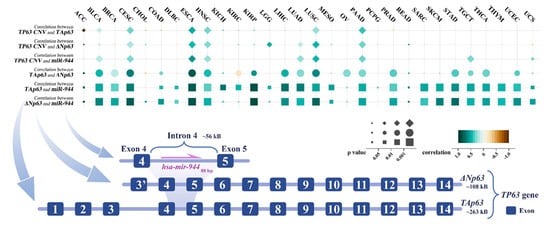
miR-944 is localized in intron 4 of TP63. ΔNp63 in intron 3 of TP63 recruits the transcription factor AP-2 to promote miR-944 gene expression, which mediates epidermal differentiation induction by ΔNp63. miR-944 is dysregulated in various cancers. In squamous cell carcinoma. miR-944 can target and inhibit 27 protein-coding genes, thereby regulating cell cycle, proliferation, apoptosis, epithelial mesenchymal transition, cancer cell invasion and migration, and other cell behaviors. The genes targeted by miR-944 are involved in three signaling pathways, including the Wnt/β-catenin pathway, Jak/STAT3 pathway, and PI3K/AKT pathway. miR-944 was regulated by a total of 11 competing endogenous RNAs, including 6 circular RNAs and 5 long non-coding RNAs. Abnormally expressed miR-944 can act as an independent prognostic factor and is closely related to tumor invasion, lymph node metastasis, TNM staging, and drug resistance. miR-944 is expected to become a critical biomarker with great clinical application value in cancer.
- miR-944
- ceRNA
- dysregulation
- diagnosis
1. Introduction
2. miR-944 and Its Host Gene TP63
3. Aberrant Expression of miR-944 in Cancer
| Physiological System | Cancer | miR-944 Expression | Cell Line | Tissue or Serum | Ref. |
|---|---|---|---|---|---|
| Nervous system | GBM/LGG | Downregulated | HA1800 versus SHG44, U87MG, and U251MG | Paracancerous tissues versus glioma tissues from 5 patients | [28] |
| Respiratory system | NPC | Downregulated | NP69 versus C666-1, CNE1, CNE2, and HNE1 | Paracancerous tissues versus tumor tissues from 20 NPC patients | [29] |
| Downregulated | NP69 versus CNU46, SUNE1, HONE1, 6–10 B, CNE1, CNE2, and HNE1 | Nasopharyngeal mucosa tissues from 30 healthy people versus primary tumor tissues from 30 NPC patients | [7] | ||
| LUAD | Downregulated | 16HBE versus A549, H1299, SK-Lu-1, and PC-9 | Paracancerous tissues versus LUAD tissues from 25 patients | [30] | |
| LUSC | Upregulated | — | Paracancerous tissues from patients versus SCC tissues from patients | [21] | |
| NSCLC | Downregulated | BEAS-2B versus H522 and H1975 | — | [15] | |
| Downregulated | BEAS-2B versus H358, H1299, PC-9, and A549 | Paracancerous tissues versus tumor tissues from 65 NSCLC patients | [31] | ||
| Downregulated | BEAS-2B versus A549, H226, H292, ANP973, and H1299 | Paracancerous tissues versus tumor tissues from 60 NSCLC patients | [32] | ||
| Downregulated | — | Paracancerous tissues versus tumor tissues from 9 NSCLC patients | [2] | ||
| Digestive system | TSCC | Downregulated | normal gingival epithelial cells versus SCC-9, CAL-27, and SCC-15 | Paracancerous tissues versus TSCC tissues from 57 patients | [33] |
| ECa | Downregulated | — | Paracancerous tissues versus adenocarcinoma tissues from 59 eca patients; serum exosomes from healthy persons versus serum exosomes from 59 eca patients | [20] | |
| GC | Downregulated | GES-1 versus AGS, MKN-1, HGC-27, MKN-45, SGC-7901, and BGC-823 | — | [34] | |
| Downregulated | GES-1 versus SGC-7901, MGC-803, MKN-28, and BGC-823 | Paracancerous tissues versus tumor tissues from 40 GC patients | [35] | ||
| HCC | Downregulated | L02 versus Hep3B, Bel-7402, SMMC-7721, Huh7, and SK-HEP-1 | Paracancerous tissues versus tumor tissues from 61 HCC patients | [36] | |
