Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cardiac & Cardiovascular Systems
Extracellular vesicles are particles released from cells and delimited by a lipid bilayer. They have been widely studied, including extensive investigation in cardiovascular diseases. In this entry we focus on their role in atrial fibrillation.
- atrial fibrillation
- extracellular vesicles
- microRNA
- ablation
1. Preclinical Studies
It was proven that cardiomyocytes, treated with the EVs derived from myofibroblasts, showed the downregulation of L-type calcium channel Cav1.2. This downregulation is considered to be a characteristic feature of the ionic remodeling associated with AF [18]. Additionally, EVs derived from the angiotensin II-treated human cardiac myocytes encouraged macrophages to conducted M1 polarization and, consequently, proinflammatory state; moreover, it was evidenced that Plasmacytoma Variant Translocation 1 (PVT1) contained in EVs promoted extracellular matrix remodeling in atrial fibroblasts [19].
Another research group established that beagles undergoing rapid atrial pacing for 7 days showed a rise in the atrial and plasma EVs release; moreover, it was effectively hampered by GW4869, a commonly used agent inhibiting EVs generation. It was also suggested that miR-21-5p could play a role, as it was upregulated in both atrial and plasma EVs [20]. EVs originating from mouse adipose-tissue-derived mesenchymal stem cells and transfected with the X-inactive specific transcript (XIST) caused a decrease in inflammation and myocardial pyroptosis [21]. In a recent study, EVs from bone marrow mesenchymal stem cells were transduced with the nuclear factor-erythroid 2-related factor 2 (Nrf2). These EVs injected into rats with AF not only shortened AF duration and reduced cardiomyocyte apoptosis but also minimized atrial fibrosis [22]. It was also proven that EVs derived from bone marrow mesenchymal stem cells overexpressing miR-148a reduced cardiomyocyte apoptosis by inhibiting SPARC-associated modular calcium-binding protein 2 (SMOC2) [23]. The preclinical studies discussed in this subsection are graphically summarized in Figure 1.
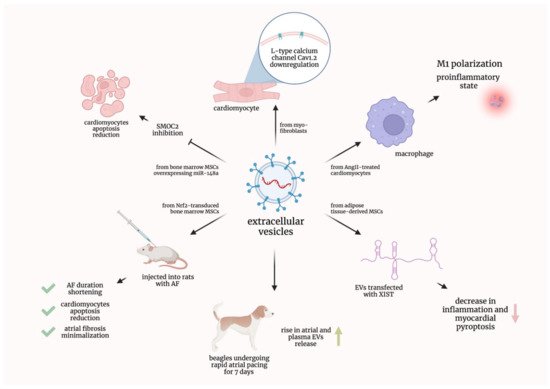
Figure 1. Graphical summarization of the preclinical studies concerning extracellular vesicles in atrial fibrillation. AF—atrial fibrillation; AngII—Angiotensin II; EVs—extracellular vesicles; miR—micro-ribonucleic acid; MSCs—mesenchymal stem cells; Nrf2—nuclear factor-erythroid 2-related factor 2; SMOC2—SPARC-associated modular calcium-binding protein 2; XIST—X-inactive specific transcript.
2. EVs in Atrial Fibrillation Patients Treated with Anticoagulants and Other Drugs
Chirinos et al. investigated the association between digoxin use in patients suffering from non-valvular AF and the level of EVs originating from endothelium and platelets. They showed that patients taking digoxin exhibited increased levels of endothelial EVs [24]. Lau et al. studied the population of AF patients treated with warfarin. It was shown that endothelial and platelet EVs collectively negatively correlated with the estimated glomerular filtration rate (eGFR), making them potential nephrotoxicity biomarkers. However, platelet-derived EVs alone did not present any correlation with the eGFR [25]. Lenart-Migdalska et al. studied the impact of dabigatran intake on platelet and endothelial EV concentration in non-valvular AF patients. Platelet-derived EVs were increased in patients treated with dabigatran; moreover, dabigatran concentration correlated negatively with the concentration change among these EVs. Endothelial-derived EVs did not exhibit such relationships [26]. The same research group evidenced that non-valvular AF patients treated with rivaroxaban presented increased levels of both platelet- and endothelial-derived EVs after drug administration [27]. Moreover, Weiss et al. demonstrated that non-valvular AF patients treated with rivaroxaban had a significantly altered proteomic profile of EVs compared with those treated with warfarin; proinflammatory proteins and complement factors were decreased, whereas negative regulators of inflammatory pathways were elevated in patients treated with rivaroxaban [28]. Complementary to the aforementioned studies, Duarte et al. showed that AF patients treated with rivaroxaban or warfarin presented increased levels of platelet-derived EVs compared with the control subjects with no AF. However, no differences in endothelial-derived EVs were noted [29]. Further improvement in this field may lead to the treatment individualization with EVs being potential predictors of treatment response in AF patients.
