output can be saved from 2014-2050.[11]
Prescribing by an infectious disease specialist compared with prescribing by a non-infectious disease specialist decreases antibiotic consumption and reduces costs.[12]
4. Antibiotic Resistance
Though antibiotics are required to treat severe bacterial infections, misuse has contributed to a rise in bacterial resistance. The overuse of fluoroquinolone and other antibiotics fuels antibiotic resistance in bacteria, which can inhibit the treatment of antibiotic-resistant infections.[13][14][15] Their excessive use in children with otitis media has given rise to a breed of bacteria resistant to antibiotics entirely.[16] Additionally, the use of antimicrobial substances in building materials and personal care products has contributed to a higher percentage of antibiotic resistant bacteria in the indoor environment, where humans spend a large majority of their lives.[17]
Widespread use of fluoroquinolones as a first-line antibiotic has led to decreased antibiotic sensitivity, with negative implications for serious bacterial infections such as those associated with cystic fibrosis, where quinolones are among the few viable antibiotics.[18][19][20]
5. Inappropriate Use

Antibiotics have no effect on viral infections such as the common cold. They are also ineffective against sore throats, which are usually viral and self-resolving.[21] Most cases of bronchitis (90–95%) are viral as well, passing after a few weeks—the use of antibiotics against bronchitis is superfluous and can put the patient at risk of suffering adverse reactions.[22]
Official guidelines by the American Heart Association for dental antibiotic prophylaxis call for the administration of antibiotics to prevent infective endocarditis. Though the current (2007) guidelines dictate more restricted antibiotic use, many dentists[23] and dental patients[24] follow the 1997 guidelines instead, leading to overuse of antibiotics.[25]
A study by Imperial College London in February 2017 found that of 20 online websites, 9 would provide antibiotics (illegally) without a prescription to UK residents.[26]
5.1. Antibiotics in Livestock
There has been massive use of antibiotics in animal husbandry. The most abundant use of antimicrobials worldwide is in livestock; they are typically distributed in animal feed or water for purposes such as disease prevention and growth promotion.[27] Debates have arisen surrounding the extent of the impact of these antibiotics, particularly antimicrobial growth promoters, on human antibiotic resistance. Although some sources assert that there remains a lack of knowledge on which antibiotic use generates the most risk to humans,[28] policies and regulations have been placed to limit any harmful effects, such as the potential of bacteria developing antibiotic resistance within livestock, and that bacteria transferring resistance genes to human pathogens [29] On January 1, 2017, the FDA enacted legislation to require that all human medically important feed-grade antibiotics (many prior over-the-counter-drugs) become classified as Veterinary Feed Directive drugs (VFD). This action requires that farmers establish and work with veterinaries to receive a written VFD order.[30] The effect of this act places a requirement on an established veterinarian-client-patient relationship (VCPR). Through this relationship, farmers will receive an increased education in the form of advice and guidance from their veterinarian.
The content is sourced from: https://handwiki.org/wiki/Chemistry:Antibiotic_misuse
References
- Food Insight (2016). FDA Antibiotic Regulation Through the Decades. http://www.foodinsight.org/fda-antibiotics-regulations-fact-sheet.
- American Academy of Pediatrics, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Pediatrics), http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-pediatrics/, retrieved 1 August 2013 , which cites American Academy of Pediatrics Subcommittee on Diagnosis and Management of Bronchiolitis (2006). "Diagnosis and Management of Bronchiolitis". Pediatrics 118 (4): 1774–1793. doi:10.1542/peds.2006-2223. PMID 17015575. Shulman, S. T.; Bisno, A. L.; Clegg, H. W.; Gerber, M. A.; Kaplan, E. L.; Lee, G.; Martin, J. M.; Van Beneden, C. (2012). "Clinical Practice Guideline for the Diagnosis and Management of Group a Streptococcal Pharyngitis: 2012 Update by the Infectious Diseases Society of America". Clinical Infectious Diseases 55 (10): e86–102. doi:10.1093/cid/cis629. PMID 22965026.
- American Academy of Otolaryngology–Head and Neck Surgery, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Otolaryngology–Head and Neck Surgery), http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-otolaryngology-head-and-neck-surgery-foundation//, retrieved 1 August 2013 , which cites Rosenfeld, R. M.; Schwartz, S. R.; Pynnonen, M. A.; Tunkel, D. E.; Hussey, H. M.; Fichera, J. S.; Grimes, A. M.; Hackell, J. M. et al. (2013). "Clinical Practice Guideline: Tympanostomy Tubes in Children". Otolaryngology–Head and Neck Surgery 149 (1 Suppl): S1–S35. doi:10.1177/0194599813487302. ISSN 0194-5998. PMID 23818543.