| CRC | Downregulated | HIEC and HEK293 versus HCT116, Caco-2, HT29, SW620, and SW480 | — | [9] | |
| Downregulated | COS7 versus HCT116, LoVo, RKO, HCT15, HT29, SW480, and SW620 | — | [37] | ||
| Downregulated | — | Paracancerous tissues versus fresh CRC tissues from 140 CRC patients | [8] | ||
| Downregulated | CCC-HIE-2 versus HT-29, HCT116, SW480, and SW620 | Paracancerous tissues versus fresh CRC tissues from 100 CRC patients | [38] | ||
| Reproductive system | EC | Upregulated | — | Normal endometrial tissues from 20 non-cancer patients versus tumor tissues from 68 EC patients | [22] |
| CxCa | Upregulated | — | Paracancerous tissues versus tumor tissues from 27 cxca patients | [25] | |
| Upregulated | — | Serum specimens from 24 women with localized disease versus serum specimens from 25 women with metastatic disease | [24] | ||
| Upregulated | HcerEpiC versus HeLa, CaSki, SiHa, and C33A | Paracancerous tissues versus fresh cxca tissues from 70 cxca patients | [23] | ||
| Upregulated | — | 50 FFPE normal cervical tissue samples versus 66 FFPE cxca tissue samples | [5] | ||
| BrC | Downregulated | MCF-10A versus MDA-MB-231, MCF-7, MDA-MB-453, ZR-75, and T47-D | Paracancerous tissues versus locally invasive breast tumors tissues from brc patients | [27] | |
| Upregulated | — | Paracancerous tissues versus tumor tissues from 40 brc patients; serum samples from 30 healthy people versus serum samples from 30 brc patients | [26] | ||
| Motor system | SaOS | Downregulated | hFOB1.19 versus MG-63, SAOS-2, HOS, and U2OS | Paracancerous tissues versus tumor tissues from 38 saos patients | [39] |
| COF | Downregulated | — | Bone tissues from 10 healthy people versus bone tissues from 9 COF patients | [3] |
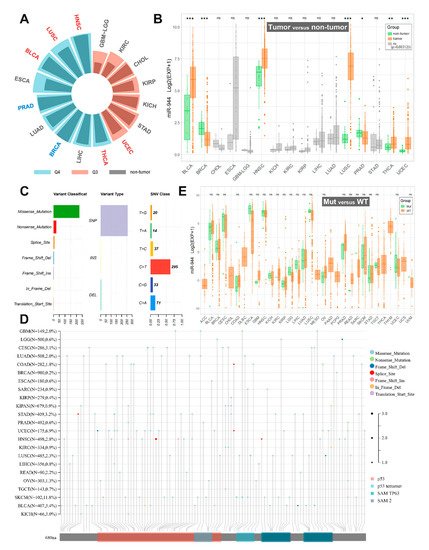
| TCGA Cancers | Sample Size (T/N) | miR-944 Expression in TCGA | miR-944 Expression in the Present Studies |
|---|---|---|---|
| BLCA | 405/18 | Upregulated; Q4 | Not studied |
| BRCA | 624/74 | Downregulated; Q4 | Downregulated in BrC tissues and BrC cells (MDA-MB-231, MCF-7, MDA-MB-453, ZR-75, and T47-D) [27]; and Upregulated in BrC tissues and serum sample of BrC patients [26] |
| CHOL | 20/8 | ns; Q3 | Not studied |
| ESCA | 176/8 | ns; Q4 | Downregulated in ECa tissues and serums of ECa patients [20] |
| GBM/LGG | 209/3 | ns; Q3 | Downregulated in GBM/LGG tissues and GBM/LGG cells (SHG44, U87MG, and U251MG) [28] |
| HNSC | 485/44 | Upregulated; Q4 | Not studied |
| KICH | 49/8 | ns; Q3 | Not studied |
| KIRC | 108/19 | ns; Q3 | Not studied |
| KIRP | 155/23 | ns; Q3 | Not studied |
| LIHC | 324/47 | ns; Q4 | Downregulated in HCC tissues and HCC cells (Hep3B, Bel-7402, SMMC-7721, Huh7, and SK-HEP-1) [36] |
| LUAD | 430/40 | ns; Q4 | Downregulated in LUAD tissues and LUAD cells (A549, H1299, SK-Lu-1, and PC-9) [30] |
| LUSC | 334/44 | Upregulated; Q4 | Upregulated in LUSC tissues [21] |
| PRAD | 437/50 | Downregulated; Q4 | Not studied |
| STAD | 303/26 | ns; Q3 | Downregulated in GC tissues and GC cells (AGS, MKN-1, HGC-27, MKN-45, SGC-7901, MGC-803, BGC-823, and MKN-28) [34,35] |
| THCA | 420/50 | Upregulated; Q4 | Not studied |
| UCEC | 330/26 | Upregulated; Q3 | Upregulated in EC tissues [22] |
4. Co-Expression of TP63 Transcripts and miR-944
This entry is adapted from the peer-reviewed paper 10.3390/cancers14174232
