These hydrogels are fluid-like at room temperature and quickly gelate at body temperature to promote the sustained release of encapsulated drugs, increasing drug contact time with the RWM [
]. Hydrogels have numerous advantages, including increased biocompatibility, adjustable biodegradability, low toxicity, and good swelling behavior [
]. The degree of swelling is a critical parameter, with a higher concentration of polymers leading to greater swelling and slower drug release [
]. In the middle ear, hydrogels are typically injected near the RWM and RWM niche. This enables prolonged diffusion of the released drug across the RWM at appropriate therapeutic concentrations [
]. Hydrogels have been developed in several formulations for inner ear drug delivery, including polymers such as chitosan or PEG-based hydrogel, Poloxamer 407, and hyaluronic acid [
]. Injectable PEG-based hydrogel has been shown to be an effective and safe method for inner ear delivery. In guinea pigs, the dexamethasone concentrations in perilymph were maintained for at least 10 days for the PEG hydrogel as compared to the control sample of free dexamethasone [
]. Hyaluronic acid, when applied to the RWM of guinea pigs prior to delivering an adenovirus, provides an atraumatic and feasible method of delivering transgene into the inner ear [
].
Poloxamer 407, also known as Pluronic
® F-127, is the primary polymer for formulating hydrogels used for inner ear delivery of therapeutics [
59]. Poloxamer 407 is an amphiphilic, non-ionic triblock copolymer consisting of a residue of polyoxypropylene (POP) between two units of polyoxyethylene (POE). It is a widely used thermo-sensitive hydrogel due to its non-irritating action on biological membranes and can remain as a gel for several weeks to months [
71]. Its thermo-sensitivity is due to the hydrophobic interactions between the copolymer chains of Poloxamer 407. As temperature increases, copolymer chains of Poloxamer 407 aggregate to form a micellar structure due to the dehydration of hydrophobic poly(propylene oxide) units [
72] with a micelle diameter in the 20–100 nm range. The hydrophobic core is the drug loading site, creating space for the encapsulation of drugs through chemical interactions. The properties of the inner and outer shell determine the rate of drug release. Different methods are employed for encapsulating drugs in Poloxamer 407, such as direct dissolution, evaporation, and freeze-drying [
73]. The gelation of Poloxamer 407 is reversible once gelling conditions, such as temperature, pH, or chemical, are removed [
62].
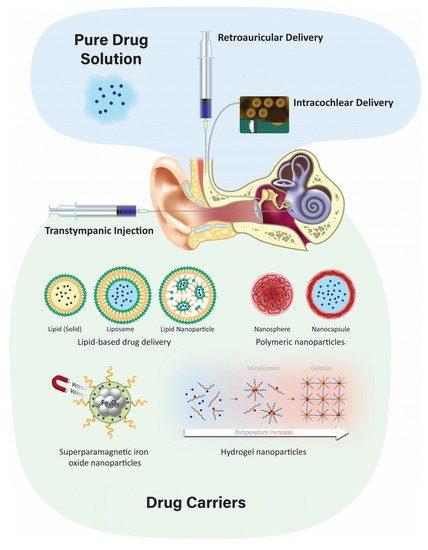
4.3. Nanoparticulate Injection Systems
Nanoparticulate drug delivery is one of the most advanced technologies in drug design due to its advantages such as surface modification, improved drug solubility, stability, and bioavailability, as well as sustained controlled drug release at the target site. Injecting nanoparticulates at the targeted site leads to lower systemic toxicity, fewer side effects, improved kinetics of the drug, and extended drug bioavailability [77]. There are two primary nanoparticulate strategies: passive and self-delivery. In passive delivery, drugs are encapsulated in nanocarriers and are slowly released from the carriers. In self-delivery, drugs are conjugated to the carrier for easy delivery, and the drug dissociates from the carrier quickly at the presumptive targeted site, e.g., in the vicinity of tumors [78,79]. A large variety of nanoparticles have emerged, including polymeric, liposomes, and lipid-based structures, among others.
