Obsessive–compulsive personality disorder (OCPD) is a cluster C personality disorder marked by an excessive need for orderliness, neatness, and perfectionism. Symptoms are usually present by the time a person reaches adulthood, and are visible in a variety of situations. The cause of OCPD is thought to involve a combination of genetic and environmental factors, namely problems with attachment. This is a distinct disorder from obsessive–compulsive disorder (OCD), and the relation between the two is contentious. Some studies have found high comorbidity rates between the two disorders but others have shown little comorbidity. Both disorders may share outside similarities—rigid and ritual-like behaviors, for example. Attitudes toward these behaviors differ between people affected with either of the disorders: for people with OCD, these behaviors are egodystonic, unwanted and involuntary, being the product of anxiety-inducing and involuntary thoughts. On the other hand, for people with OCPD, they are egosyntonic; the person perceives them as rational and wanted, being the result of, for example, strong adherence to routines, a desire for control, or a need for perfection. OCPD is highly comorbid with other personality disorders, autism spectrum, eating disorders, anxiety, mood disorders, and substance use disorders. The disorder is the most common personality disorder in the United States, and is diagnosed twice as often in males as in females, however, there is evidence to suggest the prevalence between men and women is equal.
- substance use
- obsessive–compulsive
- autism
1. Signs and Symptoms
Obsessive–compulsive personality disorder (OCPD) is marked by an excessive obsession with rules, lists, schedules, and order; a need for perfectionism that interferes with efficiency and the ability to complete tasks; a devotion to productivity that hinders interpersonal relationships and leisure time; rigidity and zealousness on matters of morality and ethics; an inability to delegate responsibilities or work to others; restricted functioning in interpersonal relationships; restricted expression of emotion and affect; and a need for control over one's environment and self.[1][2]
Some of OCPD's symptoms are persistent and stable, whilst others are unstable. The obsession with perfectionism, reluctance to delegate tasks to others, and rigidity and stubbornness are stable symptoms. On the other hand, the symptoms that were most likely to change over time were the miserly spending style and the excessive devotion to productivity.[3] This discrepancy in the stability of symptoms may lead to mixed results in terms of the course of the disorder, with some studies showing a remission rate of 58% after a 12 month period, whilst others suggesting that the symptoms are stable and may worsen with age.[4]
1.1. Attention to Order and Perfection
People with OCPD tend to be obsessed with controlling their environments; to satisfy this need for control, they become preoccupied with trivial details, lists, procedures, rules, and schedules.[1]
This preoccupation with details and rules makes the person unable to delegate tasks and responsibilities to other people unless they submit to their exact way of completing a task because they believe that there is only one correct way of doing something. They stubbornly insist that a task or job must be completed their way, and only their way, and may micromanage people when they are assigned a group task. They are frustrated when other people suggest alternative methods. A person with this disorder may reject help even when they desperately need it as they believe that only they can do something correctly.[1]
People with OCPD are obsessed with maintaining perfection. The perfectionism and the extremely high standards that they establish are to their detriment and may cause delays and failures to complete objectives and tasks.[1] Every mistake is thought of as a major catastrophe that will soil their reputation for life. For example, a person may write an essay for a college, and then believe that it fell short of "perfection", so they continue rewriting it until they miss the deadline. They may never complete the essay due to the self-imposed high standards. They are unaware that other people may become frustrated and annoyed by the repeated delays and hassles that this behavior causes. Work relationships may then become a source of tension.[1]

1.2. Devotion to Productivity
Individuals with OCPD devote themselves to work and productivity at the expense of interpersonal relationships and recreation. Economic necessity, such as poverty, cannot account for this behavior.[1] They may believe that they do not have sufficient time to relax because they have to prioritize their work above all. They may refuse to spend time with friends and family because of that. They may find it difficult to go on a vacation, and even if they book a vacation, they may keep postponing it until it never happens. They may feel uncomfortable when they do go on a vacation and will take something along with them so they can work. They choose hobbies that are organized and structured, and they approach them as a serious task requiring work to perfect. The devotion to productivity in OCPD, however, is distinct from work addiction. OCPD is controlled and egosyntonic, whereas work addiction is uncontrolled and egodystonic, and the person afflicted may display signs of withdrawal.[5]
