Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Subjects:
Pharmacology & Pharmacy
Deferiprone (L1) is an EMA- and FDA-approved drug used worldwide for the treatment of iron overload and also other conditions where there are no effective treatments. The multi-potent effects and high safety record of L1 in iron loaded and non-iron loaded categories of patients suggests that L1 could be developed as a “magic bullet” drug against COVID-19 and diseases of similar symptomatology.
- COVID-19
- SARS-CoV-2
- deferiprone
1. Introduction
A report by the World Health Organization (WHO) estimated that as of the end of February 2022, there have been globally about 0.5 billion confirmed cases of the coronavirus disease 2019 (COVID-19), including about 6 million deaths (according to another report, 18 million deaths) since the beginning of the pandemic [1,2]. It has also been estimated that more than 10 billion vaccine doses against the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) have been administered over the same period [1].
Different health strategies have been adopted in each country for controlling and reducing the morbidity and mortality associated with COVID-19, based on different priorities and aims at each stage of the progression of the pandemic, including transport restrictions, financial growth, educational and public health considerations for the treatment of other diseases, etc. [3].
The general strategy for curbing the COVID-19 pandemic is based on the prevention of transmission of SARS-CoV-2 and the identification and development of drug(s) and vaccines, which can decrease the mortality rate to minimum acceptable levels [3,4,5]. In this context, measures preventing transmission of SARS-CoV-2—such as self-isolation, distancing between individuals and face masks, as well as vaccinations and the administration of different drugs for supporting the prospects of survival in selected categories of seriously ill patients—have so far been the mainstay therapy for the limited control of the spread of the infection and therapeutic prospects for decreasing the rate of mortality [3,5,6,7,8,9].
However, despite the periodical improvements and therapeutic successes, COVID-19 is still here and is life threatening for the whole of humanity because of many unsettling factors such as the slow development and low availability of effective antiviral drugs and vaccines, limited effect of vaccinations, increased prospects of reinfection after vaccination, more emerging toxic SARS-CoV-2 variants and insufficient prophylaxis from viral transmission and toxicity [3,5,10,11,12,13].
There are many emerging challenges for the development of drugs targeting different aspects of COVID-19. These include the targeting of different stages of the disease, such as transmission and proliferation, ‘hyper-inflammation/cytokine storm’, lung damage and multi-organ damage and sepsis, long-term side effects and many others [3,5,8,9,14,15]. Drug targeting could mainly be focused on the respiratory system, which is the most affected and major cause of mortality by COVID-19, but also other systems which are affected at a different extent such as the cardiovascular, gastrointestinal, nervous, immune and hematopoietic systems [3,5,7,14,15]. Furthermore, drug targeting could be based on different categories of patients which are more susceptible to SARS-CoV-2 infection such as obese, renal, pulmonary, diabetic, immune-compromised and cardiovascular patients [3,7].
The development of specific drugs with effective targeting in each of the above categories could increase the prospects of a better outcome in the COVID-19 pandemic. In this context, there can be different strategies and approaches in the selection and evaluation process for new drugs against the disease [3,5,15]. One such strategy could be based on the identification of one drug for one target, another based on a multi-potent drug for many targets and also drug combinations for one or more targets [3,5]. The aim of any strategy is the selection of one drug or drugs for achieving a significant reduction in mortality in COVID-19 to acceptable levels; e.g., similar to the mortality rate caused by the influenza virus [3,4,5,16].