4.3.1. Polymeric Nanoparticles
Biodegradable polymeric microparticles or nanoparticles have been developed for a wide range of therapeutic applications and as inner ear drug delivery systems. They are often based on poly (lactic) co-glycolic acid (PLGA) or chitosan [
6] and have advantages over other delivery systems due to their biocompatibility, biodegradability, small size, long shelf life, stability during storage, and highly reproducible formulation methods [
59]. Nanoparticles have a diameter of <1 µm and are usually formulated with diameters of 100–300 nm, and for inner ear delivery, ~200 nm or less [
4]. Polymeric nanoparticles can also incorporate visualization agents such as fluorescent dyes and MRI contrast agents [
100]. Iron oxide nanoparticles have been extensively studied as a contrast agent for MRI. It has a magnetic core and different ligands focus on targeting specific sites or cells. PLGA is one of the more popular polymeric particles that can encapsulate both hydrophobic and hydrophilic drugs for intratympanic delivery and can be transported across the RWM into perilymph via the transcellular pathway [
101].
4.3.2. Solid Lipid Nanoparticles
Solid lipid nanoparticles (SLNs) are a novel class of stable nanoparticles that are particularly suitable for the encapsulation of hydrophobic drugs such as curcumin, resveratrol, or quercetin [
102]. They can also act as a carrier for hydrophilic drugs when formulated without the use of organic solvents [
103]. SLNs are composed of a hydrophobic triglyceride core with an amphiphilic surfactant shell [
104]. SLNs are biodegradable, biocompatible, and are non-ototoxic over a wide dose range. Low doses of hydrocortisone encapsulated in SLNs increase their protective effect and prolong the survival of auditory cells treated with cisplatin in vitro [
97]. In vivo application of SLNs has shown no interference in hearing threshold or loss of hair cells [
105].
4.3.3. Liposomes
Liposomes are composed of two layers of amphipathic molecules with a hydrophilic external layer and an internal surface composed of a phospholipid bilayer [
106]. A key advantage of using liposomes for cochlear drug delivery is their ability to control drug release [
96]. In an in vivo study, the microinjection of cationic liposome-mediated gene transfer into guinea pig cochleas revealed that transgene expression was steady for up to 14 days in the neurosensory epithelia and surrounding tissues without any toxicity [
107]. Others have successfully demonstrated cell–gene delivery of therapeutic agents to the inner ear using a liposome-mediated delivery method [
108].
4.3.4. Superparamagnetic Iron Oxide Nanoparticles (SPION)
SPIONs are Fe
3O
4 particles that can be magnetically controlled to focus on the migration of particles into the inner ear after crossing the RWM [
60]. These particles are encapsulated in a polymeric layer of PLGA [
109] or chitosan [
110] to contain the therapeutic agent. Other polymers such as polyacrylic acid and polyvinylpyrrolidone are used to form a coat around iron oxide nanoparticles to increase stability and improve their magnetic properties [
111]. This technique has been demonstrated in vivo in rat and guinea pig models, as well as in vitro in cell lines and the human temporal bone. Biocompatibility and safety have been demonstrated by various methods, including hair cell survival in organotypic cell cultures [
112].
4.4. Advantages and Disadvantages of the Nanoparticulate Injection System
Nanoparticles are created from a variety of materials with a diameter range of 10 to several 100 nanometers, and customized to encapsulate various therapeutic agents [
113]. Nanoparticles are widely used for non-invasive application, sustained, or controlled release of drugs, drug stabilization, and surface modification for targeting specific organs [
114]. Various studies that administered nanoparticles onto the RWM have shown successful delivery of biomaterials into the inner ear [
115]. Nanoparticles can enter the perilymph and the endolymph [
106] following intratympanic administration and can be targeted to a specific intracochlear site of interest. Nanoparticles, when combined with hydrogel, improve the bioavailability of the drug at the targeted site and prevent rapid drug release [
106]. Nanoparticles can also be conjugated to peptides that can penetrate cells, or their surface can be modified to increase their contact with RWM [
116]. Challenges for nanoparticle delivery into the inner ear include limited access to the inner ear and poor uptake of drugs by inner ear cells [
106].