1.3. Rigidity
Individuals with OCPD are overconscientious, scrupulous, and rigid, and inflexible on matters of morality, ethics, and other areas of life. They may force themselves and others to follow rigid moral principles and strict standards of performance. They are self-critical and harsh about their mistakes. These symptoms should not be accounted for or caused by a person's culture or religion.[1] Their view of the world is polarised and dichotomous; there is no grey area between what is right and what is wrong. Whenever this dichotomous view of the world cannot be applied to a situation, this causes internal conflict as the person's perfectionist tendencies are challenged.[6]
People with this disorder are so obsessed with doing everything the "right and correct" way that they have a hard time understanding and appreciating the ideas, beliefs, and values of other people, and are reluctant to change their views, especially on matters of morality and politics.[1]
1.4. Restricted Emotions and Interpersonal Functioning
Individuals with this disorder may display little affection and warmth; their relationships and speech tend to have a formal and professional approach, and not much affection is expressed even to loved ones, such as greeting or hugging a significant other at an airport or train station.[1]
They are extremely careful in their interpersonal interactions. They have little spontaneity when interacting with others, and ensure that their speech follows rigid and austere standards by excessively scrutinising it. They filter their speech for embarrassing or imperfect articulation, and they have a low bar for what they consider to be such. They lower their bar even further when they are communicating with their superiors or with a person of high status. Communication becomes a time-consuming and exhausting effort, and they start avoiding it altogether. Others regard them as cold and detached as a result.[2]
Their need for restricting affect is a defense mechanism used to control their emotions.[2] They may expunge emotions from their memories and organize them as a library of facts and data; the memories are intellectualized and rationalized, not experiences that they can feel. This helps them avoid unexpected emotions and feelings and allows them to remain in control. They view self-exploration as a waste of time and have a patronising attitude towards emotional people.[2]
1.5. Interpersonal Control
Individuals with OCPD are at one extreme of the conscientiousness continuum. While conscientiousness is a desirable trait generally, its extreme presentation for those with OCPD leads to interpersonal problems. OCPD individuals present as over-controlled and this extends to the relationships they have with other people. Individuals with OCPD are referential to authority and rules. OCPD individuals may therefore punish those who violate their strict standards. The inability to accept differences in belief or behaviors from others often leads to high conflict and controlling relationships with coworkers, spouses, and children.[7]
1.6. Millon's Subtypes
In his book, Personality Disorders in Modern Life, Theodore Millon describes 5 types of obsessive–compulsive personality disorder, which he shortened to compulsive personality disorder.[2]
The Conscientious Compulsive
Millon described those with conscientious compulsive traits as displaying a dependent form of compulsive personality disorder. Those with conscientious compulsivity view themselves as helpful, co-operative, and compromising. They downplay their achievements and abilities and base their confidence on the opinions and expectations of others; this compensates for their feelings of insecurity and instability. They assume that devotion to work and striving for perfection will lead to them receiving love and reassurance. They believe that making a mistake or not achieving perfection will lead to abandonment and criticism. This mindset causes perpetual feelings of anxiety and an inability to appreciate their work.[2]:{{{1}}}
The Puritanical Compulsive
The puritanical compulsive is a blend of paranoid and compulsive features. They have strong internal impulses that are countered vociferously through the use of religion. They are constantly battling their impulses and sexual drives, which they view as irrational. They attempt to purify and pacify the urges by adopting a cold and detached lifestyle. They create an enemy which they use to vent their hostility, such as "non-believers", or "lazy people". They are patronizing, bigoted, and zealous in their attitude toward others. Their beliefs are polarized into "good" and "evil".[2]:231
The Bureaucratic Compulsive