3. EVs Containing Nucleic Acids in Atrial Fibrillation Patients
Wang et al. investigated EVs containing micro-ribonucleic acids (miRs). They proved that patients suffering from non-valvular AF presented increased levels of miR-483-5p and decreased levels of miR-142-5p, miR-223-3p, and miR-223-5p compared with controls in sinus rhythm. Moreover, miR-483-5p, miR-142-5p, and miR-223-3p were shown to be related to AF by univariate logistic analysis, whereas multivariate logistic analyses proved miR-483-5p to be independently correlated with AF [30]. Mun et al. researched differences in the expression of miRs in circulating EVs between subjects with supraventricular tachycardia and patients suffering from persistent AF. The study revealed that the latter group presented increased levels of miR-107, miR-320d, miR-103a-3p, miR-486-5p, and let-7b-5p [31]. Soltész et al. proved that there were no differences in the EV-contained mitochondrial deoxyribonucleic acid (mtDNA) copy numbers between AF patients and healthy controls [32]. Additionally, Wei et al. demonstrated that AF patients had increased levels of miR-92b-3p, miR-1306-5p, and miR-let-7b-3p contained in the EVs compared with control patients in sinus rhythm [33].
Liu et al. found that patients suffering from congenital heart disease (CHD) and AF presented different concentrations of miRs associated with EVs when compared with CHD patients in sinus rhythm. Quantitative analysis showed reduced levels of miR-382-3p and miR-450a-2-3p as well as increased levels of miR-3126-5p in AF patients [34]. Wang et al. showed that AF patients had higher expression of EV-contained miR-107 compared with healthy controls [35].
Interestingly, Liu et al. demonstrated that AF patients presented decreased expression levels of EV-incorporated LINC00636 (Long Intergenic Non-Protein Coding RNA) and miR-450a-2-3p compared with non-AF patients. Moreover, the expression levels of these two RNAs positively correlated with each other [36]. Importantly, Chen et al. proved that AF patients showed an increased expression of myocardial infarction associated transcript (MIAT) in serum-derived EVs when compared with healthy individuals. Interestingly, the highest MIAT expression was observed in patients with permanent AF. It was also evidenced that MIAT, abundant in those EVs, promoted atrial fibrosis and thus compounded atrial remodeling and subsequent AF [37].
Siwaponanan et al. evidenced that AF patients presented increased levels of miR-106b-3p, miR-590-5p, miR-339-3p, miR-378-3p, miR-328-3p, and miR-532-3p derived from EVs. These miRs were suggested to be possibly involved in processes such as arrhythmogenesis or structural remodeling in AF [38]. Similarly, Zhu et al. investigated EV-contained miRs expression levels in AF patients. They presented an increase in miR-124-3p, miR-378d, miR-2110, and miR-3180-3p levels as well as a decrease in miR-223-5p, miR-574-3p, miR-125a-3p, and miR-1299 levels when compared with patients in sinus rhythm [39]. Finally, Mun et al. proved that patients with persistent AF showed a significant downregulation of miR-30a-5p in small EVs [40]. Just as EVs alone, miRs and other small molecules contained in EVs can become not only diagnostic but also predictive tools.
4. EVs in Atrial Fibrillation Patients Undergoing Ablation or Other Invasive Procedures
Herrera-Siklódy et al. studied the differences between AF patients undergoing cryoablation and radiofrequency (RF) ablation in terms of EVs as cellular damage markers. In both groups of patients, they observed an increase in platelet- and leukocyte-derived (but not endothelial-derived) EVs after the ablation procedure. However, there were no significant differences between the groups [41]. Jesel et al. compared the concentrations of EVs between the right and the left atria in AF patients undergoing ablation. They investigated procoagulant EVs derived from platelets, leukocytes, and endothelial cells. Interestingly, only endothelial-derived EVs presented atrial-specific differences, being increased in the right atrium [42]. Liles et al. measured the levels of tissue-factor extracellular vesicles (TF-EVs) in non-valvular AF patients prior to ablation surgery. They compared patients and healthy controls and divided patients based on the type of their anticoagulant therapy. It was shown that TF-EVs were increased in AF patients compared with healthy controls; however, after dividing AF patients into two groups, not-treated with anticoagulants and treated with anticoagulants, only the latter showed increased levels of TF-EVs compared with healthy controls. Consistently, this group also presented increased levels of TF-EVs compared with the first group. Interestingly, there were no differences in TF-EV levels between AF patients treated with warfarin and AF patients treated with apixaban or rivaroxaban [43]. Pourtau et al. proved the diminished tissue-factor-dependent procoagulant activity of EVs in both paroxysmal and persistent AF patients undergoing ablation compared with healthy controls; however, only the paroxysmal AF patients showed decreased fibrinolytic activity of EVs compared with controls. Moreover, 10 AF patients in sinus rhythm (for 10 days before ablation) were subjected to induced AF. After 20 minutes of acute AF, these patients presented decreased procoagulant activity of EVs with unaltered fibrinolytic activity [44].
Meng et al. demonstrated that AF patients had elevated levels of TF-EVs and EVs derived from platelets, endothelial cells, and leukocytes (but not from erythrocytes) compared with healthy controls. It was also proven that both endothelial-derived EVs (>355/μL) as well as leukocyte-derived EVs (>639/μL) were risk factors for the early recurrence of atrial fibrillation (ERAF). Additionally, the former were shown to be an independent predictor of the ERAF [45].