Several drugs are regularly used in different categories of COVID-19 patients, especially those suffering from pulmonary complications and hypoxia. For example, one such drug is remdesivir, which has broad spectrum antiviral activity and was initially used against the hepatitis C virus. Remdesivir is a pro-drug, which is metabolized to a ribonucleotide analogue inhibitor of viral RNA polymerase. In clinical studies remdesivir has been shown to cause a reduction in the rate of mortality of hypoxic COVID-19 patients [17,18,19,20]. Two other drugs widely used for treating COVID-19 patients are molnupiravir and paxlovid. Molnupiravir was initially developed to treat influenza and also recently licensed to prevent severe COVID-19 infection in patients [21,22]. It is a pro-drug of a synthetic nucleoside and exerts its antiviral action through introduction of copying errors during viral RNA replication. Oral molnupiravir appears to reduce the risk of hospitalization and death from COVID-19 by about 50% for newly diagnosed, high-risk patients [22]. Another antiviral co-packaged medication is a drug combination of nirmatrelvir and ritonavir, sold under the brand name paxlovid. It is used for the treatment of mild-to-moderate COVID-19 patients, who are at high risk for progression to severe COVID-19, including hospitalization or death. Oral paxlovid has been shown to reduce hospital admissions and deaths by 80–90% among patients with COVID-19 who are at high risk of severe illness [23]. The mode of action of nirmatrelvir is inhibition of the activity of the SARS-CoV-2-3CL protease, an enzyme that the coronavirus needs to replicate. Co-administration with ritonavir decreases the metabolism of nirmatrelvir and maintains its antiviral activity at higher levels [23]. Dexamethasone and other corticosteroids are also widely used in certain categories of patients for inhibiting the immune system, including cytokine response during hypoxia [24]. Progress in COVID-19 research has been very rapid, including development of antiviral drugs which are effective at the early phase, and also immune-modulating agents for treating cytokine storm [3,5,17,18,19,20,21,22,23].
In the meantime, there are thousands of drugs and nutraceuticals along with their combinations that can be used to select candidate therapeutics for targeting the transmission, proliferation and the fatal or severe symptoms of SARS-CoV-2 [3,5]. The development of more such drugs could reduce further the unacceptably high morbidity and mortality rate observed in the COVID-19 pandemic, as well as its associated newly identified long-term side effects and overall negative effects on daily life worldwide [3,24,25,26,27,28,29,30,31].
One such promising candidate drug against COVID-19 is deferiprone (L1), an iron chelating drug approved by the drug regulatory authorities, the FDA in the USA and EMA in the European Union, for the treatment of iron overload in thalassemia but has also been tested and shown to be effective in many other clinical conditions including viral infections (Figure 1) [3,32,33]. The drug was designed more than 40 years ago and tested in many in vitro, in vivo and clinical systems [3,32,33]. A detailed analysis of the clinical, pharmacological and other properties of L1 suggests that there may be an increased prospect for its use as a multi-potent drug against COVID-19 and also diseases with similar symptomatology.
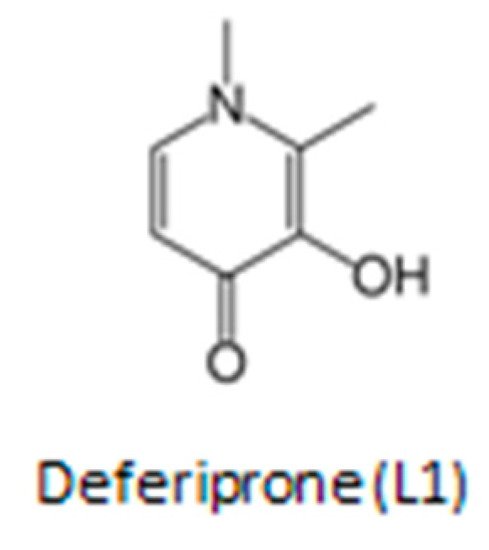
Figure 1. The chemical structure of the iron chelating drug deferiprone (L1). The drug is used mainly for the treatment of iron overload in thalassemia but also in many other diseases.