The bureaucratic compulsive displays signs of narcissistic traits alongside the compulsivity. They are champions of tradition, values, and bureaucracy. They cherish organizations that follow hierarchies and feel comforted by definitive roles between subordinates and superiors, and the known expectations and responsibilities. They derive their identity from work and project an image of diligence, reliability, and commitment to their institution. They view work and productivity in a polarized manner; either done or not. They may use their power and status to inflict fear and obedience in their subordinates if they do not strictly follow their rules and procedures, and derive pleasure from the sense of control and power that they acquire by doing so.[2]:232–233
The Parsimonious Compulsive
The parsimonious compulsive is hoarding and possessive in nature; they behave in a manner congruent with schizoid traits. They are selfish, miserly, and are suspicious of others' intentions, believing that others may take away their possessions. This attitude may be caused by parents who deprived their child of wants or wishes but provided necessities, causing the child to develop an extreme protective approach to their belongings, often being self-sufficient and distant from others. They use this shielding behavior to prevent having their urges, desires, and imperfections discovered.[2]:233
The Bedevilled Compulsive
This form of compulsive personality is a mixture of negativistic and compulsive behavior. When faced with dilemmas, they procrastinate and attempt to stall the decision through any means. They are in a constant battle between their desires and will, and may engage in self-defeating behavior and self-torture in order to resolve the internal conflict. Their identity is unstable, and they are indecisive.[2]:235
2. Cause
The cause of OCPD is thought to involve a combination of genetic and environmental factors.[4] There is clear evidence to support the theory that OCPD is genetically inherited, however, the relevance and impact of genetic factors vary with studies placing it somewhere between 27% and 78%.[4]
Other studies have found links between attachment theory and the development of OCPD. According to this hypothesis, those with OCPD have never developed a secure attachment style, had overbearing parents, were shown little care, and were unable to develop empathetically and emotionally.[4]
3. Diagnosis
3.1. DSM-5
The fifth edition of the Diagnostic and Statistical Manual of Mental Disorders, a widely used manual for diagnosing mental disorders, places obsessive-compulsive personality disorder under section II, under the "personality disorders" chapter, and defines it as: "a pervasive pattern of preoccupation with orderliness, perfectionism, and mental and interpersonal control, at the expense of flexibility, openness, and efficiency, beginning by early adulthood and present in a variety of contexts". A diagnosis of OCPD is only received when four out of the eight criteria are met.
Alternative model for diagnosis
The DSM-5 also includes an alternative set of diagnostic criteria as per the dimensional model of conceptualising personality disorders. Under the proposed set of criteria, a person only receives a diagnosis when there is an impairment in two out of four areas of one's personality functioning, and when there are three out of four pathological traits, one of which must be rigid perfectionism.
The patient must also meet the general criteria C through G for a personality disorder, which state that the traits and symptoms being displayed by the patient must be stable and unchanging over time with an onset of at least adolescence or early adulthood, visible in a variety of situations, not caused by another mental disorder, not caused by a substance or medical condition, and abnormal in comparison to a person's developmental stage and culture/religion.
Differential diagnosis
There are several mental disorders in the DSM-5 that are listed as differential diagnoses for OCPD. They are as follows:
- Obsessive–compulsive disorder. OCD and OCPD have a similar name which may cause confusion; however, OCD can be easily distinguished from OCPD: OCPD is not characterized by true obsessions or compulsions.
- Hoarding disorder. A diagnosis of hoarding disorder is only considered when the hoarding behavior exhibited is causing severe impairment in the functioning of the person, such as an inability to access rooms in a house due to excessive hoarding.
- Narcissistic personality disorder. Individuals with a narcissistic personality disorder usually believe that they have achieved perfection (especially compared to other people) and cannot get better, whereas those with OCPD do not believe that they have achieved perfection, and are self-critical. Those with NPD tend to be stingy and lack generosity; however, they are usually generous when spending on themselves, unlike those with OCPD who hoard money and are miserly on themselves and others.
- Antisocial personality disorder. Similarly, individuals with antisocial personality disorder are not generous, but miserly around others, although they usually over-indulge themselves and are sometimes reckless in spending.
- Schizoid personality disorder. Schizoid personality disorder and obsessive-compulsive personality disorder may both display restricted affectivity and coldness; however, in OCPD, this is usually due to a controlling attitude, whereas, in SPD, it occurs due to a lack of ability to experience emotion and display affection.