Mørk et al. analyzed EVs (particularly TF-EVs) in patients with or without AF undergoing cardiac surgery procedures. Total EVs, as well as TF-EVs, were shown to be increased in patients suffering from AF in all measurements, from venous blood preoperatively/intraoperatively and directly from the left atrial appendage intraoperatively [46]. Amabile et al. showed that non-valvular AF patients who underwent left atrial appendage occlusion presented increased levels of annexin V-positive, and platelet-, erythrocyte-, and leukocyte-derived EVs after the intervention. In patients undergoing coronary angiography, who served as a control group, only annexin V-positive EVs were proven to be increased after the procedure [47]. Shaihov-Teper et al. investigated the population of patients with or without AF undergoing elective heart surgery. Organ cultures, grown from epicardial fat, secreted more EVs in samples from AF patients. Moreover, EV contents, proinflammatory and profibrotic cytokines as well as profibrotic miR, were also elevated in this group [48]. Perhaps ongoing and future research will provide evidence that will lead to the EVs’ inclusion into the qualification criteria for invasive procedures such as ablation.
5. Other Research Studies Concerning EVs in Atrial Fibrillation Patients
Choudhury et al. proved that both patients suffering from AF and patients in sinus rhythm suffering from other cardiovascular diseases had increased levels of platelet EVs compared with healthy controls in sinus rhythm. Moreover, they evidenced that neither AF type (paroxysmal or permanent) nor applied therapy (aspirin or warfarin) influenced the level of platelet EVs [49]. Ederhy et al. showed increased levels of annexin V-positive EVs in AF patients compared with control subjects with or without cardiovascular risk factors. The level of platelet- and endothelial-derived EVs showed no differences between AF patients and control subjects with cardiovascular risk factors; however, they were increased in those two groups as compared with control subjects without cardiovascular risk factors [50]. Azzam et al. proved that patients suffering from valvular AF had increased levels of platelet-derived EVs compared with age-matched healthy volunteers in sinus rhythm. Moreover, it appeared that the severity of mitral stenosis correlated with EV levels [51].
Wang et al. investigated non-valvular AF patients, both with paroxysmal AF and persistent AF. It emerged that the latter group had increased levels of EVs compared with normal controls and paroxysmal AF patients. What is more interesting is it was shown that patients with persistent AF had increased levels of EV-bound interleukin-1β and P-selectin [52]. Hayashi et al. compared the levels of P-selectin-positive EVs in platelet-rich plasma between non-valvular AF patients and control subjects; there were no differences between these groups. However, they proved that the induction of AF in paroxysmal AF patients resulted in increased levels of EVs expressing P-selectin [53]. Idriss et al. proved that both mitral valve disease (MVD) patients with AF and MVD patients in sinus rhythm had increased levels of EVs showing positive binding to anti-CD41a as compared with healthy controls; however, there were no differences between these two groups of MVD patients [54].
Wang et al. studied non-valvular AF patients with or without left atrial thrombi. Both groups showed increased phosphatidyl-serine (PS)-exposing EV levels compared with control subjects; moreover, the patients with thrombi had elevated EV levels compared with the patients without thrombi. Both groups presented an increased procoagulant activity to be effectively inhibited by the addition of lactadherin. Interestingly, the amount of EVs positively correlated with the thrombus diameter [55]. Siwaponanan et al. demonstrated that non-valvular AF patients had increased levels of total EVs and increased levels of platelet- and endothelial-derived EVs compared with healthy controls [56].
Thulin et al. investigated AF patients (some of whom were stroke cases) selected from a large randomized clinical trial and a cohort of the randomly selected control individuals of age 70. It was shown that AF patients presented increased levels of PS-positive EVs and EVs derived from platelets, leukocytes, and erythrocytes (but not from endothelial cells) compared with controls. Moreover, there were no differences in the EV levels among the AF patients when comparing the stroke cases to the others [57]. Wang et al. classified non-valvular AF patients as “low to moderate risk” or “high risk” of stroke using the CHADS2 score. The latter group was evidenced to have increased levels of annexin V-positive and platelet-derived EVs as compared with the lower-risk group. Moreover, it was shown that EVs derived from AF patients bound to platelet receptor CD36 and activated platelets [58].
Voukalis et al. evidenced that AF patients presented increased levels of apoptotic EVs (annexin V-positive) when compared with ischemic disease patients in sinus rhythm; however, both groups had similar levels of platelet-derived EVs [59]. Ni et al. conducted a proteomic analysis of serum EVs comparing paroxysmal AF patients with healthy subjects. These two groups were proven to have different expression levels of many proteins mainly involved in anticoagulation, complement system, and protein folding, as indicated by the bioinformatic analysis [60]. Zietzer et al. proved that patients suffering from AF had higher levels of large EVs derived from platelets in the left atrial appendage than patients with no AF. Moreover, patients with permanent AF presented higher levels of these EVs when compared with non-permanent AF patients [61].
This entry is adapted from the peer-reviewed paper 10.3390/ijms23147591
This entry is offline, you can click here to edit this entry!
