Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Cell Biology
Atypically shaped cardiomyocytes (ACMs) are found in cultures of the cardiomyocyte-removed fraction obtained from cardiac ventricles from neonatal to aged mice. ACMs are thought to be a subpopulation of cardiomyocytes or immature cardiomyocytes, most closely resembling cardiomyocytes due to their spontaneous beating, well-organized sarcomere and the expression of cardiac-specific proteins, including some fetal cardiac gene proteins.
- atypically shaped cardiomyocytes
- ACMs
- subpopulation of cardiomyocytes
- spontaneous beating
- ischemic resistance
- cell fusion
1. Introduction
The mammalian heart is one of the organs with a low regeneration capacity after birth [1,2]. In the development stage, embryonic cardiomyocytes arise from the early cardiac progenitors or the proliferation of pre-existing cardiomyocytes [3]. Neonatal cardiomyocytes undergo additional rounds of DNA synthesis without cytokinesis, resulting in the binucleation or multinucleation shortly after birth [4], and have transient regeneration potential during this period [5]. In the adult heart, a number of studies have reported evidence to support the notion that the pre-existing cardiomyocytes are capable of re-entering the cell cycle in both the human and mouse heart [6,7,8,9,10], the rate and degree of cardiomyocyte renewal under both physiological and pathophysiological conditions are far too small; thus, dead cells are not substantially replaced by renewed cells [11,12]. In the mouse heart, the turnover of cells through the proliferation of resident cardiomyocytes is estimated to occur at a rate of approximately 1.3–4% per year, whereas in the human heart, the annual turnover rate of cardiomyocytes is observed to gradually decrease from 1% at 25 years of age to 0.45% at 75 years of age; thus, the rate of cardiomyocyte exchange in adulthood is <1% per year [6,13].
Following myocardial infarction, the heart loses approximately 25% of the cardiomyocytes within a few hours [14]; however, it is estimated that <0.1% of cardiomyocytes re-enter the cell cycle [15]. At present, the “proliferative activity” of the postnatal mammalian heart is thought to be limited to the process of multinucleation and polyploidization, which occurs in the early postnatal period and in the failing heart [12]. Under pathophysiological conditions, active cardiomyocyte proliferation to cardiac hypertrophy has been reported based on an autopsy of patients with LEOPARS syndrome [16]. One of the most effective tools for understanding the mechanism of binucleation, polyploidization and cell-cycle arrest of cardiomyocytes is now thought to be a model system using induced pluripotent stem cells (iPSCs) that reproduces the essential factors in the heart [17]. In addition, the upregulation of resident or bone marrow-derived progenitor cells has been reported to give rise to cardiomyocytes for repairing the heart [18,19,20,21,22,23,24,25].
As the regulation of cardiomyocyte regeneration has been one of the most important themes in clinical research, a number of studies have attempted to manipulate endogenous progenitor cells to induce differentiation into functional cardiomyocytes. The first adult resident cardiac stem cells were identified by the expression of stem cell receptor kinase (c-kit) but not blood lineage markers (Lin), c-kit+/Lin− cells, in 2003 [26]. Thereafter, the identification of cardiac stem or progenitor cells based on characteristics such as the expression of stem cell antigen-1 (Sca-1) [27,28] and LIM-homeobox transcription factor (islet 1) [29] and the ability to exclude Hoechst 33342 dye [30], has been reported. During this period, these cells were demonstrated to differentiate into cardiomyocytes in vitro in response to hormones or chemicals, such as 5′-azacytidine [27,28], oxytocin [28,30] and trichostatin A [30]. Adult cardiac stem cells isolated by c-kit+/Lin− selection have been shown to more systematically give rise to cardiomyocytes cultured in leukemia inhibitory factor (LIF)-deprived basic differentiation medium supplemented with several chemicals in sequence, including oxytocin and activin A [31]. Negative views have also been reported, with one review reporting that no reliable data have shown the existence of cardiomyocyte-differentiable stem cells in the adult heart that might be used in practical therapeutics to repair the injured myocardium [32]. Although there are still some limitations that hinder cell therapy using cardiac stem or progenitor cells, the methodology is constantly being innovated, with methods such as proteomic analyses of cardiac progenitor cells, including cells isolated based on surface-marker selection, differentiated human embryonic stem cells (ESCs) and iPSCs [33], and the 3D structure applications composed of cardiac and endothelial progenitor cells [34]. These methods have been accelerated with the aim of translation into cell therapy [1,2].