- Other personality traits. Obsessive-compulsive personality traits may be particularly useful and helpful, especially in productive environments. Only when these traits become extreme, maladaptive, and cause clinically significant impairment in several aspects of one's life should a diagnosis of OCPD be considered.
- Personality change due to another medical condition. Obsessive-compulsive personality disorder must be differentiated from a personality change due to a medical condition, which affects the central nervous system, and may cause changes in behavior and traits.
- Substance use disorders. Substance use may cause the advent of obsessive-compulsive traits. It is necessary that this is distinguished from underlying and persistent behavior, which must occur when a person is not under influence of a substance.
3.2. ICD-10
The World Health Organization's ICD-10 uses the term anankastic personality disorder (F60.5).[8]
4. Comorbidity
Several disorders have been observed to have a higher risk of comorbidity with OCPD, they include: obsessive–compulsive disorder, eating disorders, Asperger's syndrome, depression, and anxiety.
4.1. Obsessive–Compulsive Disorder
OCPD is often confused with obsessive-compulsive disorder (OCD). Despite the similar names, they are two distinct disorders. Some OCPD individuals do have OCD, and the two can be found in the same family,[9] sometimes along with eating disorders.[10]
The rate of comorbidity of OCPD in patients with OCD is estimated to be around 15–28%.[11] However, due to the addition of the hoarding disorder diagnosis in the DSM-5, and studies showing that hoarding may not be a symptom of OCPD, the true rate of comorbidity may be much lower.[11]
There is significant similarity in the symptoms of OCD and OCPD, which can lead to complexity in distinguishing them clinically. For example, perfectionism is an OCPD criterion and a symptom of OCD if it involves the need for tidiness, symmetry, and organization. Hoarding is also considered both a compulsion found in OCD and a criterion for OCPD in the DSM-5. Even though OCD and OCPD are seemingly separate disorders there are obvious redundancies between the two concerning several symptoms.[12]
Regardless of similarities between the OCPD criteria and the obsessions and compulsions found in OCD, there are discrete qualitative dissimilarities between these disorders, predominantly in the functional part of symptoms. Unlike OCPD, OCD is described as invasive, and stressful. Time-consuming obsessions and habits are aimed at reducing obsession-related stress. OCD symptoms are at times regarded as egodystonic because they are experienced as alien and repulsive to the person. Therefore, there is a greater mental anxiety associated with OCD.[12]
In contrast, the symptoms seen in OCPD, although repetitive, are not linked with repulsive thoughts, images, or urges. OCPD characteristics and behaviors are known as ego-syntonic, as people with this disorder view them as suitable and correct. On the other hand, the main features of perfectionism and inflexibility can result in considerable suffering in an individual with OCPD as a result of the associated need for control.[12]
The presence of OCPD in patients with OCD has been linked to a worse prognosis of OCD, especially when cognitive behavioral therapy was used. This may be due to the ego-syntonic nature of OCPD which may lead to the obsessions becoming aligned with one's personal values. In contrast, the trait of perfectionism may improve the outcome of treatment as patients are likely to complete homework assigned to them with determination. The findings with regards to pharmacological treatment has also been mixed, with some studies showing a lower reception to SRIs in OCD patients with comorbid OCPD, with others showing no relationship.[11]
Comorbidity between OCD and OCPD has been linked to a more severe presentation of symptoms,[13] a younger age of onset,[11] more significant impairment in functioning, poorer insight, and higher comorbidity of depression and anxiety.[14]