4.5. Positively-Charged Biomaterials for Local Drug Delivery
The charge of nanoparticles can determine their uptake by inner ear hair cells and their penetration of epithelial membranes. Phospholipid-based nanoparticles with a positive charge of +26 mV were taken up by sensory hair cells at a two-fold higher rate than nanoparticles with a neutral or negative charge. This is likely due to the interaction between positively-charged nanoparticles and negatively-charged lipid plasma membranes [
119]. The addition of cationic polyethylene glycol (PEG) to phospholipid-based nanoparticles increases their trafficking across the RWM but has enhanced cytotoxicity [
120]. Nanoparticulates containing cationic-PEG to deliver dexamethasone to the RWM in mice provide an anti-inflammatory effect during combined kanamycin and furosemide treatment and higher cellular uptake within the organ of Corti [
99]. Positively-charged chitosan nanoparticles enter the inner ear at a faster rate [
59]. Positively-charged chitosan nanoparticles containing D-glucosamine and N-acetyl-D-glucosamine facilitate penetration of lipid cell membranes in the inner ear [
119]. Other positively-charged nanoparticles, such as 1,2-dioleoyl-3-trimethylammonium-propane (DOTAP), are distributed widely in the inner ear after RWM application [
14]. In rodents, positively-charged ferritin readily passes through RWM, while negatively-charged ferritin does not [
13].
4.6. Negatively-Charged Biomaterials for Local Drug Delivery
Negatively charged polymers have been frequently used for the preparation of nanoparticles due to their biocompatible properties. PLGA, an anionic polymer, is one of the most successful biodegradable systems for inner ear drug delivery [
128]. PLGA with penetration enhancers, such as cell-penetrating peptides, has been used to investigate their impact on cochlear drug delivery in vivo [
129]. PLGA nanoparticles coated with Poloxamer-407, with a zeta-potential of −15.90 mV, had a 1.6-fold higher distribution in the cochlea as compared to anionic PLGA nanoparticles coated with chitosan [
128]. Negatively charged nanoparticles, with a surface charge of −22.1 mV, were administered intratympanically, diffused across the RWM, and distributed in the basal and middle cochlear turns when visualized by transmission electron microscopy [
130]. Negatively-charged gelatin hydrogels composed of highly biocompatible polymers are used for controlled drug release, such as insulin-like growth factor 1 to the inner ear after noise-induced hearing loss in guinea pigs, resulting in increased outer hair cell survival [
131]. Zeolitic imidazole nanoparticles have great potential to deliver drugs, proteins, and RNA to the inner ear for the treatment of noise-induced hearing loss. These nanoparticles are anionic carriers with superior cell viability and biocompatibility [
132].
5. Conclusions
Local delivery has the advantage of maximizing targeted effects in the inner ear while minimizing systemic toxicity. Intratympanic injections are a relatively minimally invasive procedure. Future research to enhance permeation through the RWM and methods to increase the release duration of therapeutic agents from biomaterials may provide higher and more sustained concentrations of the drug in the cochlea following intratympanic administration. The use of nanoparticles encapsulating therapeutic agents that can target the sensory hair cells in the inner ear is innovative and exciting.
Currently, there are no FDA-approved drugs or licensed therapies on the market for hearing loss due to ototoxicity. As the field of inner ear therapeutics evolves, drug delivery strategies must recognize the relationships between therapeutic agents, formulations, delivery systems, and the disease. Treatment options for hearing loss will undeniably be further refined and optimized in the coming years as new therapeutics become available. Future research is needed to identify new mechanisms of action and delivery that will enable exciting novel treatments for inner ear disorders.