2. Atypically Shaped Cardiomyocytes (ACMs)
The isolation of cardiomyocytes is performed via coronary perfusion of the whole heart with enzymes using either the retrograde [97] or antegrade [36,98] perfusion method, and the cardiomyocyte-depleted fraction including interstitial heart cells of various cell lineages can then be cultured in semi-solid culture medium. After tightly adhering to the bottom of the appropriate dish, the cells grow over several days and start spontaneously beating. Given its peculiar morphology (Figure 1), we named these cells ACMs [35]. ACMs are also observed in the cell culture with a commonly used liquid culture medium [35], but the number of ACMs, especially beating cells, is extremely low. These beating cells have occasionally been observed as distorted or unusual cells present in culture dishes of isolated cardiomyocytes, where they have not received particular attention [36,37]. Observations indicate that 3D culture is a better condition for the development of these cells in comparison to two-dimensional (2D) culture with a liquid culture medium, which is considered one reason why these cells have not received much attention thus far.
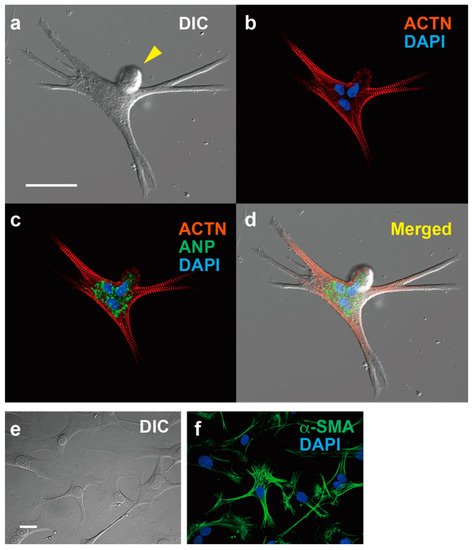
Figure 1. Immunofluorescent microscopy of ACM and cardiac fibroblasts. expressing ACTN and ANP, and cardiac fibroblasts expressing α-SMA. (a–d) ACM, bar, 50 µm. (a) Differential interference contrast image (DIC). (b) Immunostaining for α-actinin (ACTN, red) and DAPI staining for nuclei (blue). (c) Merged image for ACTN, DAPI and atrial natriuretic peptide (ANP, green). (d) Merged images for (a–c). (e,f) Cardiac fibroblasts, bar, 50 µm. (e) DIC. (f) Immunostaining for α-smooth muscle actin (α-SMA) and DAPI staining.
ACMs can be detected in cultures prepared from neonatal to aged mice without showing appreciable proliferation during long-term culturing [39]. The data thus indicate that ACMs survive in the heart for a life-long period but lack a self-renewing or clonogenic ability. A few days after plating, ACMs already show the automaticity and express characteristic proteins for ventricular and atrial myocytes, SA nodal pacemaker cells and fetal cardiac cells, indicating that the cells undergo the differentiation process to become cardiomyocytes as opposed to having multipotency. Therefore—at least based on the present data—it is unlikely that these would be classified as progenitor cells; rather, they would be classified as a subpopulation of cardiomyocytes or immature cardiomyocytes.
3. Characteristics of ACMs
3.1. Peculiar Morphology
One of the most obvious characteristics of ACMs, in addition to their spontaneous contracting activity, is that the cell shapes are markedly different from those of normal rod-shaped cardiac ventricular myocytes (Figure 1). ACMs possess a spherical shape at the start of culture, but after a few days of culture, they show peculiar shapes with many branches and/or protrusions, and most possess multiple nuclei with bulge(s) on the cell surface (Figure 1). However, while the cell shapes are complicated, the sarcomere structures are well organized and regularly arranged up to the branched tips [35,36,37]. The protrusions of ACMs not only come out horizontally, touching the bottom of the culture dish, but also grow three-dimensionally; thus, these cells are thicker than the proliferating fibroblast-like cells observed in the same culture dish, indicating that the cytoplasm is enriched in the contractile proteins. As the tight adherence of the plasma membrane to the culture dish may be a limitation to forming cells, the cell shapes in the heart tissues are not clear.