4.2. Asperger's Syndrome
There are considerable similarities and overlap between Asperger's syndrome and OCPD,[15] such as list-making, inflexible adherence to rules, and obsessive aspects of Asperger's syndrome, although the latter may be distinguished from OCPD especially regarding affective behaviors, worse social skills, difficulties with Theory of Mind and intense intellectual interests, e.g. an ability to recall every aspect of a hobby.[16] A 2009 study involving adult autistic people found that 40% of those diagnosed with Asperger's syndrome met the diagnostic requirements for a comorbid OCPD diagnosis.[17]
4.3. Eating Disorders
In people with eating disorders, 13% also have OCPD.[4]
Regardless of the prevalence of the full-fledged OCPD among eating disordered samples, the presence of this personality disorder or its traits, such as perfectionism, has been found to be positively correlated with a range of complications in eating disorders and a negative outcome, as opposed to impulsive features—those linked with histrionic personality disorder, for example—which predict a better outcome from treatment.[18] OCPD predicts more severe symptoms of Anorexia Nervosa,[19] and worse remission rates,[19] however, OCPD and perfectionistic traits predicted a higher acceptance of treatment, which was defined as undergoing 5 weeks of treatment.[19]
People with Anorexia Nervosa who exercise excessively display a higher prevalence of several OCPD traits when compared to their counterparts who did not exercise excessively. The traits included self-imposed perfectionism, and the childhood OCPD traits of being rule-bound and cautious. It may be that people with OCPD traits are more likely to use exercise alongside restricting food intake in order to mitigate fears of increased weight, reduce anxiety, or reduce obsessions related to weight gain. Samples that had the childhood traits of rigidity, extreme cautiousness, and perfectionism endured more severe food restriction and higher levels of exercise and underwent longer periods of underweight status. It may be that OCPD traits are an indicator of a more severe manifestation of AN which is harder to treat.[20]
Perfectionism has been linked with AN in research for decades. A researcher in 1949 described the behavior of the average “anorexic girl” as being "rigid" and "hyperconscious", observing a tendency to "[n]eatness, meticulosity, and a mulish stubbornness not amenable to reason [which] make her a rank perfectionist".[21]
4.4. Other Disorders and Conditions
A diagnosis of OCPD is common with anxiety disorders, substance use disorders, and mood disorders.[4] OCPD is also highly comorbid with Cluster A personality disorders,[4]
| Psychiatric disorder | Prevalence of OCPD in 12 month diagnosis[4] |
|---|---|
| Substance use disorder | 12–25% |
| Mood disorders | 24% |
| Major depressive disorder | 23–28% |
| Bipolar disorder | 26–39% |
| Anxiety disorders | 23–24% |
| Generalised anxiety disorder | 34% |
| Panic disorder | 23–38% |
| Social anxiety disorder | 33% |
| Specific phobia | 22% |
especially paranoid and schizotypal personality disorders.[4] OCPD has also been linked to a higher relapse in those who are treated for major depressive disorder,[13] and a higher risk of suicidal behaviour.[13]
OCPD is also linked to hypochondriasis, with some studies estimating a rate of co-occurrence as high as 55.7%.[13]
Moreover, OCPD has been found to be very common among some medical conditions, including Parkinson's disease and the hypermobile subtype of Ehler-Danlos syndrome. The latter may be explained by the need for control that arises from musculoskeletal problems and the associated features that arise early in life, whilst the former can be explained by dysfunctions in the fronto-basal ganglia circuitry.[4]
5. Treatment

