Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Genetics & Heredity
The basic composition of the mitogen-activated protein kinase (MAPK) pathway is divided into three modules in sequence, with a cascade effect: MAPK kinase kinase (MAPKKK), MAPK kinase (MAPKK), and MAPK. The MAPK signaling pathway is activated in over 50% of human oral cancer cases.
- oral squamous cell carcinoma
- MAPK
- signaling pathway
- immunotherapy
1. Activation of MAPK Signaling Pathway
MAPK activation requires double phosphorylation on the Thr-X-Tyr (X representing any amino acid) motif catalyzed by MAP2K. Upon activation, MAPK phosphorylates specific serine and threonine residues on target substrates, including other protein kinases and many transcription factors. Common and bispecific phosphatases inactivate MAPKs and are regulated by scaffold proteins [12]. Figure 1 demonstrates the cascade activation of the MAPK signaling pathway.
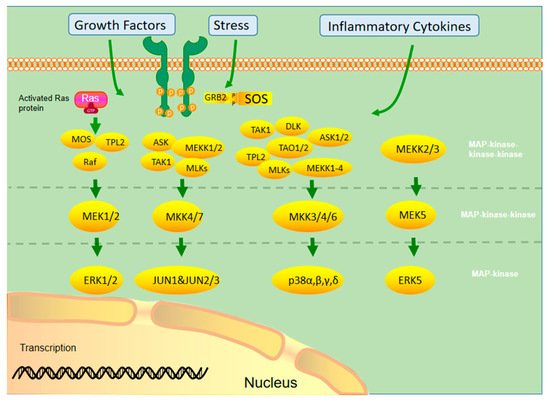
Figure 1. Different MAPKs associate with specific MAPK kinase (MAPKK) and MAPK kinase kinase (MAPKKK) to form a conserved three-stage enzymatic cascade (MAPKKK→MAPKK→MAPK), through which upstream signals are transmitted from MAPK to downstream nuclear transcription factors and cytoskeletal proteins to form a complete MAPK signaling pathway, which finally completes the regulation of cellular physiological activities.
Currently, the ERK1/2 pathway is the most widely studied pathway in the MAPK family. It involves extracellular growth factors, such as the epidermal growth factor (EGF), and activated tyrosine kinase receptors, such as the EGF receptor (EGFR), providing a binding site for the adaptor protein growth factor receptor-bound protein 2 and recruiting the SOS protein into the cell membrane. SOS activates Ras by consuming GTP to form Ras GTP. After Ras activation, it can affect many downstream proteins, including AF6, phosphatidylinositol-3-kinase (PI3K), phospholipase C, and Raf. Among them, Ras GTP recruits the Raf protein into the plasma membrane and phosphorylates it using other kinases (protein kinase A, p21-activated kinase, Src) to activate its kinase function. The Raf protein family includes B-Raf, A-Raf, and C-Raf (Raf1). B-Raf plays an important role in the development and progression of malignant tumors. The activated Raf kinase binds to the downstream MEK 1/2 and activates ERK1/2. Activated ERK1/2 can continue to phosphorylate transcription factors, such as ELK1, ETS, FOS, Jun, myc, and Sp1, and induce gene expression related to cell cycle and cell proliferation. In addition, activated ERK1/2 can phosphorylate various intracellular kinases, such as Raks, msks, and mnks, which affect cell proliferation and adhesion [13,14,15].
The JNK/MAPK signaling pathway can activate cytokines (tumor necrosis factor-alpha [TNF-α], interleukin [IL]-1), EGF, and some G protein-coupled receptors by generating stress through, for example, ultraviolet light, heat shock, hyperosmotic stimuli, and protein synthesis inhibitors. The stress response signal is transmitted to MAPKKK through the Rho subfamily (Rac, rho, Cdc42), a member of the small molecule G protein Ras superfamily, which in turn activates mek4/7 and JNK. JNK phosphorylation can act on various downstream transcription factors (e.g., Jun, ELK1, Ets2, etc.) and kinases (mainly MNK) and produce various physiological processes that promote cell growth, differentiation, survival, and apoptosis [16].
