Pancreatic cancer is the fourth leading cause of cancer-related mortality worldwide, with a five-year survival rate of less than 8% [1]. It can be classed into endocrine and exocrine tumours with PDAC, a form of exocrine pancreatic cancer, the most common form. The high mortality rate associated with PDAC is primarily due to delayed diagnosis and tumour resistance to chemotherapy [2]. A broad range of non-specific symptoms are associated with PDAC such as abdominal pain, jaundice, dry/itchy skin, steatorrhoea, and bilirubinuria. Surgery is the primary treatment option, with chemotherapy being administered as adjuvant therapy in select cases. Resistance to chemotherapy has become a critical problem in the treatment of PDAC, with most patients displaying resistance patterns [10].
1. Current Approved Therapies
Chemotherapy
Currently, chemotherapy is the main form of treatment for unresectable PDAC tumours [
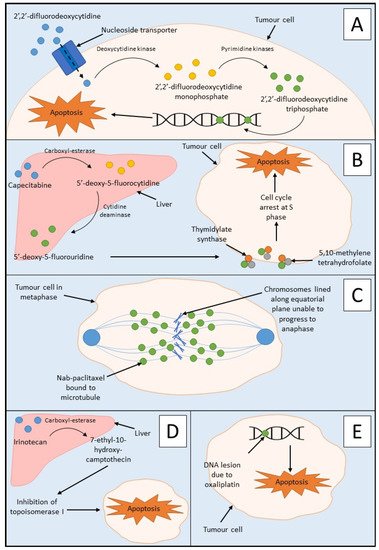
21]. More commonly known as gemcitabine, 2′,2′-difluorodeoxycytidine is an antimetabolite drug that inhibits DNA synthesis during the S phase of the cell cycle (
Figure 1A) [
22]. Gemcitabine is utilised as mono- or combination therapy (with capecitabine or albumin-bound nanoparticle paclitaxel (nab-paclitaxel)) in the treatment strategies of several stages of PDAC including locally advanced PDAC, metastatic PDAC, and as adjuvant therapy in resectable cases [
8]. Treatment with gemcitabine alone yields dismal results with progression-free survival (PFS) of 3.9 months (95% CI, 3.0–5.1) and overall survival (OS) of 9.2 months (95% CI, 8.3–10.4) [
23].
Figure 1. Mechanism of action of PDAC chemotherapies: (A) the mechanism of action of gemcitabine showing administration of prodrug 2′,2′-difluorodeoxycytidine, conversion to 2′,2′-difluorodeoxycytidine monophosphate, and 2′,2′-difluorodeoxycytidine triphosphate, respectively leading to incorporation into DNA and apoptosis of the tumour cell; (B) mechanism of action of capecitabine showing its metabolism to 5′-deoxy-5-fluorocytidine by carboxyl-esterase in the liver. This is further metabolised to 5′-deoxy-5′-fluorouridine by cytidine deaminase in both the liver and the tumour. 5′-deoxy-5′-fluorouridine inhibits thymidylate synthase by forming a ternary complex with thymidylate synthase and 5,10-methylenetetrahydrofolate. The formation of thymidine is stopped by the inhibition of thymidylate synthase, and therefore, DNA synthesis is blocked in S phase of the cell cycle; (C) mechanism of action of nab-paclitaxel showing the binding of paclitaxel to the tubulin beta-subunit of the microtubules. This leads to the inability of the chromosomes to separate resulting in the inhibition of mitosis of the tumour cell and inevitably apoptosis; (D) mechanism of action of irinotecan through administration of the camptothecin-derivative prodrug. Carboxyl-esterase in the liver converts irinotecan to its active form, 7-ethyl-10-hydroxy-camptothecin, which causes impaired DNA synthesis via the inhibition of topoisomerase I preventing the removal of torsional stress. This then leads to a double-stranded DNA break, ultimately leading to cell death; (E) mechanism of action of oxaliplatin showing the induction of apoptosis of tumour cells due to DNA damage via DNA lesions which leads to the inhibition of both DNA and messenger RNA.