2. Pharmacological and Toxicological Considerations in the Use of Deferiprone against COVID-19
Drug selection against COVID-19 by the regulatory authorities is similar to that in many orphan drug development efforts, and in particular drug approval for emergency use in diseases where there are no available therapeutics [34]. Furthermore, the search for emergency drugs for the COVID-19 pandemic is considered urgent because of the rapid progress of the disease in different world regions and also the large number of the fatalities observed in aged and other susceptible categories of patients [3,5,6,7,8,35,36,37]. The prospect of the development of effective drugs for each of the different stages of COVID-19 is also challenging, since any drug targeting effectively one of the different targets or stages of the disease could potentially reduce the rate of mortality. Similarly, multi-targeting drugs such as L1 or drug combinations may further increase the prospects of mortality reduction in COVID-19.
Deferiprone is an EMA- and FDA-approved drug, which is listed by the WHO as one of the essential medicines (Figure 1). It has been used for more than 25 years by hundreds of thousands of patients worldwide for the treatment of transfusional iron overload in thalassemia and other conditions [32,33,34,38]. The general molecular characteristics, mechanisms of chelation, antioxidant, pharmacological, toxicological and other properties of L1 have been previously reviewed [32,33,34,38,39]. Deferiprone is an orally active, low molecular weight hydrophilic drug, which is on the top of the list of drugs with the highest safety record per dose and frequency of administration. It has been used in many non-iron loaded categories of patients in addition to iron overload categories with no significant toxicity [32,33,34,38,39]. Deferiprone can diffuse through almost all major organs where it can exert effectively its antiviral, antioxidant and other therapeutic effects [33,34,38,39].
The relatively short life cycle of SARS-CoV-2 and its associated life-threatening toxicity implications suggest that proposed therapeutic drugs against COVID-19 should exert their therapeutic activity in a matter of a few days or weeks [3,5]. The risk/benefit assessment for this short therapeutic time window can generally allow the administration of repeated high doses of L1 at the maximum dose of the approved range (50–100 mg/kg/day), similar to that in other non-iron loaded categories of patients. This short-term treatment period and the prior use of L1 in other categories of patients could potentially facilitate the rapid approval of drug trials and clinical use due to the emergency COVID-19 pandemic conditions, or other similar disease situations in the future [3,5,15,34].
2.1. Pharmacological Properties and Effects of Deferiprone
The pharmacological properties and other molecular characteristics of L1 have been under investigation in the past 40 years. Deferiprone is a small molecule of neutral charge, which is orally absorbed, widely distributed in most tissues and organs such as the heart, liver, spleen and the brain and is excreted almost completely in the urine [32,38,39]. It can also be monitored and measured in blood and also in saliva. Deferiprone can exert its therapeutic effects in most tissues, organs and cells as a result of its extensive tissue distribution. For example, L1 can enter most iron loaded tissues and mobilize excess iron by forming an iron complex of stoichiometry of three molecules of L1 to one molecule of iron. The iron complex of L1 has a red color similar to that excreted in the urines of iron loaded patients [32]. Although L1 has high affinity for iron, it can also bind other endogenous and xenobiotic metals including copper, zinc, aluminum, indium, plutonium, europium and uranium [40,41,42,43,44].
The pharmacokinetic and metabolic properties of L1 have been previously reported and some are shown in Table 1 [45,46,47,48]. Oral L1 is readily absorbed from the stomach, metabolized to a glucuronide conjugate in the liver, cleared from the plasma over a period of 6–8 h and excreted in the urine in three forms, namely the L1 iron complex, L1 glucuronide conjugate and free unconjugated L1 [38,45,46,47,48].