The best-validated treatment for OCPD is cognitive therapy (CT) or cognitive behavioral therapy (CBT), with studies showing an improvement in areas of personality impairment, and reduced levels of anxiety and depression.[4] Group CBT is also associated with an increase in extraversion and agreeableness and reduced neuroticism.[4] Interpersonal psychotherapy has been linked to even better results when it came to reducing depressive symptoms.[22]
6. Epidemiology
Estimates for the prevalence of OCPD in the general population range from 3% to 8%, making it the most common personality disorder. Some studies show no gender differences, but others show OCPD more prevalent among men. It is estimated to occur in 8.7% of psychiatric outpatient settings.[4]
7. History
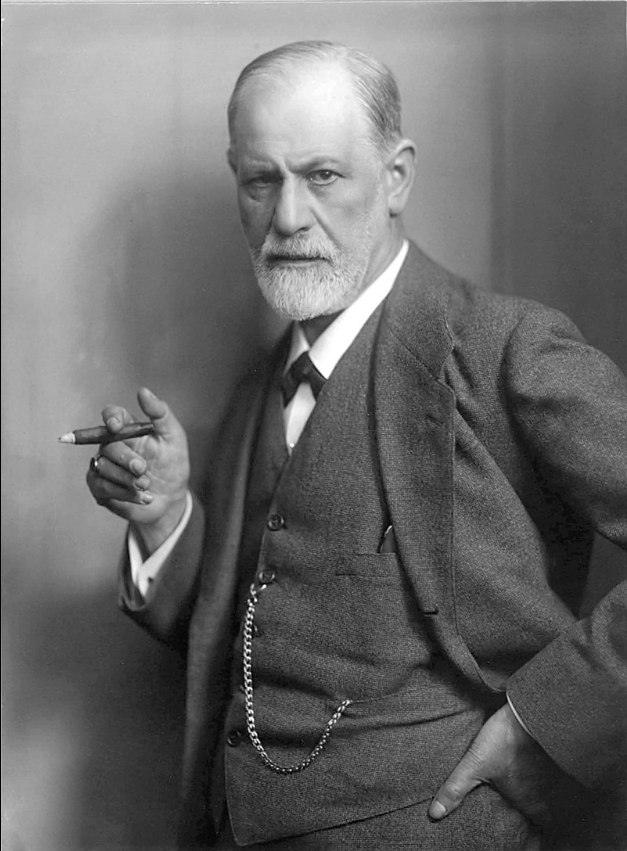
In 1908, Sigmund Freud named what is now known as obsessive–compulsive or anankastic personality disorder "anal retentive character".[23][24] He identified the main strands of the personality type as a preoccupation with orderliness, parsimony (frugality), and obstinacy (rigidity and stubbornness). The concept fits his theory of psychosexual development. Freud believed that the anal retentive character faced difficulties regulating the control of defecation, leading to repercussions by the parents, and it is the latter that would cause the anal retentive character.[25]
Aubrey Lewis, in 1936, in his book Problems of Obsessional Illness,[26] Lewis suggests that anal-erotic characteristics are found in patients without obsessive thoughts, and proposed two types of obsessional personality, one melancholy and stubborn, the other uncertain and indecisive.[27]
In the book Contributions to the theory of the anal character, Karl Abraham noted that the core feature of the anal character is being perfectionistic, and he believed that these traits will help an individual in becoming industrious and productive, whilst hindering their social and interpersonal functioning, such as working with others.[27]
OCPD was included in the first edition of the Diagnostic and Statistical Manual of Mental Disorders in 1952 by the American Psychiatric Association under the name "compulsive personality". It was defined as a chronic and excessive preoccupation with adherence to rules and standards of conscience. Other symptoms included rigidity, over-conscientiousness, and a reduced ability to relax.[28]
The DSM-II (1968) changed the name to "obsessive-compulsive personality", and also suggested the term "anankastic personality" in order to reduce confusion between OCPD and OCD, but the proposed name was removed from later editions. The symptoms described in the DSM-II closely resembled those in the original DSM.[29]
In 1980, the DSM-III was released, and it renamed the disorder back to "compulsive personality disorder", and also included new symptoms of the disorder: a restricted expression of affect, and an inability to delegate tasks. Devotion to productivity, perfectionism, and indecisiveness was the other symptoms included.[30] The DSM-III-R (1987) renamed the disorder again to "obsessive-compulsive personality disorder" and the name has remained since then. A diagnosis of OCPD was given when 5 of the 9 symptoms were met, and the 9 symptoms included perfectionism, preoccupation with details, an insistence that others submit to one's way, indecisiveness, devotion to work, restricted expression of affect, over conscientiousness, lack of generosity, and hoarding.[31]
With DSM-IV, OCPD was classified as a 'Cluster C' personality disorder. There was a dispute about the categorization of OCPD as an Axis II anxiety disorder. Although the DSM-IV attempted to distinguish between OCPD and OCD by focusing on the absence of obsessions and compulsions in OCPD, OC personality traits are easily mistaken for abnormal cognitions or values considered to underpin OCD. The disorder is neglected and understudied area of research.[32]
The content is sourced from: https://handwiki.org/wiki/Medicine:Obsessive%E2%80%93compulsive_personality_disorder
References
- Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) (5th ed.). United States: American Pyschiatric Association. May 18, 2013. pp. 678–681. ISBN 978-0-89042-554-1.