Capecitabine is an antimetabolite chemotherapeutic agent utilised in the treatment of PDAC [
24]. It is administered as a pre-prodrug of 5-fluorouracil and is, therefore, an antimetabolite drug which inhibits thymidylate synthase (
Figure 1B) [
24,
25]. Capecitabine may be used in combination with gemcitabine as adjuvant therapy in resectable PDAC if tolerated by the patient and may also be used in combination with radiotherapy for locally advanced unresectable PDAC cases [
8]. A combination of stereotactic body radiation therapy, gemcitabine, and capecitabine yielded a PFS of 12 months (95% CI, 8.34–15.66) and an OS of 19 months (95% CI, 14.6–23.4) [
26].
Nab-paclitaxel is another drug that is utilised in the treatment of metastatic PDAC in combination with gemcitabine if FOLFIRNOX is not tolerated by the patient [
8]. Paclitaxel is a chemotherapeutic agent that causes cell death by interfering with microtubule function during mitosis (
Figure 1C) [
27]. Combination treatment of gemcitabine and nab-paclitaxel yielded a PFS with a median value of 6.7 months (95% CI, 6.0–8.0) and a median OS of 10 months (95% CI, 7.9–12.1) [
28].
Another form of chemotherapy, FOLFIRINOX, is a combination therapy consisting of 5-fluorouracil, folinic acid, oxaliplatin, and irinotecan, and is used in the first-line treatment of metastatic PDAC [
8,
29]. Furthermore, 5-fluorourcail is an antimetabolite drug which inhibits thymidylate synthase, and this reaction is stabilised by folinic acid [
25]. The mechanism of action of 5-fluorouracil is similar to that of capecitabine in the latter stages (from 5′-deoxy-5-fluorouradine), as seen in
Figure 1B. Irinotecan is a derivative of camptothecin which causes impaired DNA synthesis via the inhibition of topoisomerase I (
Figure 1D) [
29]. Oxaliplatin is an alkylating chemotherapeutic drug which induces apoptosis of tumour cells due to DNA damage via DNA lesions, leading to the inhibition of both DNA and messenger RNA (
Figure 1E) [
29]. FOLFIRINOX remains a valuable treatment option for PDAC, with a median PFS of 13.6 months (95% CI, 11.3–15.9) and a median OS of 35.4 months (95% CI, 23.8–45.0) [
30].
2. Targeted Therapeutic Approaches
2.1. Synthetic Lethality
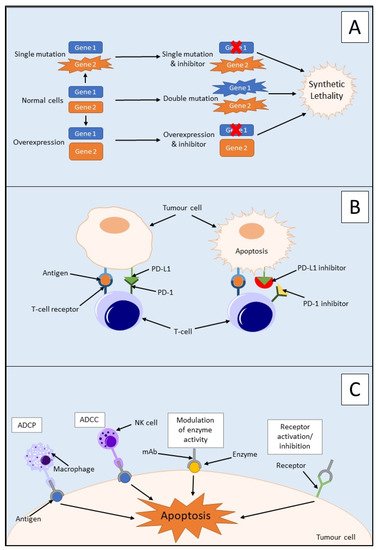
Synthetic lethality is used to define an interaction between two genes in which a mutation of one is viable; however, a mutation of both leads to cell death, as outlined in
Figure 2A [
31,
32]. It can also involve a mutation only being synthetically lethal if it is combined with another specific mutation. These synthetically lethal interactions can be described as gain-of-function alleles or loss-of-function alleles, with the most common being the latter [
33]. Loss-of-function alleles can be categorised based on their protein product′s function; for example, they could have an essential function, be a subunit of a protein complex, or play a role in protein folding pathways. Synthetic lethality has proven successful in the treatment of
BRCA1/2-mutated neoplasms which are sensitive to poly(ADP-ribose) polymerase (PARP) inhibitors [
34]. PARP is an enzyme which is involved in the repair of single-strand DNA breaks (SSBs) [
32]. Inhibition of PARP will lead to irreparable SSBs and, therefore, a one-ended double-stranded DNA break (DSB) via the collapse of a replication fork. Neoplasms containing a loss-of-function mutation of either the
BRCA1 or
BRCA2 gene lack homologous recombination; therefore, DSB results in cell death [
32]. Due to this aspect, synthetic lethality is believed to be a possible route for potential anticancer drugs in the treatment of PDAC via the proteins produced by potential synthetically lethal genes with mutations [
33]. However, commonly occurring loss-of-function mutations in PDAC such as those in
CDKN2A,
TP53, and
SMAD4 are currently not targetable due to the many genetic aberrations, mainly point mutations, associated with each gene [
35].
