Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Alzheimer’s disease is the most common form of dementia, and the prodromal phases of Alzheimer’s disease can last for decades. Vascular dementia is the second most common form of dementia and is distinguished from Alzheimer’s disease by evidence of previous stroke or hemorrhage and current cerebrovascular disease. A compiled group of vascular-related dementias (vascular dementia and unspecified dementia) is often referred to as non-Alzheimer dementia.
- Alzheimer’s disease
- vascular dementia
- body mass index
- lipids
1. Introduction
Dementia is a clinical diagnosis defined by cognitive symptoms that interfere with the ability to function at usual activities [1]. It is a devastating neurodegenerative disease affecting more than 50 million individuals worldwide [2]. The most common symptoms are problems with memory, language, problem solving, and other thinking skills [3], and it is preceded by a period during which individuals have subtle cognitive changes called mild cognitive impairment (MCI) [3]. The dementia syndrome is categorized as mild, moderate, or severe [3].
Alzheimer’s disease is the most common form of dementia, and the prodromal phases of Alzheimer’s disease can last for decades [4]. The disease is categorized as early-onset (before age 65) and late-onset (after age 65) dementia [5]. It has been viewed as a mysterious disease with no single obvious cause, different hypotheses regarding its pathogenesis, and no curative treatment. Even though β-amyloid is the pathological hallmark of Alzheimer’s disease, the amyloid cascade hypothesis that states Alzheimer’s disease is mainly caused by the accumulation of toxic β-amyloid [6] has been challenged several times. Clinical randomized trials aimed at reducing the β-amyloid burden have failed to show any effect on disease endpoint [7][8][9][10][11], and β-amyloid plaques have been shown to be present in cognitively normal individuals [12] and individuals without dementia [13].
Vascular dementia is the second most common form of dementia and is distinguished from Alzheimer’s disease by evidence of previous stroke or hemorrhage and current cerebrovascular disease [3]. Other types of dementia include frontotemporal [14], Lewy body dementia [15], unspecified dementia [3], and mixed dementia [3]. Many of the types of dementia in the unspecified dementia category are likely to be of vascular origin, and therefore, unspecified dementia and vascular dementia are often categorized as non-Alzheimer dementia [16][17]. This classification will be used throughout the review.
Recent evidence indicates that curing or reverting Alzheimer’s disease in the prodromal phases or after disease onset is futile. In contrast, preventing the disease by lifestyle interventions early in life with a focus on reducing cardiovascular risk factors is a promising strategy for reducing the future risk of dementia [16][18]. One study estimated that approximately 40% of dementia cases worldwide could be prevented by targeting modifiable, primarily cardiovascular risk factors [2]. Furthermore, neuroimaging studies have suggested that early vascular dysregulation is the initial pathologic event leading to late-onset Alzheimer’s disease [19][20].
2. Alzheimer’s Disease and Vascular Dementia
General diagnostic criteria for dementia according to the International Classification of Diseases (ICD) version 10 include: (1) decline in memory and decline in other cognitive functions, (2) preserved consciousness sufficient to be able to judge decline in memory, (3) weakening of emotional control, motivation, or social interaction, (4) duration of more than 6 months. In addition, the symptoms must not be explained by other major psychiatric disorders [3]. Dementia has many causes, and Alzheimer’s disease and vascular dementia are the two most common. A diagnosis of either form of dementia is based on family and medical history, cognitive tests such as the Mini-Mental State Examination (MMSE), and input from close relatives about the patient’s changes in behavior, abilities, and/or mood [3][4].
Alzheimer’s disease was first described in 1907 by Alois Alzheimer [21]. The post-mortem examination of the patient’s brain was described with arteriosclerotic changes in the vascular tissues and thick bundles of neurofibrils that stained with dyes that normally would not stain neurofibrils (later known as neurofibrillary tangles) [21]. Biomarkers can be used to distinguish Alzheimer’s disease from other types of dementia [4]. These include early signs of Alzheimer’s disease such as abnormal levels of β-amyloid shown either by examination of cerebrospinal fluid or in positron emission tomography (PET) scans and decreased glucose metabolism shown on PET scans [4].
Vascular dementia has different causes which can be classified according to the following [22]: multiple infarcts, strategic single-infarct, small-vessel disease with dementia, hypoperfusion, hemorrhagic dementia, and other causes [22]. Alzheimer’s disease and vascular dementia share many clinical features and their differential diagnosis requires brain imaging and or/postmortem assessment [23]. The pathological characteristics of vascular dementia are microinfarcts, lacunar infarcts, arteriosclerosis, lesions caused by hemorrhages, fibroid necrosis, and hyalinosis [23]. While all these features can also be seen in Alzheimer’s disease, the pathological hallmark of Alzheimer’s disease is the accumulation of β-amyloid [23][24]. When β-amyloid accumulates in the capillaries of the brain it causes cerebral amyloid angiopathy, which is very often seen in Alzheimer’s disease and often causes cerebral hemorrhages [24]. Cerebral amyloid angiopathy is also present in vascular dementia, however, amyloid plaques are rarely seen [24].