- Personality disorders in modern life. (2nd. ed.). Wiley. 2004. pp. 223–258. ISBN 978-0-471-23734-1.
- "Obsessive-compulsive (anankastic) personality disorder: toward the ICD-11 classification". Revista Brasileira de Psiquiatria 36 Suppl 1: 40–50. 2014. doi:10.1590/1516-4446-2013-1282. PMID 25388611. https://dx.doi.org/10.1590%2F1516-4446-2013-1282
- "Obsessive–compulsive personality disorder: a current review". Current Psychiatry Reports 17 (2): 2. February 2015. doi:10.1007/s11920-014-0547-8. PMID 25617042. https://dx.doi.org/10.1007%2Fs11920-014-0547-8
- "Work Addiction, Obsessive-Compulsive Personality Disorder, Burn-Out, and Global Burden of Disease: Implications from the ICD-11". International Journal of Environmental Research and Public Health 17 (2): 660. January 2020. doi:10.3390/ijerph17020660. PMID 31968540. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=7014139
- "Living with obsessional personality". BJPsych Bulletin 41 (6): 366–367. December 2017. doi:10.1192/pb.41.6.366a. PMID 29234518. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=5709690
- Hertler, Steven C. (June 1, 2014). "The Continuum of Conscientiousness: The Antagonistic Interests among Obsessive and Antisocial Personalities". Polish Psychological Bulletin 45 (2): 167–178. doi:10.2478/ppb-2014-0022. https://psycnet.apa.org/record/2014-32977-009.
- "Anankastic personality disorder". International Statistical Classification of Diseases and Related Health Problems. http://apps.who.int/classifications/icd10/browse/2010/en#/F60.5.
- "Personality disorders and normal personality dimensions in obsessive–compulsive disorder". The British Journal of Psychiatry: The Journal of Mental Science 177 (5): 457–62. November 2000. doi:10.1192/bjp.177.5.457. PMID 11060001. https://dx.doi.org/10.1192%2Fbjp.177.5.457
- "The relation among perfectionism, obsessive–compulsive personality disorder and obsessive–compulsive disorder in individuals with eating disorders". The International Journal of Eating Disorders 38 (4): 371–4. December 2005. doi:10.1002/eat.20190. PMID 16231356. https://dx.doi.org/10.1002%2Feat.20190
- Thamby, Abel; Khanna, Sumant (January 2019). "The role of personality disorders in obsessive–compulsive disorder". Indian Journal of Psychiatry 61 (Suppl 1): S114–S118. doi:10.4103/psychiatry.IndianJPsychiatry_526_18. ISSN 0019-5545. PMID 30745684. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=6343421
- Pinto, Anthon y; Eisen, Jane L.; Mancebo, Maria C.; Rasmussen, Steven A. (2008). "Obsessive–Compulsive Personality Disorder". Obsessive–Compulsive Disorder: Subtypes and Spectrum Conditions. Elsevier. pp. 246–263. ISBN 978-0-08-044701-8. http://ac.els-cdn.com/B9780080447018500164/3-s2.0-B9780080447018500164-main.pdf?_tid=5e5920c6-6e10-11e6-8885-00000aab0f02&acdnat=1472492906_7d594e8d9e99c696b9336666dab25769.