Table 1. Properties and mode of action of the chelating drug deferiprone.
| Chemical and physicochemical properties |
|---|
| Molecular weight: 139. Molecular weight of iron complex: 470. |
| Charge of L1 and iron complex at pH 7.4: neutral. |
| Partition coefficient (n-octanol/water): 0.19 (hydrophilic). |
| Stability constant (Log β) of deferiprone iron complex: 35. |
| Clinical and biological effects |
| Recommended dose in different categories of patients including combination with other chelating drugs: 10–100 mg/kg/day. |
| Effect of deferiprone on iron absorption: decrease of iron absorption. |
| Iron removal from diferric transferrin in iron loaded patients: removal of about 40% of iron at deferiprone concentrations of greater than 0.1 mM. Iron removal from ferritin and hemosiderin. |
| Differential iron removal from various organs of iron loaded patients: preferential iron removal of excess iron from the heart but also from liver, spleen and pancreas of iron loaded patients. Efficacy in iron removal is related to dose. |
| Iron redistribution in diseases of iron metabolism: Deferiprone can cause iron redistribution from iron deposits and also through transferrin from the reticuloendothelial system to the erythron in the anemia of chronic disease. Similar effects of excess iron redistribution is observed in patients with neurodegenerative diseases |
| Increase excretion of metals other than iron, e.g., zinc (Zn) and aluminum (Al): increased Zn excretion in iron loaded patients, following long-term treatments. Increase Al excretion in renal dialysis patients. |
| Iron mobilization and excretion of chelator metabolite iron complexes: no iron binding and no increase in iron excretion by the deferiprone glucuronide metabolite. |
| Combination chelation therapy: Combination therapies of all chelating drugs are more effective in iron excretion than monotherapies. The International Committee On Chelation of deferiprone and deferoxamine combination protocol causes normalization of the iron stores in thalassemia patients. |
| Metabolism and pharmacokinetics |
| Metabolite(s): The deferiprone−gluguronite conjugate is cleared through the urine but have no iron chelation properties. |
| T1/2 absorption of deferiprone: 0.7–32 min. T max of deferiprone: mostly within 1 h on empty stomach. |
| T1/2 elimination of deferiprone: 47–134 min at 35–71 mg/kg dose. |
| T1/2 elimination of the deferiprone iron complex: estimated within 47–134 min. |
| T max of the L1 iron complex: estimated within 1 h. T max of the metabolite deferiprone-glucuronide: 1–3 h. |
| Route of elimination of deferiprone and its iron complex: urine. |
The interactions of L1 with iron and other metal ions on the molecular level, proteins of iron metabolism, cells and tissues has also been extensively studied in vitro and in vivo. Iron chelation and mobilization by L1 has been shown to occur from all the iron pools in cells including intracellular low molecular weight iron, ferritin and hemosiderin and also from transferrin and non-transferrin bound iron (NTBI) in plasma. It has also been shown in clinical studies that the mobilization of iron by L1 depends in general on the iron load of the patients and the dose of L1 [38,46]. The increase of urinary iron excretion caused by L1 in non-iron loaded categories of patients is only a few mg, which is a small fraction in comparison to the amount of iron excreted in iron loaded patients [46]. The level of iron that could be excreted during L1 therapy in non-iron loaded patients, e.g., COVID-19 patients, is negligible and less than the amount of iron present in western diets or less than 1% of what is lost during blood donation. In this context it is expected that the amount of iron removed in COVID-19 patients during the short period of treatment, e.g., a week, can easily be replaced by dietary iron.
The body distribution of iron and mode of iron removal activity by L1 and other chelating drugs from iron loaded and non-iron loaded categories of patients, as well as the determination of the iron metabolic pathways involved in these processes, can be determined using different diagnostic techniques [49]. In particular, the recent introduction of the magnetic resonance imaging (MRI) T2 and T2* techniques have been instrumental for identifying the level and distribution of iron load in the heart, liver, spleen, brain and other organs [50,51,52,53,54]. Similarly, the same MRI methods have been used for monitoring the efficacy, specificity and safety levels of iron removal from different organs by L1 and other chelating drugs [55,56]. This information is vital for toxicity monitoring and also for designing therapeutic strategies for specific targets, as well as for personalized therapeutic protocols in iron overload diseases and also other diseases of focal iron deposits [52,56].