Figure 2. Mechanism of action of three PDAC immunotherapies: (A) the mechanism of synthetic lethality showing normal cells, single mutation, or overexpression of one gene is viable for a cell but inhibition of one gene and mutation in the other, a double mutation, or overexpression of one gene and inhibition of the other leads to cell death via cell viability; (B) mechanism of action of immune checkpoint inhibitors, for example, PD-1 and PD-L1. Binding of PD-1 and PD-L1 inhibits activation of T cells. Upregulation of both PD-1 and PD-L1 in tumour cells makes them an ideal target for inhibition leading to the activation of T cells; (C) mechanism of action of monoclonal antibodies (mAbs) in cancer treatment. mAbs may be used to target different molecules in the treatment of cancer, for example, receptors, antigens, or enzymes. Receptors on macrophages may target Fc portions of antigen-bound mAb and engulf tumour cells through antibody-dependent cellular phagocytosis (ADCP). Receptors on natural killer (NK) cells may also target Fc portions of antigen-bound mAb and imitate antibody-dependent cellular cytotoxicity (ADCC).
2.2. Immunotherapy
With the issue of growing resistance to current PDAC treatments, new and more targeted therapies are required to improve the prognosis of patients. As previously mentioned, the TME plays a major role in intrinsic resistance to chemotherapeutic drugs. Immunotherapy is the use of treatments and therapies that target and stimulate an immune response to combat cancer [
38]. There are several different forms of immunotherapy available such as the use of immune checkpoint inhibitors, monoclonal antibodies, adoptive cell transfer, and vaccination. Research into the use of these immunotherapeutic strategies for several different solid tumours, including PDAC, has increased over recent decades, due to its outstanding success in the past [
38]. With approximately 25% of breast cancer cases positive for human epithelial growth receptor 2 (HER2), the monoclonal antibody trastuzumab has forged a new path in the treatment of this malignancy [
39]. Another example is rituximab, an anti-CD20 monoclonal antibody that is a cornerstone drug in the treatment of B-cell malignancies such as non-Hodgkin lymphoma and chronic lymphocytic leukaemia [
40].
2.2.1. Immune Checkpoint Inhibitors
Immune checkpoint inhibitors are an immunotherapeutic strategy that activates the immune system to modulate the immune response to cancer [41]. This occurs through the stimulation of the innate and adaptive immune systems, with the main focus on the activation of T cells.
Programmed death-1 (PD-1) is an immune checkpoint protein that is activated by its ligand PD-L1 and is expressed by activated T cells [45]. PD-L1 is a membrane protein that is expressed on immune and tumour cells and inactivates T cells by inducing programmed cell death via heterodimer formation with CD80 [46,47]. Overexpression of PD-L1 has been detected in several cancers, including PDAC, and this overexpression is associated with advanced tumour stage and, therefore, a poorer prognosis for patients [45,48]. PD-L1 blockade alone has been shown to display minimal inhibition in PDAC and, therefore, is not regarded as a sufficient therapeutic target alone. This could be due to the non-immunogenic nature of PDAC or immunosuppression due to the high tumour burden [45].