3.2. Automaticity
In most beating ACMs, the rhythmic action potentials are recorded that are reversibly suppressed by acetylcholine [35], while isoproterenol also shortens the peak intervals of the spontaneous Ca2+ transient in ACMs [99]. These findings are similar to the cell responses detected in sino-atrial (SA) node pacemaker cells [100,101], showing that the receptors and signal induction molecules for autonomic nervous systems function properly in ACMs. Unlike SA node pacemaker cells, ACMs often exhibit abnormal electrical automaticity caused by the repeated events of marked hyperpolarization to some extent and the subsequent depolarization. These arrhythmic events occur naturally, and the frequency varies from cell to cell.
It would be interesting to learn whether or not ACMs residing in the heart show automaticity under both physiological and pathophysiological conditions. The heart possesses a highly specialized system for generating rhythmic impulses to cause rhythmic contraction of the cardiomyocytes and for conducting these impulses rapidly throughout the heart. The electrical coupling within cardiomyocytes in ventricles is facilitated by gap junctions mainly composed of connexin 43 (Cx43) localized at the intercalated discs, whereas SA nodal cells do not express this type of gap junction proteins [102,103]. The expression of Cx43 in ACMs is low and particularly detected in the peri-nuclear area at the beginning of the culture before gradually increasing and spreading towards the cell periphery from five to eight days of culture along with the morphological maturation, confirmed by the expression of contractile protein [104]. Similar observations have been reported in which changes in the distribution of Cx43 in cardiomyocytes are observed in both cultured cells [105] and also in the myocardium of individuals with compensated and decompensated cardiac hypertrophy [106]. In addition, ACMs show an average maximal diastolic potential of around −65 mV [35], while the resting membrane potential in the isolated ventricular myocytes obtained from adult mice using our preparation method is approximately −74 mV on average [107], suggesting that the ACMs are not likely to electrically stimulate neighboring cardiomyocytes. These data suggest that the small native ACMs resident in the interstitial spaces have no—or very small—effects on the ventricular myocytes, at least in a healthy heart.
3.3. Protein Expression
While ACMs are small cells, with a diameter of approximately 10 µm immediately after isolation from the adult cardiac ventricular tissues, the large amounts of contractile proteins, such as α-actinin (ACTN) (Figure 1) and cardiac troponin T (cTnT), are synthesized within several days to help them increase their length more than 10-fold. Interestingly, ACMs, isolated from cardiac ventricular tissues, typically express hyperpolarization-activated cyclic nucleotide-gated channel 4 (HCN4), T-type voltage-gated Ca2+ channel (CaV3.2), and atrial natriuretic peptide (ANP). It should be noted that these proteins are not functionally expressed in normal adult ventricles and are referred to as fetal cardiac gene proteins.
Adult cardiac stem cells, which were originally found in the c-kit+/Lin− cardiac cells subpopulation, possessing the characteristics of self-renewal, clonogenicity and multipotency, can regenerate functional myocardium in vivo [26]. Eliminating cells expressing endothelial and hematopoietic markers, such as CD31 and CD45, has been imperative for the isolation of cardiac stem cells from the heart [31,79]. ACMs do not show appreciable proliferation during long-term culturing and simultaneously express characteristic proteins of ventricular and atrial myocytes, SA nodal pacemaker cells and fetal cardiac cells, suggesting that these cells have different properties from cardiac stem cells or stem cells of other types. As expected, typical stem cell surface markers, Sca-1, c-kit, hematopoietic stem cell marker (CD34), platelet-endothelial adhesion molecule-1 (CD31) and vascular endothelial cell growth factor receptor 2 (Flk-1), are absent in ACMs. The evidence suggests that ACMs should not be classified as stem or progenitor cells that can undergo the differentiation process.