The main inducing factors of the p38/MAPK pathway are hypoxia, ultraviolet radiation, osmotic shock, inflammation, and other stress reactions. P38 MAPK is mainly activated by ERK3/6 phosphorylation, which further promotes cell apoptosis and inhibits cell proliferation by inducing transcription factors and kinases. In addition, this pathway also promotes cell movement [17]. Ras plays an important role in activating the MAPK signal pathway. It is a key component of many cellular signal transduction pathways. Permanent activation of the Ras protein caused by mutation is prevalent in all human cancers. Therefore, Ras inhibitors are effective drugs to treat OSCC [18].
2. Mutation of the MAPK Signaling Pathway
As a signal medium in cells, MAPK controls cell differentiation, proliferation, apoptosis, and other effector functions under the stimulation of external pressure or ligands. The mutation rate of MAPK1 is higher in Asian populations, with an average of 0.79% among 32 cancer genomic profiles from The Cancer Genome Atlas (TCGA) database. The mutation rate of MAPK1 is relatively higher in HNSCC than in pan-cancer TCGA [19,20]. One-fifth of the patients with HNSCC are affected by MAPK pathway mutations, and abnormalities in the MAPK pathway are correlated with the survival time of patients [21]. Chan et al. analyzed the gene-chip technology and showed that MAPK in human HNSCC was overexpressed compared to matched non-cancerous tissues. The expression of several genes in MAPK signaling pathways, such as p38β, ERK2, and JNK2, increased two-folds, showing statistical significance. p38β, JNK2, and ERK2 showed a 5.27-, 2.57-, and 3.30-time increase, respectively [22]. An immunohistochemical analysis of 100s of HNSCC tissues showed elevated active phosphorylated p38 in 79% of the tissues, with increased phosphorylation activities of ERK1/2 and JNK in <33% and <16% of cases, respectively [21,23].
3. MAPK Signaling Pathway in OSCC
3.1. ERK/MAPK Signaling Pathway in OSCC
Activation of ERK1/2 is mostly associated with cell survival, while that of JNK or p38 is associated with the induction of apoptosis [24]. However, this classification is too simplistic, and the actual role of each MAPK cascade depends highly on the cell type and the situation [25]. Activation of MAPK, particularly ERK, is differentially regulated according to the stage of tumor differentiation. For instance, the phosphorylation level of ERK is lower in advanced poorly differentiated prostate cancer than in early prostate cancer [26]. Dickkopf-related protein 3 (Dkk3), as a member of the Dickkopf WNT signaling pathway inhibitor family, has a tumor suppressive effect [27,28]. For example, overexpression of Dkk3 messenger (mRNA) is related to a good prognosis of prostatic cancer [29]. It may induce cancer cell apoptosis by overexpressing through adenovirus-mediated gene transfer [30,31]. Dkk3 plays a carcinogenic role in OSCC. Its overexpression in OSCC cells would largely increase the malignancy of the cells in vitro and in vivo and regulate the malignant behavior of cancer cells through the PI3K/mammalian target of rapamycin (mTOR)/Akt and MAPK pathways. Thus, MAPK may have a tumor- or tissue-specific effects [32]. C-Myc can alter the biological behavior of tumors through the ERK/MAPK pathway. For example, Marconi et al. showed that KRAS mutations activate the Raf/MEK/ERK signaling pathway to upregulate c-Myc, causing overexpressions of Bcl-2, hypoxia-inducible factor (HIF)-1α, vascular endothelial growth factor (VEGF), MMP-9, and other proteins, affecting the invasive, hypoxic, angiogenic, migratory, and inflammatory processes in OSCC [33].