The high efficacy and low toxicity of L1 in the treatment of iron overload prompted investigations of its use and development in many other clinical conditions, especially in conditions with no other effective therapies such as neurodegenerative, cardiovascular, renal, infectious diseases, cancer, as well as all diseases associated with free radical pathology including ageing and also currently COVID-19 [3,5,34,57,58].
In each case, the strategic initiatives for the use of L1 in non-iron loaded diseases were based on the risk/benefit assessment of therapeutic outcomes in each of these diseases, where no other effective therapies are available. The same approach is also adopted for the proposed multi-target treatment of COVID-19 using L1.
2.2. Toxicological Aspects of Deferiprone Therapy
The safety of L1 has been studied over the past 40 years in different in vitro, in vivo and clinical models of short- and long-term toxicity [33,59,60]. Most importantly, the safety of L1 has been confirmed in different categories of patients following short- and long-term studies, as well as continuous clinical monitoring involving thousands of iron loaded patients and also other groups of non-iron loaded patients in the past 35 years [33,57,58,59,60]. The most serious toxic side effects observed during short- and long-term treatment in iron loaded thalassemia patients are agranulocytosis (1% >) and neutropenia (5% >). Both toxicities are reversible and weekly or fortnightly mandatory blood count monitoring is recommended for prophylaxis for all patients using L1. Less serious toxic side effects include musculoskeletal and joint pains, gastric intolerance and zinc deficiency [33,59,60].
Prophylactic measures and toxicity vigilance are usually necessary and implemented for monitoring the safety of L1 and also of other drugs during long-term treatments. In this context, mandatory monitoring of weekly white blood cell count is considered as an essential prophylactic measure for the prevention of agranulocytosis during long-term treatment with L1. In cases of L1 agranulocytosis, the toxicity is transient and recovery is achieved following treatment with granulocyte-colony stimulating factor (G-CSF) [33,61]. The mechanism of L1-induced agranulocytosis is thought to be related to an immune response against white cell progenitors produced in the bone marrow. Zinc supplementation is also used for prophylaxis in patients on long-term treatment with L1 [33]. It can be considered that in general, all the toxic side effects of L1 during long-term clinical use are considered controllable, manageable and reversible.
The serious toxic side effects reported during L1 treatments in chronic cases are not expected to appear during short-term treatments, such as those using other drugs in COVID-19 patients. The absence of toxic side effects has also been previously shown during L1 short treatment periods in other categories of non-iron loaded patients.
No serious toxic side effects have in general been observed regarding the posology of L1 in iron loaded and non-iron loaded patients. The range of doses for the proposed use of L1 in COVID-19 patients depends on several parameters including the target characteristics of different aspects of the disease. For example, low doses (10 mg/kg/day) could be used for prophylaxis, whereas maximum doses (100 mg/kg/day) could be used for intensive therapy protocols [62,63]. In considering tolerance, divided doses of L1 of up to 250 mg/kg/day in total have been used in intensive chelation in iron loaded thalassemia patients causing continuous increases in iron excretion and with no apparent toxicity [33,46].
Another parameter of possible toxicity in the use of L1 in COVID-19 patients is the monitoring of serum ferritin levels. Despite that serum ferritin increases are observed in seriously ill COVID-19 patients during the inflammatory response, the changes are not a reflection of an increase in the iron stores. In contrast, decreases of serum ferritin levels in thalassemia major patients reflect a lowering of the iron store levels, and in some cases of low serum levels withdrawal of chelation therapy may be necessary for avoiding iron deficiency [64,65]. However, no substantial decreases of serum ferritin or body iron load can possibly occur during a course of chelation therapy of a short period, e.g., a week in COVID-19 patients.
Overall it can be suggested that there is a very low prospect of toxicity, including insignificant reduction of the iron stores during a short course, e.g., a week’s treatment for COVID-19 patients treated with L1.
This entry is adapted from the peer-reviewed paper 10.3390/ijms23126735
This entry is offline, you can click here to edit this entry!