3. Shared Risk Factors between Dementia and Atherosclerotic Cardiovascular Disease
Recently, an increasing amount of evidence points towards risk factors for atherosclerotic cardiovascular disease as risk factors for dementia [16]. Diabetes mellitus type 2 and midlife hypertension have been robustly associated with risk of dementia, whereas other risk factors such as obesity, plasma concentrations of LDL cholesterol, HDL cholesterol, triglycerides and total cholesterol, NAFLD, diet, the gut microbiome, smoking, and physical inactivity are less well-established risk factors [16]. Increasing evidence also suggests that genetic factors may be shared risk factors for dementia and atherosclerotic cardiovascular disease [16][17][18]. The associations between risk factors and dementia vary according to what time point in life they have been measured and which type of dementia is the outcome. This often complicates the interpretation of research within this field. An overview of shared risk factors between dementia and atherosclerotic cardiovascular disease is given in Figure 1.
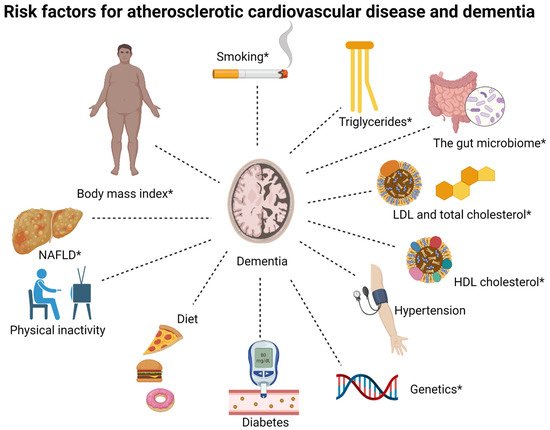
Figure 1. Overview of shared risk factors between dementia and atherosclerotic cardiovascular disease. LDL, low-density lipoprotein; HDL, high-density lipoprotein; NAFLD, non-alcoholic fatty liver disease. The associations for some risk factors differ between Alzheimer’s disease and non-Alzheimer dementia, specifically, body mass index, triglycerides, HDL cholesterol, NAFLD, the gut microbiome, smoking, and genetics (these are marked by *).
This entry is adapted from the peer-reviewed paper 10.3390/ijms23179777
References
- McKhann, G.M.; Knopman, D.S.; Chertkow, H.; Hyman, B.T.; Jack, C.R.; Kawas, C.H.; Klunk, W.E.; Koroshetz, W.J.; Manly, J.J.; Mayeux, R.; et al. The Diagnosis of Dementia Due to Alzheimer’s Disease: Recommendations from the National Institute on Aging-Alzheimer’s Association Workgroups on Diagnostic Guidelines for Alzheimer’s Disease. Alzheimer’s Dement. 2011, 7, 263–269.
- Livingston, G.; Huntley, J.; Sommerlad, A.; Ames, D.; Ballard, C.; Banerjee, S.; Brayne, C.; Burns, A.; Cohen-Mansfield, J.; Cooper, C.; et al. Dementia Prevention, Intervention, and Care: 2020 Report of the Lancet Commission. Lancet 2020, 396, 413–446.
- World Health Organization. ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research; World Health Organization: Geneva, Switzerland, 1993.
- 2021 Alzheimer’s Disease Facts and Figures. Alzheimer’s Dement. 2021, 17, 327–406.
- Cacace, R.; Sleegers, K.; Van Broeckhoven, C. Molecular Genetics of Early-Onset Alzheimer’s Disease Revisited. Alzheimer’s Dement. 2016, 12, 733–748.
- Hardy, J.A.; Higgins, G.A.; Hardy, J.A.; Higgins, G.A. Alzheimer ’ s Disease: The Amyloid Cascade Hypothesis Published by: American Association for the Advancement of Science Alzheimer ’ s Disease: The Amyloid Cascade Hypothesis. Science 1992, 256, 184–185.
- Salloway, S.; Sperling, R.; Fox, N.C.; Blennow, K.; Klunk, W.; Raskind, M.; Sabbagh, M.; Honig, L.S.; Porsteinsson, A.P.; Ferris, S.; et al. Two Phase 3 Trials of Bapineuzumab in Mild-to-Moderate Alzheimer’s Disease. N. Engl. J. Med. 2014, 370, 322–333.
- Honig, L.S.; Vellas, B.; Woodward, M.; Boada, M.; Bullock, R.; Borrie, M.; Hager, K.; Andreasen, N.; Scarpini, E.; Liu-Seifert, H.; et al. Trial of Solanezumab for Mild Dementia Due to Alzheimer’s Disease. N. Engl. J. Med. 2018, 378, 321–330.
- Laske, C. Phase 3 Trials of Solanezumab and Bapineuzumab for Alzheimer’s Disease. N. Engl. J. Med. 2014, 370, 1459–1460.