3.4. Ischemic Tolerance
Since ACMs are cultured in a methylcellulose-based semi-solid medium, it is more difficult to perform medium exchange than with a liquid medium, so a small droplet of the liquid medium is added from time to time during long-term culture. However, the proliferation of fibroblasts renders the culture condition an acidic one of chronic malnutrition. Surprisingly, ACMs in a medium that has turned a yellowish-orange color continue contracting rhythmically despite the harsh culture environment for over one month. Furthermore, another important feature of ACMs during long-term culture is that they fuse with each other while maintaining spontaneous contraction.
Cardiomyocytes are highly sensitive to hypoxia; for example, in the human heart, ventricular myocytes become irreversibly damaged approximately 30 min after blood flow stops [68,71]. Following the reestablishment of the blood flow, the reperfusion of the coronary artery paradoxically causes further—occasionally lethal—damage to the heart and as well as a wide range of organs [108]. ACMs can survive these lethal ischemic conditions by blocking airflow by covering the cell suspension with oil [109], with half of the cells subsequently able to develop into beating cells, while approximately 85% of ventricular myocytes die within 90 min [99]. ACMs have thus been shown to possess ischemic resistance in addition to resistance to malnutrition and acidic conditions, suggesting that these cells may survive after cardiomyocytes die in injured hearts. The finding that ACMs (Prp+/cTnT+ cells, as stated in Section 6) survived in the peripheral area of infarction in pathological heart tissue specimens obtained from the patients who had a myocardial infarction [104] supports this view.
3.5. Constitutively Active Autophagy
Autophagy is an evolutionally conserved process for the degradation of long-lived and/or damaged proteins and organelles occurring in cells throughout the body [110,111,112] and during the neonatal period in particular, thus providing a necessary source of energy in various tissues [113]. Under physiological conditions, the autophagy activity in the heart remains low, aiding in the maintenance of the cell components, and is rapidly activated under pathophysiological conditions to support cardio-protection [114,115,116,117,118,119]. However, during the only early neonatal starvation period, autophagy in the heart is known to be activated [113].
In contrast, autophagy is constitutively activated in ACMs, not only to support cellular functions, but it also plays an essential role in the development of beating cells in the culture [99]. Constitutively active autophagy is thought to enable ACMs to rapidly synthesize proteins to grow into large beating cells and to continue beating in harsh environments by providing a source of energy.
3.6. Multinucleation and Cell Fusion
The most obvious characteristic of ACMs is that approximately 76% of these cells have multiple nuclei (Figure 1), sometimes more than four [38]. In mice, the majority of cardiomyocytes undergo additional DNA synthesis without cytokinesis within approximately 14 days after birth, resulting in multinucleation [3,12]. However, we have not observed such nuclear fission in ACMs during culturing; thus, one possible explanation for the multiple nuclei of ACMs is that cells fuse with each other, whether it occurs in vivo or after culturing.
“Native ACMs” that are resident in the heart tissues (as stated in Section 6) have often been observed as clusters [38], potentially resulting in the formation of fused cells with plural nuclei through the cell preparation procedure. Among the various interstitial cells that exist in the culture dish, ACMs are only able to fuse with the same type of cell [38]. When other types of cells are attached, ACMs pull the cell membrane along while beating, but they do not fuse with any cells other than ACMs [99]. These phenomena indicate that ACMs can only fuse with cells that have a cell membrane with the same membrane components, leading to the hypothesis that cardiomyocytes are indeed candidates for fusion with ACMs. Unfortunately, the coculture of ACMs and ventricular myocytes has not succeeded because isolated ventricular myocytes cannot survive in culture while ACMs settle at the bottom of the culture dish and grow. Some ACMs are observed to closely contact with ventricular myocytes but not attach, and then ventricular myocytes shrink and die over time. Therefore, the behavior of native ACMs should be explored in the future.
This entry is adapted from the peer-reviewed paper 10.3390/biom12070896
This entry is offline, you can click here to edit this entry!