Due to the poor success of immune checkpoint inhibitor monotherapy in PDAC, potential combination therapies are being sought to improve its efficacy. Cancer Forkhead box protein 3 (cFOXP3) is an upregulated protein in PDAC and plays a vital role with regulatory T cells and immune evasion in cancer [49]. It achieves this through the recruitment of cFOXP3 positive regulatory T cells to the site of malignancy via upregulation of C–C chemokine ligand 5 (CCL5). PD-L1 expression in PDAC has been shown to coexist with regulatory T-cell infiltration of tumours. This suggests a possible link between PD-L1 and cFOXP3 expression [49].
3.2.2. Monoclonal Antibodies
The four main mechanisms of action of monoclonal antibodies are outlined in
Figure 2C. There are several studies on monoclonal antibodies that could potentially bring new targeted therapies to the forefront of PDAC treatment and improve patient prognosis [
5]. In a study investigating monoclonal antibody pairs and their effect on monolayer BxPC-3 cells and CD1 nude mice injected with BxPC-3 cells, it was found that two strategies worked to combat PDAC in this animal model [
5]. The first strategy was the combination of two antibodies which were both specific to either epidermal growth factor receptor (EGFR) or HER2. This was described as a homo-combination of antibodies. The second was the combination of antibodies consisting of a pair of antibodies, one to EGFR and the other to HER2. This was described as a hetero-combination of antibodies. The homo-combination of antibodies yielded better results than the hetero-combinations at carrying out anticancer effects via the degradation of their respective receptor [
5].
3.2.3. Adoptive Cell Transfer
Adoptive cell transfer is the transfer of immune cells into a patient as a form of therapy to improve the patient’s immune system. The use of natural killer cells as a form of adoptive cell transfer therapy has recently become a point of interest in the field of immunotherapy [
56]. This is due to their ability to target and eliminate tumour cells via cytotoxic mechanisms and the role they play in inducing an adaptive immune response. In the pre-cancerous stages of PDAC, there is a loss of natural killer cells due to mutations in
KRAS. This could be due to their involvement in the initiation and progression of PDAC.
3.2.4. Therapeutic Vaccination
Any tumour cells remaining post-surgery/treatment could lead to a relapse of the PDAC tumour [
57]. Therefore, vaccination yields a possible approach to target remnant tumour cells via activation of the immune system toward tumour-associated antigens. The whole tumour cell lysate was utilised by processing murine PDAC tumour membranes to enable them to be opsonised by naturally occurring human IgG antibodies [
57]. This can stimulate the immune system to target tumour associated antigens, in this case, galactose-alpha-1,3-galactose (α-gal). An immune response was mounted against the PDAC tumour lysate vaccine, resulting in antitumour properties in murine models. A statistically significant median OS was observed with mice treated with PDAC tumour lysate and α-gal of 95.0 days (95% CI, 69–95), compared with the untreated control mice of 40.0 days (95% CI, 35–45) (
p < 0.01). This shows a potential route of treatment for PDAC which could be utilised in the future [
57].
3.3. Ongoing Clinical Trials
At present, there are a plethora of clinical trials recruiting patients that involve the treatment of PDAC. Many of these studies involve the utilisation of immunotherapies, in particular, monoclonal antibodies in combination with another form of therapy such as conventional chemotherapy. An example of this is a study currently recruiting in the Cancer Centre at Johns Hopkins University which aims to determine the effects of pembrolizumab which could be given in combination with defactinib in patients with resectable PDAC as a form of neoadjuvant or adjuvant therapy [
50]. Pembrolizumab is a monoclonal antibody directed towards PD-1, and this may or may not be administered intravenously alongside defactinib, a focal adhesion kinase inhibitor. Focal adhesion kinase is a non-receptor tyrosine kinase that is involved in cell scaffolding and signalling at the sites of integrin clustering on the cell membrane [
59]. The effects of these drugs will be determined in combination with standard neoadjuvant and adjuvant chemotherapy regimens such as gemcitabine [
50]. This study will determine if the tumour microenvironment can be reprogrammed via targeting focal adhesion kinase post-chemotherapy and, therefore, potentiate anti-PD-1 effects to halt cancer progression [
50].
This entry is adapted from the peer-reviewed paper 10.3390/cancers14102417