ERK1 and ERK2 are widely expressed in tissues and participate in regulating meiosis, mitosis, and post-mitotic function of differentiated cells. In the early 1980s, ERK1 was the first MAPK core molecule identified in mammals [34]. ERK activation causes phosphorylation and activation of various cytoplasmic substrates, such as cytoskeletal proteins and downstream protein kinases. In addition, phosphorylated ERK1/2 can be transported to the nucleus to activate various transcription factors, such as ELK-1, SP-1, and AP-1, thereby regulating the transcription of different genes [10]. The ERK1/2 signaling pathway mainly affects tumor cells by proliferating cell cycle regulation. Sustained ERK activation can induce cell cycle inhibition and pro-differentiation signals in epithelial origin cells [35]. G1/S conversion is the key regulatory point of the cell cycle. Sustained activation and nuclear localization of ERK1/2 may affect G1/S conversion by regulating cyclin D1 transcription [36,37]. Inhibiting the ERK/MAPK signaling pathway leads to the proliferation, invasion, and migration of OSCC cells, causing G0/G1 arrest and promoting apoptosis [38,39]. Wu et al. [40]. reported that downregulations of MAPK/ERK1/2 and PI3K/Akt signals and cyclin D1 and E expression levels can induce G0/G1 arrest and inhibit OSCC cell proliferation. ERK1/2 is closely associated with tumor invasion and migration, and phosphorylation of ERK/MAPK activates AP-1 and nuclear factor kappa B (NF-κB). They upregulated expressions of MMP2 and MMP9, which are extracellular membrane-degrading enzymes associated with tumor aggressiveness. MMP2 and MMP9 degrade type IV collagen, a major extracellular membrane component of the basement membrane, which may be critical for tumor invasion and metastatic potential, thereby degrading the extracellular matrix and allowing cells to cross the basement membrane, facilitating tumor cell metastasis [41,42]. Blocking ERK/MAPK activation inhibited cell migration and stem characteristics of the nhri-hn1 cell line in a mouse tongue cancer model [43]. Junhai et al. found that miR-145 could inactivate the ERK/MAPK signaling pathway by inhibiting Hoxa1, thereby inhibiting the proliferation, migration, and invasion of OSCC cells and inhibiting their growth in vivo [44]. The integrin (ITG) family of proteins plays important roles in OSCC αV invasion, migration, and apoptosis via ITG-β. They regulate the proliferation and invasion of OSCC cells through the MAPK/ERK signaling pathway [45,46,47]. Chloride intracellular channel 1 (CLIC1) silence reduces αv and β1. p-ERK, vimentin, MMP2, and MMP9 levels increased p-p38, E-cadherin, Caspase3, and caspase9 levels. CLIC1 interacted with ITG, thereby activating the MAPK signaling pathway, which regulates OSCC progression [48]. Different MAPK activation times may lead to different results, occasionally even contradictory ones. For example, transient activation of ERK may generate proliferative signals, but sustained phosphorylation may generate signals leading to cell differentiation [49].
3.2. JNK/MAPK Signaling Pathway in OSCC
JNKs were isolated and identified as stress-activated protein kinases, which activate the inhibitory response to protein synthesis [50]. The JNK protein is encoded by three genes, i.e., MAPK8 (JNK1), MAPK9 (JNK2), and MAPK10 (JNK3), and alternately spliced to produce ≥ 10 isomers. JNK1 and JNK2 are expressed in almost every cell, while JNK3 is mainly expressed in the brain [51]. The carcinogenic function of JNKs is related to their ability to phosphorylate Jun and activate AP1. In contrast, their antitumor effect may be related to the apoptotic activity [52]. In addition, JNK1 and JNK2 play different roles in cancer, promoting or inhibiting tumor formation [53].
Although some studies support the carcinogenic effect of JNK, others show that JNK plays a tumor-inhibitory role in HNSCC [63], which requires more studies to clarify its role in OSCC.
