Ionchannels are membrane protein that allows the flow of ions across the cell membrane. This is essential for cellular communication and hence mutations that results in non functional protein cause disease. The paper reviews only nonsense mutations of ion channels that cause blindness and proposes several ways this can be corrected.
- Retina, physiology, cell-signaling, pathology, PTC
1. Introduction
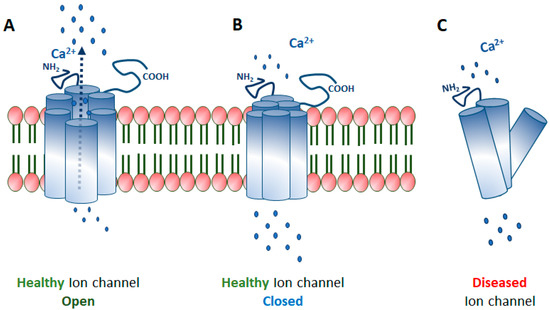
Ion channels are membrane-spanning transport proteins that facilitate the passive bidirectional (into and out of cell and cell organelles) flow of selective ions like sodium (Na+), potassium (K+), calcium (Ca2+), chloride (Cl−), or unspecific cations (Figure 1). These ion channel proteins have an enormous heterogeneity in their electrophysiological properties. In the eye, numerous ion channels are found at different anatomical locations like cornea, lens, ciliary body, and retina, as outlined in Figure 2. A flux of ions generates a membrane potential that maintains the ionic homeostasis required for the proper functioning of cells like signal transmission and visual processing in ocular cells [1,2,3,4]. Ion channels are either gated or non-gated, which permit selective ions to pass through the membrane based on the electrochemical gradient. Gated ion channels are regulated by electrical (membrane potential, voltage), chemical (ligands, cyclic nucleotides, phosphorylation), or other signals (light, temperature, pH, or mechanical stimuli). In contrast, non-gated channels allow the free flow of ions across the membrane.
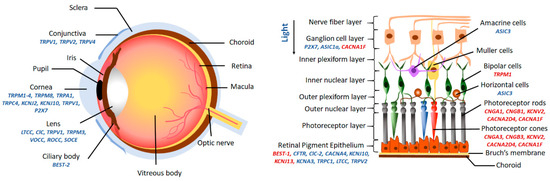
The steady-state regulation of ionic balance by channel proteins is a critical phenomenon in the eye for most of the cellular functions. The most common is the cyclic nucleotide-gated (CNG) cationic channel, which mediates phototransduction in rod and cone photoreceptors by regulating ligand-dependent homeostasis (Na+ and Ca2+) [5,6,7,8,9]. Ca2+ homeostasis is also required to regulate the physiology of the lens, and an overload of Ca2+ is detrimental to the lens, leading to cortical cataract [10]. Different combinations of channels (voltage-operated Ca2+ channels; VOCCs, receptor-operated Ca2+ channels; ROCCs, second messenger-operated Ca2+ channels; SOCE, transient receptor potential channels; TRPs) tightly regulate the Ca2+ influx in lens to maintain its transparency [10,11]. Voltage and ligand operated Ca2+, K+, Cl− channels in the retinal pigmented epithelial (RPE) layer contribute to the secretory activity, volume regulation, and transepithelial ion transport to maintain the retinal health. In contrast, alterations in these channel functions lead to retinal degeneration [12]. K+ channel activity modulates essential action potential in excitable cells and transport and secretory activity in non-excitable cells. K+ channels (inwardly rectifying K+ (Kir)-channels, voltage-gated K+ channels (Kv), Ca2+-activated K+ channels, two-pore or leak K+-channels) are imperative in ocular tissues like the cornea to regulate epithelial cell proliferation and apoptosis [13,14,15], the lens to maintain the volume and transparency [16], the retinal ganglion cells to modulate the resting membrane potential and cell excitability [17], and the RPE cell physiology, for its interaction with the photoreceptor and ionic composition of the subretinal space [18,19]. The passive flow of Cl− in ocular tissues like cornea, conjunctiva, ciliary epithelium, and RPE is mediated by Cl− channels (high- (maxi) conductance, the cystic fibrosis transmembrane conductance regulator (CFTR), volume-regulated, voltage-gated, Ca2+-activated) to regulate tear film volume, aqueous humor volume, corneal transparency, and ionic composition [20,21,22,23,24,25,26,27,28,29,30].