- Holmes, C.; Boche, D.; Wilkinson, D.; Yadegarfar, G.; Hopkins, V.; Bayer, A.; Jones, R.W.; Bullock, R.; Love, S.; Neal, J.W.; et al. Long-Term Effects of Aβ42 Immunisation in Alzheimer’s Disease: Follow-up of a Randomised, Placebo-Controlled Phase I Trial. Lancet 2008, 372, 216–223.
- Ostrowitzki, S.; Lasser, R.A.; Dorflinger, E.; Scheltens, P.; Barkhof, F.; Nikolcheva, T.; Ashford, E.; Retout, S.; Hofmann, C.; Delmar, P.; et al. A Phase III Randomized Trial of Gantenerumab in Prodromal Alzheimer’s Disease. Alzheimer’s Res. Ther. 2017, 9, 1–15.
- Erten-Lyons, D.; Woltjer, R.L.; Dodge, H.; Nixon, R.; Vorobik, R.; Calvert, J.F.; Leahy, M.; Montine, T.; Kaye, J. Factors Associated with Resistance to Dementia despite High Alzheimer Disease Pathology. Neurology 2009, 72, 354–360.
- Bennett, D.A.; Schneider, J.A.; Arvanitakis, Z.; Kelly, J.F.; Aggarwal, N.T.; Shah, R.C.; Wilson, R.S. Neuropathology of Older Persons without Cognitive Impairment from Two Community-Based Studies. Neurology 2006, 66, 1837–1844.
- McKhann, G.M. Clinical and Pathological Diagnosis of Frontotemporal Dementia. Arch. Neurol. 2001, 58, 1803.
- McKeith, I.G.; Dickson, D.W.; Lowe, J.; Emre, M.; O’Brien, J.T.; Feldman, H.; Cummings, J.; Duda, J.E.; Lippa, C.; Perry, E.K.; et al. Diagnosis and Management of Dementia with Lewy Bodies: Third Report of the DLB Consortium. Neurology 2005, 65, 1863–1872.
- Rasmussen, I.J.; Thomassen, J.Q.; Frikke-Schmidt, R. Impact of Metabolic Dysfunction on Cognition in Humans. Curr. Opin. Lipidol. 2021, 32, 55–61.
- Nordestgaard, L.T.; Christoffersen, M.; Afzal, S.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Frikke-Schmidt, R. Triglycerides as a Shared Risk Factor between Dementia and Atherosclerotic Cardiovascular Disease: A Study of 125 727 Individuals. Clin. Chem. 2021, 67, 245–255.
- Rasmussen, I.J.; Rasmussen, K.L.; Nordestgaard, B.G.; Tybjærg-Hansen, A.; Frikke-Schmidt, R. Impact of Cardiovascular Risk Factors and Genetics on 10-Year Absolute Risk of Dementia—Risk Charts for Targeted Prevention. Eur. Heart J. 2020, in press.
- Iturria-Medina, Y.; Sotero, R.C.; Toussaint, P.J.; Mateos-Pérez, J.M.; Evans, A.C.; Weiner, M.W.; Aisen, P.; Petersen, R.; Jack, C.R.; Jagust, W.; et al. Early Role of Vascular Dysregulation on Late-Onset Alzheimer’s Disease Based on Multifactorial Data-Driven Analysis. Nat. Commun. 2016, 7.
- Iturria-Medina, Y.; Carbonell, F.M.; Sotero, R.C.; Chouinard-Decorte, F.; Evans, A.C. Multifactorial Causal Model of Brain (Dis)Organization and Therapeutic Intervention: Application to Alzheimer’s Disease. Neuroimage 2017, 152, 60–77.
- Stelzmann, R.A.; Norman Schnitzlein, H.; Reed Murtagh, F. An English Translation of Alzheimer’s 1907 Paper, “Über Eine Eigenartige Erkankung Der Hirnrinde. ” Clin. Anat. 1995, 8, 429–431.
- Roman, G.C.; Tatemichi, T.K.; Erkinjuntti, T.; Cummings, J.L.; Masdeu, J.C.; Garcia, J.H. Vascular Dementia: Diagnostic Criteria for Research Studies: Report of the NINDS-AIREN International Workshop Vascular Dementia: Diagnostic Criteria for Research Studies: Report of the NINDS-AIREN International Workshop 1993. Neurology 1993, 43, 250–260.
- Salminen, A.; Kauppinen, A.; Kaarniranta, K. Hypoxia/Ischemia Activate Processing of Amyloid Precursor Protein: Impact of Vascular Dysfunction in the Pathogenesis of Alzheimer’s Disease. J. Neurochem. 2017, 140, 536–549.
- Braak, H.; Braak, E. Demonstration of Amyloid Deposits and Neurofibrillary Changes in Whole Brain Sections. Brain Pathol. 1991, 1, 213–216.
This entry is offline, you can click here to edit this entry!