3.3. p38/MAPK Signaling Pathway in OSCC
P38 kinase was originally screened and defined in drugs that inhibit the TNF-mediated inflammatory response [64]. The p38-MAPK pathway and some physiological changes in cells, such as growth signal transmission, the ability of unlimited replication, and apoptosis, angiogenesis, invasion, or metastasis prevention, are involved in transformation [65]. P38 is a conserved serine–threonine protein kinase, which can be activated by various extracellular inflammatory factors (e.g., TNF-α, IL-1), bacterial lipopolysaccharide, lipopolysaccharide, chemokine, and ultraviolet light. Activated p38 MAPK regulates cell function by regulating expression activities of downstream enzymes and transcription factors [66]. p38 MAPK activation is necessary for normal immune processes and inflammatory responses. It promotes key regulators of pro-inflammatory cytokine biosynthesis through transcription and translation, and thus, the components of this pathway become potential therapeutic targets for autoimmune and inflammatory diseases [67]. Simultaneously, it participates in tumorigenesis and ischemia-reperfusion injury [66]. In OSCC, p38 signal inhibition can reduce the tumor proliferation rate and reduce inflammation caused by the tumor [68,69]. Angiogenesis plays a key role in tumor progression, providing nutrition and oxygen for tumors and eliminating metabolic waste and carbon dioxide. Continuous neovascularization promotes tumor growth and diffusion [65,70]. P38α can control the growth of cancer cells and tumor-induced angiogenesis and lymphangiogenesis. It is a positive regulator in the tumor microenvironment of OSCC [23]. Banerjee et al. found that glycophorin receptor 2 (GALR2) induces angiogenesis by secreting pro-angiogenic cytokines mediated by the p38/MAPK signaling pathway, vascular endothelial growth factor (VEGF), and IL-6. In addition, GALR2 activates the small GTP protein Rap1b, which induces the inactivation of p38-mediated tristetraprolin (TTP). TTP is an RNA-BP that downregulates angiogenic factors, such as IL-6, VEGF, and IL-8, produced by tumor and inflammatory cells [71,72,73]. Its function is to destroy the stable transcription of cytokines, increase the secretion of pro-angiogenic cytokines, and promote angiogenesis in vitro and in vivo. In OSCC cells with GALR2 overexpression, p38 inhibition activates TTP and reduces cytokine secretion. TTP inactivation increases IL-6 and VEGF secretions [24]. IL-6 is a biomarker with low disease-specific survival [74], and VEGF elevation is associated with reduced recurrence time [75]. In HNSCC cases with low differentiation, p38 activation is more obvious and associated with a poor prognosis. The P38/MAPK signaling pathway is related to apoptosis and autophagy. Treating cells with the p38 MAPK (SB203580) or JNK1/2 (sp600125) inhibitor can promote/weaken G2/M phase arrest, apoptosis, and autophagy of cancer cells, respectively [76].
3.4. MAPK Signaling Pathway and Immunity
Tumor cells downregulate immune cells in the tumor microenvironment to obtain tumor-promoting activity. MAPK is a central molecule of signal transduction regulating cell function. P38a MAPK participates in inflammation. It can produce proinflammatory cytokines [77], and acute inflammation can lead to cancer [78]. In the inflammatory microenvironment of OSCC, p38 αMAPK produces proinflammatory cytokines TNF-α, IL-1B, and IL-6, and plays a role in cancer progression [79]. Around MAPK-mutated HNSCC tumor cells, there exists a tumor microenvironment with high CD8+ T-cell inflammatory immunoreactivity, resulting in an increased endogenous lytic activity. These differences are evident in OSCC, suggesting that the ability of MAPK pathway mutation to predict disease in OSCC may be stronger than that of TMB. Pan pathway immune profiling studies revealed that MAPK-mutant tumors are the only “CD8+ T-cell inflammatory” tumors with an inherently hyperimmune responsive and structurally cytolytic tumor microenvironment. Immunoreactive MAPK-mutant models of HNSCC show massive in situ recruitment of cell-active or dead in situ CD8+ T cells. Consistent with the CD8+ T inflammatory phenotype, patients with MAPK-mutant OSCC had a 3.3–4.0-times longer survival time than patients with WT receiving anti-PD1/PD-L1 immunotherapy, independent of the tumor mutation burden. The pan-cancer prognosis of patients is consistent. MAPK mutations may recognize the high inflammatory/cytolytic activity of CD8+ T cells in patients with OSCC. p38 inhibitors have shown some success in treating and limiting adverse sequelae of inflammatory diseases and are a potential adjuvant therapy for OSCC [80].