- American Academy of Otolaryngology–Head and Neck Surgery (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Otolaryngology–Head and Neck Surgery), http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-otolaryngology-head-and-neck-surgery-foundation/, retrieved 1 August 2013 , which cites Rosenfeld, R.; Brown, L.; Cannon, C.; Dolor, R.; Ganiats, T.; Hannley, M.; Kokemueller, P.; Marcy, S. et al. (2006). "Clinical practice guideline: Acute otitis externa". Otolaryngology–Head and Neck Surgery 134 (4): S4–23. doi:10.1016/j.otohns.2006.02.014. PMID 16638473.
- Consumer Reports; American Academy of Allergy, Asthma, and Immunology (July 2012), "Treating sinusitis: Don't rush to antibiotics", Choosing Wisely: an initiative of the ABIM Foundation (Consumer Reports), http://consumerhealthchoices.org/wp-content/uploads/2012/04/ChoosingWiselySinusitusAAAAI.pdf, retrieved 14 August 2012
- Sheikh, Aziz; Hurwitz, Brian; van Schayck, Constant Paul; McLean, Susannah; Nurmatov, Ulugbek (2012-09-12). "Antibiotics versus placebo for acute bacterial conjunctivitis". The Cochrane Database of Systematic Reviews 9: CD001211. doi:10.1002/14651858.CD001211.pub3. ISSN 1469-493X. PMID 22972049. https://dx.doi.org/10.1002%2F14651858.CD001211.pub3
- American Geriatrics Society, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Geriatrics Society), http://www.choosingwisely.org/doctor-patient-lists/american-geriatrics-society/, retrieved 1 August 2013
- American Academy of Dermatology (February 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American Academy of Dermatology), http://www.choosingwisely.org/doctor-patient-lists/american-academy-of-dermatology/, retrieved 5 December 2013 , which cites Sheth, V. M.; Weitzul, S. (2008). "Postoperative topical antimicrobial use". Dermatitis : contact, atopic, occupational, drug 19 (4): 181–189. PMID 18674453.
- "Economic aspects of antibacterial adverse effects". PharmacoEconomics 13 (1 Pt 1): 35–49. January 1998. doi:10.2165/00019053-199813010-00004. PMID 10175984. https://dx.doi.org/10.2165%2F00019053-199813010-00004
- Weiss AJ, Elixhauser A. Origin of Adverse Drug Events in U.S. Hospitals, 2011. HCUP Statistical Brief #158. Agency for Healthcare Research and Quality, Rockville, MD. July 2013. [1]
- "Antimicrobial Resistance: Tackling a crisis for the health and wealth of nations". https://amr-review.org/sites/default/files/AMR%20Review%20Paper%20-%20Tackling%20a%20crisis%20for%20the%20health%20and%20wealth%20of%20nations_1.pdf.
- Beović B., Kreft, Seme K., Čižman M. (2009). "The Impact of Total Control of Antibiotic Prescribing by Infectious Disease Specialist on Antibiotic Consumption and Cost". Journal of Chemotherapy 21 (1): 46–51. doi:10.1179/joc.2009.21.1.46. http://www.tandfonline.com/doi/abs/10.1179/joc.2009.21.1.46.
- "Antibiotic resistance among gram-negative bacilli in US intensive care units: implications for fluoroquinolone use". JAMA 289 (7): 885–8. February 2003. doi:10.1001/jama.289.7.885. PMID 12588273. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=12588273.
- "Studies examine prescribing of antibiotics for respiratory infections in hospital emergency departments". USA: U.S. Department of Health and Human Services. Archived from the original on 7 May 2009. https://web.archive.org/web/20090507021140/http://www.ahrq.gov/research/nov07/1107RA29.htm. "From 1995 to 2002, inappropriate antibiotic prescribing for acute respiratory infections, which are usually caused by viruses and thus are not responsive to antibiotics, declined from 61% to 49%. However, the use of broad-spectrum antibiotics such as the fluoroquinolones, jumped from 41% to 77% from 1995 to 2001. Overuse of these antibiotics will eventually render them useless for treating antibiotic-resistant infections, for which broad-spectrum antibiotics are supposed to be reserved."
- "Fluoroquinolone Resistance and Tuberculosis Treatment". USA: The New York City Department of Health and Mental Hygiene. http://www.nyc.gov/html/doh/html/tb/tb4a.shtml.