The human genome has over 400 ion channel genes, and several mutations have been reported across several ion channel genes leading to various pathological conditions, known as channelopathies [31]. These mutations may alter the structure, assembly, localization, trafficking, or functions of channel protein and, therefore, turn a sensing ion channel into a non-sensing one (Figure 1C). The effect of these mutations can be studied by electrophysiological techniques. Gene mutations can result in a loss or gain of functions. Structurally, these channel proteins are formed by the assembly of several similar (homomeric) or different (heteromeric) subunits. Therefore, loss-of-function mutations sometimes result in a dominant-negative effect in ion channels. Most of the ocular channelopathies are rare conditions and have been a rapidly expanding, yet unexplored area of ophthalmology. There is a substantial amount of genetic and allelic heterogeneity in channelopathies. It remains unclear how different mutations in the same gene can result in a wide range of phenotypic variability. For example, BEST1 gene mutations result in a spectrum of ocular phenotype such as microcornea, cataract, retinitis pigmentosa, and macular and rod-cone dystrophy [32]. Interestingly, mutations in the same gene exhibit a different inheritance pattern. For example, mutations in the KCNJ13 gene lead to LCA16, an autosomal recessive disease, and snowflake vitreoretinal degeneration (SVD), an autosomal dominant disease [33,34,35].
Many ion channel genes are expressed in the eye, and few are known to harbor the disease-causing mutations. These genes involved in ocular ion channelopathies were identified by chromosomal mapping and targeted exome sequencing (KCNJ13; [35]), microsatellite analysis (CACNA1F; [36]), polymorphism analysis, and recombination mapping (BEST1; [37]), based on the phenotype in a mutant mouse model (CACNA2D4; [38]) and, homozygosity mapping and linkage analysis (KCNV2 [39], CNGA3 [40], CNGB3 [41], CNGB1 [41], CNGA1 [42], TRPM1 [43]). The present article reviews the fundamentals of ocular ion channelopathies caused by these genes, with an exclusive insight into the role of genetic mutations in disease pathogenesis. We also discuss the future percepts of potential pharmacological and therapeutic strategies.
2. Potential Therapies for Reshaping the Non-Sensing Ocular Ion Channels to Sensing Ones
Genetic mutations contribute significantly to the stunning array of ocular channelopathies. The united efforts of clinicians and scientists enabled the discovery of the association of different ion channel genes to the disease phenotype. With the advances in technology, screening mutations across these genes and their effect on specific channel protein function have become possible. It is now known that these ion channels are multimeric in nature and function in-network with several other regulatory proteins. Research on the biophysical properties of ion channels has revealed the fundamental processes responsible for the selective nature of these proteins to understand the normal physiology. These details will help scientists provide a new promising paradigm for precise diagnosis of disease to facilitate the development of rational treatments. Several therapies (Figure 7) and clinical trials targeting the disease-specific genes (mutations), transcripts, or proteins in various ocular tissues are now in practice (Table 2). One advantage of testing the potential therapies in the eye is its easy accessibility for surgical intervention, non-invasive optical imaging, monitoring, and delivering different therapeutics. Also, the presence of the blood-ocular barrier makes the eye immune-privileged and limits the toxicity of drugs and therapies. Innovating the novel therapeutic approaches and their efficient delivery to the eye for various channelopathies is a viable treatment option.
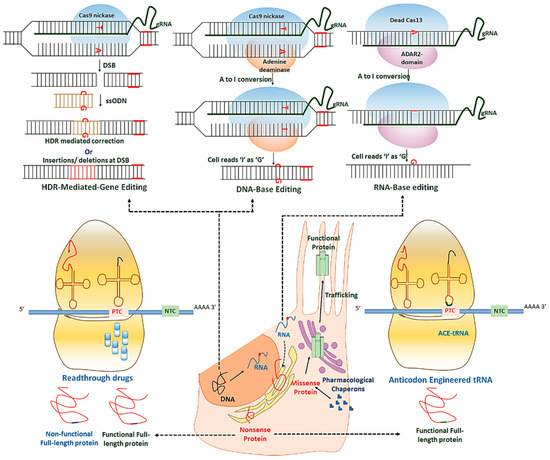
Table 2. Therapies for ion channelopathies in practice and clinical trials.
| Gene | Therapy In Vitro/In Vivo | References |
|---|---|---|
| KCNJ13 | AAV gene therapy in iPSC-RPE in vitro | [242] |
| Read through in iPSC-RPE in vitro | [242] | |
| TRPM1 | AAV gene therapy in mice | [243] |
| BEST1 | AAV2-gene therapy in dogs | [229] |
| Gene augmentation and CRISPR-gene editing in iPSC-RPE | [244] | |
| Pharmacological chaperons in culture cells (MDCK/HEK293) | [245] | |
| CNGA3 | AAV5-mediated gene therapy in mice AAV5-mediated gene augmentation in sheep |
[246,247] |
| NGB3 | AAV-gene therapy in mice | [248,249] |
| CNGB1 | AAV-gene therapy in mice | [250,251] |
3. Concluding Remarks
This entry is adapted from the peer-reviewed paper 10.3390/ijms21186925
