Transcatheter aortic valve replacement (TAVR) is a well-established treatment option for patients with severe symptomatic aortic stenosis (AS) whose procedural efficacy and safety have been continuously improving. Appropriate preprocedural planning, including aortic valve annulus measurements, transcatheter heart valve choice, and possible procedural complication anticipation is mandatory for a successful procedure. The gold standard for preoperative planning is still to perform a multi-detector computed angiotomography (MDCT), which provides all the information required. The planning can be performed manually, using semi-automated and automated software.
1. MDCT Acquisition
The key component for well-acquired MDCT images is an ECG-synchronized MDCT that covers at least the aortic root, followed by non-ECG synchronized images of the aorta, iliac, and femoral vasculature [
29]. The ECG-synchronized MDCT of the aortic root is important, because the aortic annulus undergo conformable change throughout the cardiac cycle, being bigger and circular in systole, and oval in diastole. The goal is to measure the greatest possible annular dimension, which can be found during the cardiac systole (20–40% of the cardiac cycle) [
31,
32].
Regarding radiation, a tube potential of 100 kV is usually indicated for patients weighing <90 kg or with a body mass index (BMI) <30 kg/m2, whereas a tube potential of 120 kV is indicated for patients weighing >90 kg and with BMI >30 kg/m2.
Intravenous contrast administration is mandatory. Optimal images require high intra-arterial opacification, and attenuation values should exceed 250 Hounsfield units. MDCT data should be reconstructed as an axial, thin-sliced multiphasic data set, with <1 mm slice thickness. Reconstruction intervals should be spaced at <10% intervals across the acquired portion of the cardiac cycle [
29].
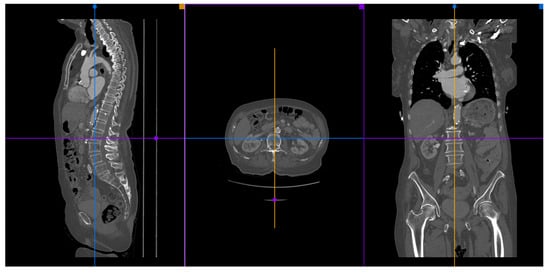
A 3D multiplanar reconstruction (MPR) of the aorta, aortic valve, and its structures is mandatory to perform TAVR planning (Figure 3).
Figure 3. A MPR reconstruction from MDCT images using the Horos® software.
2. Available Methods
Many different kinds of software can be used to make appropriate MDCT measurements of the aortic root, coronary ostia, and optimal angiographic deployment projections: manual, semi-automated, and automated. The manual measures are the most used by operators since they can be done by cheap or free software, such as Horos® and Osirix®.
2.1. Manual Sizing
The manual TAVR sizing is usually made using the 3D MPR tool of Osirix
® or Horos
® software. In the MPR mode, we have three correlated images: coronal, sagittal, and transversal. The goal is to perfectly align the virtual aortic annulus, which corresponds to the base of the three aortic cusps. The manual method does not provide information about the steps needed for sizing, and there is no automated report. In 2019, a consensus on MDCT imaging on TAVR describing the main steps was published [
29]. This consensus provides further and detailed information about MDCT manual preprocedural planning. The manual measurement takes more time than the semi-automated and automated measures, and its learning curve is bigger. However, when used by experienced professionals, it may provide all the information necessary to perform a safe TAVR procedure.
There are some studies comparing the variability of measurement by different observers. These articles found a strong agreement for aortic annulus and coronary arteries height assessment for experienced observers (at least 2 years of experience) [
33,
34].
Furthermore, Knobloch et al. and Le Couteulx et al. reported interobserver variability in MDCTs evaluated by observers with different levels of expertise. In the Le Couteulx et al. study, Observer 1 was an expert, whereas Observer 2 was a resident physician with 6 months of practice, and Observer 3 was a trained resident physician with starting experience. Intra- and inter-observer reproducibility were excellent for all aortic annulus dimensions, with an intraclass correlation coefficient ranging, respectively, from 0.84 to 0.98 and from 0.82 to 0.97. Agreement for selection of prosthesis size was almost perfect between the two most experienced observers (
k = 0.82) and substantial with the inexperienced observer (
k = 0.67) [
35]. In the Knobloch et al. study, Observer 1 was a radiologist with 6 years of experience, Observer 2 was a laboratory technician with 3 years of experience, and Observer 3 was a medical student with no experience. Intra-observer variability did not differ significantly. However, significant differences were found in mean inter-observer variance (
p < 0.001). They advocate that multi-reader paradigms led to significantly increased precision compared with single readers with different levels of experience [
36].
2.2. Semi-Automated and Automated Sizing
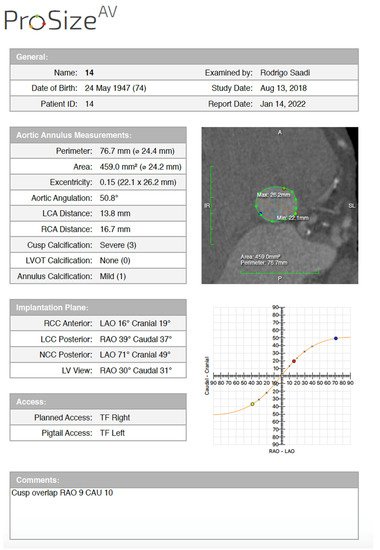
Semi-automated software are broadly used by TAVR companies and operators around the globe. The most commonly utilized software is the 3MensioValves (3mensio Medical Imaging BV, Maastricht, The Netherlands). However, the drawback of 3MensioVales software is its high cost, preventing its broad use (Figure 4). There is another semi-automated software called ProSizeAV, which is actually a plugin to be used with Horos® or Osirix®. However, this plugin does not have CE or FDA approval, and there are no data proving its efficacy (Figure 5).
Figure 4. Measurements performed using the 3MensioValves.
Figure 5. ProSizeAV report.
There is another available semi-automated (syngo. viaVB20A, Siemens, Munich, Germany) software. In 2018, Horehledova et al. compared the Siemens manual and semi-automated software and demonstrated an excellent inter-software agreement (ICC = 0.93; range 0.90–0.95). The time needed for evaluation using semi-automatic assessment (3 min 24 s) was significantly lower (
p < 0.001) compared with a fully manual approach (6 min 31 s) [
37].
Lou et al. also compared manual, semi-automated, and fully automated measurement of the aortic annulus using Siemens software. Semi-automated analysis required major correction in five patients (4.5%). Mean manual annulus area was significantly smaller than fully automated results (
p < 0.001), but similar to semi-automated measurements. The frequency of concordant recommendations for valve size increased if a manual analysis was replaced by semi-automated method (60% agreement was improved to 82.4%; 95% confidence interval for the difference [69.1–83.4%]) [
38].
This entry is adapted from the peer-reviewed paper 10.3390/jcm11092582