- Froom J; Culpepper L; Jacobs M et al. (July 1997). "Antimicrobials for acute otitis media? A review from the International Primary Care Network". BMJ 315 (7100): 98–102. doi:10.1136/bmj.315.7100.98. PMID 9240050. PMC 2127061. http://bmj.com/cgi/pmidlookup?view=long&pmid=9240050.
- Hartmann, Erica; Hickey, Roxana; Hsu, Tiffany; Roman, Clarisse; Chen, Jing; Schwager, Randall; Kline, Jeff; Brown, G. et al. (September 20, 2016). "Antimicrobial Chemicals Are Associated with Elevated Antibiotic Resistance Genes in the Indoor Dust Microbiome". Environmental Science & Technology: 9807–9815. doi:10.1021/acs.est.6b00262. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=5032049
- "Cipro, Related Antibiotics Over-Prescribed, Fueling Microbe Resistance". USA: University Of California. 1 October 2002. http://www.universityofcalifornia.edu/news/article/4786. Retrieved 13 August 2009.
- K. Bassett; B. Mintzes; V. Musini; T.L. Perry Jr; M. Wong; J.M. Wright (November 2002). "Therapeutics Letter" (PDF). Canadian Family Physician 48. http://www.cfpc.ca/cfp/2002/Nov/_pdf/vol48-nov-critical-2.pdf. "Gatifloxacin and moxifloxacin have no proven clinical advantages over other fluoroquinolones, macrolides, or amoxicillin. Based on cost, they are not first-choice drugs for their approved indications.".
- Ziganshina, Lilia E.; Titarenko, Albina F.; Davies, Geraint R. (2013-06-06). "Fluoroquinolones for treating tuberculosis (presumed drug-sensitive)". The Cochrane Database of Systematic Reviews (6): CD004795. doi:10.1002/14651858.CD004795.pub4. ISSN 1469-493X. PMID 23744519. https://dx.doi.org/10.1002%2F14651858.CD004795.pub4
- "Reattendance and complications in a randomised trial of prescribing strategies for sore throat: the medicalising effect of prescribing antibiotics". BMJ 315 (7104): 350–2. August 1997. doi:10.1136/bmj.315.7104.350. PMID 9270458. PMC 2127265. http://bmj.com/cgi/pmidlookup?view=long&pmid=9270458.
- Hueston WJ (March 1997). "Antibiotics: neither cost effective nor 'cough' effective". The Journal of Family Practice 44 (3): 261–5. PMID 9071245. http://www.ncbi.nlm.nih.gov/pubmed/9071245
- Zadik Y; Findler M; Livne S et al. (December 2008). "Dentists' knowledge and implementation of the 2007 American Heart Association guidelines for the prevention of infective endocarditis". Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106 (6): e16–9. doi:10.1016/j.tripleo.2008.08.009. PMID 19000604. http://www.ooooe.net/article/S1079-2104(08)00597-0/abstract.
- "Survey of acceptance of the 2007 American Heart Association guidelines for the prevention of infective endocarditis: a pilot study". Quintessence Int 42 (3): 243–51. March 2011. PMID 21465012. http://www.quintpub.com/journals/qi/abstract.php?iss2_id=919&article_id=10528&article=9&.
- Wilson W; Taubert KA; Gewitz M et al. (October 2007). "Prevention of infective endocarditis: guidelines from the American Heart Association". Circulation 116 (15): 1736–54. doi:10.1161/CIRCULATIONAHA.106.183095. PMID 17446442. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=17446442.
- "No prescription needed to obtain antibiotics from almost half of online sites, study shows". Pharmaceutical Journal. 17 February 2017. http://www.pharmaceutical-journal.com/20202356.article. Retrieved 19 March 2017.
- Silbergeld, E.K.; Graham, J.; Price, L.B. (2008), "Industrial food animal production, antimicrobial resistance, and human health", Annual Review of Public Health 29: 151–169, doi:10.1146/annurev.publhealth.29.020907.090904, PMID 18348709 https://dx.doi.org/10.1146%2Fannurev.publhealth.29.020907.090904
- Landers, T.F.; Cohen, B.; Wittum, T.E.; Larson, E.L. (2012), "A review of antibiotic use in food animals: Perspective, policy, and potential", Public Health Reports 127 (1): 4–22, PMID 22298919 http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=3234384
- http://www.sciencemag.org/news/2017/09/are-antibiotics-turning-livestock-superbug-factories
- Beth Ferry, Madonna Benjamin, Michigan State University Extension and Megan Sprague, MDARD (2016). Don’t wait, be ready! New antibiotic rules for 2017. http://msue.anr.msu.edu/news/dont_wait_be_ready_new_antibiotic_rules_for_2017.