- "New diagnostic perspectives on obsessive–compulsive personality disorder and its links with other conditions" (in en-US). Current Opinion in Psychiatry 27 (1): 62–7. January 2014. doi:10.1097/YCO.0000000000000030. PMID 24257122. https://dx.doi.org/10.1097%2FYCO.0000000000000030
- "The neuropsychology of obsessive–compulsive personality disorder: a new analysis". CNS Spectrums 20 (5): 490–9. October 2015. doi:10.1017/S1092852914000662. PMID 25776273. https://dx.doi.org/10.1017%2FS1092852914000662
- "Autism and Asperger syndrome: coexistence with other clinical disorders". Acta Psychiatrica Scandinavica 102 (5): 321–30. November 2000. doi:10.1034/j.1600-0447.2000.102005321.x. PMID 11098802. https://dx.doi.org/10.1034%2Fj.1600-0447.2000.102005321.x
- Fitzgerald, Michael; Corvin, Aiden (2001-07-01). "Diagnosis and differential diagnosis of Asperger syndrome". Advances in Psychiatric Treatment 7 (4): 310–318. doi:10.1192/apt.7.4.310. ISSN 1355-5146. https://dx.doi.org/10.1192%2Fapt.7.4.310
- "Psychiatric and psychosocial problems in adults with normal-intelligence autism spectrum disorders". BMC Psychiatry 9 (1): 35. June 2009. doi:10.1186/1471-244x-9-35. PMID 19515234. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2705351
- "Eating disorders and personality: a methodological and empirical review". Clinical Psychology Review 26 (3): 299–320. May 2006. doi:10.1016/j.cpr.2005.10.003. PMID 16330138. https://dx.doi.org/10.1016%2Fj.cpr.2005.10.003
- "Are obsessive–compulsive personality traits associated with a poor outcome in anorexia nervosa? A systematic review of randomized controlled trials and naturalistic outcome studies". The International Journal of Eating Disorders 40 (7): 581–8. November 2007. doi:10.1002/eat.20419. PMID 17607713. https://dx.doi.org/10.1002%2Feat.20419
- "The relationship between obsessive-compulsive personality disorder traits, obsessive-compulsive disorder and excessive exercise in patients with anorexia nervosa: a systematic review". Journal of Eating Disorders 1 (1): 16. May 2013. doi:10.1186/2050-2974-1-16. PMID 24999397. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4081792
- "Compulsion neurosis with cachexia (anorexia nervosa)". The American Journal of Psychiatry 106 (2): 107–15. August 1949. doi:10.1176/ajp.106.2.107. PMID 18135398. https://dx.doi.org/10.1176%2Fajp.106.2.107
- "Obsessive-Compulsive Personality Disorder". https://www.lecturio.com/concepts/cluster-c-personality-disorders/.
- Haslam, Nick (2016), "Anal Expulsive/Anal Retentive Personality", in Zeigler-Hill, Virgil; Shackelford, Todd K. (in en), Cham: Springer International Publishing, pp. 1–2, doi:10.1007/978-3-319-28099-8_1357-1, ISBN 978-3-319-28099-8 https://dx.doi.org/10.1007%2F978-3-319-28099-8_1357-1
- Freud, Sigmund. Jensen's 'Gradiva' and Other Works (1906-1908). 9 (Standard ed.). Karnac Books. https://www.karnacbooks.com/product/standard-edition-vol-9-jensens-gradiva-and-other-works-1906-1908/6878/. Retrieved 2020-08-02.
- The Freud Reader. W. W. Norton & Company. September 1995. ISBN 978-0393314038.
- Lewis, Aubrey (February 1936). "Problems of Obsessional Illness". Proceedings of the Royal Society of Medicine 29 (4): 325–336. doi:10.1177/003591573602900418. ISSN 0035-9157. PMID 19990606. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=2075767
- Obsessive–compulsive personality disorder. Washington, D.C.: American Psychiatric Association Publishing. October 2019. pp. 3. ISBN 978-1-61537-280-5. OCLC 45375754. http://www.worldcat.org/oclc/45375754
- Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association. 1952. pp. 57.
- Diagnostic and Statistical Manual of Mental Disorders (2nd ed.). American Psychiatric Association. 1968. pp. 43.
- Diagnostic and Statistical Manual of Mental Disorders (3rd ed.). American Psychiatric Association. 1980. pp. 326–328.
- Diagnostic and statistical manual of mental disorders: DSM-III-R.. American Psychiatric Association., American Psychiatric Association. Work Group to Revise DSM-III. (3rd, revised ed.). Washington, DC. pp. 354–356. ISBN 0-89042-018-1. OCLC 16395933. http://www.worldcat.org/oclc/16395933
- "Obsessive-compulsive (Anankastic) Personality Disorder: A Poorly Researched Landscape with Significant Clinical Relevance". Indian Journal of Psychological Medicine 38 (1): 1–5. 2016. doi:10.4103/0253-7176.175085. PMID 27011394. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pmcentrez&artid=4782437