IL-8 is closely related to the MAPK signaling pathway in OSCC. Leong et al. showed that it induces p-p38 MAPK and p-ERK expressions in HNSCC cells and downregulates p-JNK expression. It can increase NF-κB pathway expression in OSCC, suggesting that it may regulate MAPK and NF-κB pathways to regulate inflammatory response [22]. ROS or calcium ions activate p38MAPK, ERK [81], and JNK, which then affect the activation and transcriptional activity of hypoxia-inducible factor (HIF)-1. In addition, ERK leads to ser276p65/rela NF-κB phosphorylation of B, activating this transcription factor [82]. These processes lead to increased expression of some inflammatory genes and cell response to proinflammatory factors, particularly cyclooxygenase-2 [83], CC motif chemokine ligand 2/monocyte chemoattractant protein 1 (MCP-1) [84], CXC motif chemokine ligand (CXCL) 1/growth-related oncogene-α [85], CXCL8/IL-8 [86], and IL-6 [87]. They are inflammatory mediators involved in various tumor processes [88,89]. Figure 2 lists some well-studied key molecular pathways.
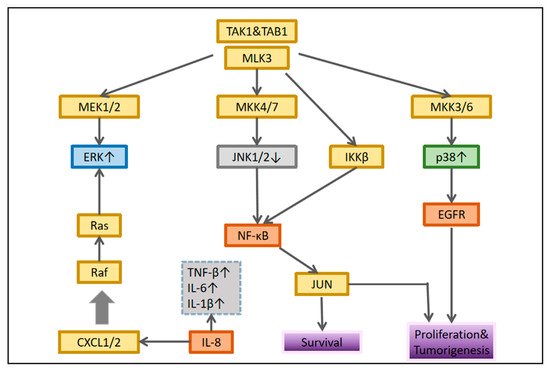
Figure 2. Interaction between MAPK and nuclear factor-κB signaling. In each cellular system, different connections are established that determine the biological response of the tumor.
4. MAPK Signaling Pathway in the EMT Process in OSCC
Overcoming intercellular adhesion and invading surrounding tissues is the main feature of the transformation from benign lesions to metastatic cancer. EMT is key to this transformation. It is molecularly characterized by loss of E-calmodulin and increased expression of mesenchymal markers, including, for example, n-calmodulin, snail, fibronectin, and wave proteins [90,91]. The loss of E-cadherin is closely related to a poor prognosis [92]. As a result, the discovery of potential EMT blockers in patients with OSCC may reveal directions for novel therapies. Snails can regulate transcriptional inhibition of epithelial marker E-cadherin during EMT [93]. MAPKP38 increased significantly in tumor cell lines with high snail expression. The P38 interacting protein (p38ip) is a human analogue of the yeast spt20 protein. It is a subunit of histone spt3-taf9-gcn5 acetyltransferase. P38 binds to and stabilizes p38ip, resulting in enhanced transcription. P38-p38ip is involved in snail-induced downregulation of E-cadherin and cell invasion in OSCC. The transcription inhibitor snail plays a direct role in the downregulation of E-cadherin, while the proinflammatory mediator upregulates snail, thus affecting the cycle of inflammation-promoting tumor progression [94]. Cui et al. [95]. found that protein kinase D3 regulates PD-L1 expression and EMT in OSCC through ERK1/2. In OSCC, transient knockout of ERK1/2 can cancel PD-1/PD-L1-induced EMT. Similarly, ERK1/2 activation is affected by PD-L1 knockdown. PD-L1 interacts with PD-1 expressed by activated T cells, B cells, natural killer cells, some dendritic cells, and tumor-associated macrophages, thereby activating the PD-1/PD-L1 pathway. In contrast, activation of this pathway can inhibit the anti-tumor function of the same immune cells, decreasing anti-tumor immunity [96,97].
This entry is adapted from the peer-reviewed paper 10.3390/cancers14194625
This entry is offline, you can click here to edit this entry!
