Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is an old version of this entry, which may differ significantly from the current revision.
Noroviruses (NoVs) are one of the emerging and rapidly spreading groups of pathogens threatening human health. A reduction in sporadic NoV infections was noted following the start of the COVID-19 pandemic, but the return of NoV gastroenteritis during the COVID-19 pandemic has been noted recently. Research in recent years has shown that different virus strains are associated with different clinical characteristics; moreover, there is a paucity of research into extraintestinal or unusual complications that may be associated with NoV.
- norovirus
- epidemiology
- gastroenteritis
- complications
1. Introduction
Norovirus (NoV) is a nonenveloped virus with a single-stranded, positive-sense, polyadenylated RNA genome that encodes three major open reading frames (ORFs) [1]. ORF1 encodes a large polyprotein that is cleaved by the viral proteinase into six nonstructural proteins, which are involved in NoV replication in host cells. ORF2 encodes the major viral capsid protein (VP) 1 [2], whereas ORF3 encodes VP2, a minor capsid protein involved in viral packaging [3]. The capsid protein consists of a shell (S) domain encoded by conserved genetic lineages and two protruding (P) subdomains: the relatively conserved P1 and highly variable P2 subdomains. The P1 subdomain plays a role in viral-particle stability, whereas the outermost P2 subdomain contains epitopes recognized by neutralizing antibodies and the clefts required for binding to human histo-blood group antigen (HBGA) receptors [4][5][6]. Recombination at the junction of ORF1 and ORF 2 can result in the emergence of a novel viral strain, similar to other RNA viruses [7].
NoVs are highly diverse viruses that can be genetically grouped into 10 genogroups from GI to GX. Only the GI, GII, GIV, GVIII, and GIX genogroups can infect humans, and the GII genogroup is the most prevalent [8][9]. Variants (subgenotypes) are determined by sequence analysis of highly variable regions of the ORF2 and named according to the location and year they were first described [9]. NoV is an emerging pathogen that causes enteric infections in humans and has diverse clinical presentations. Genetic diversity of NoV indicates its rapid evolution with genotype polymorphism. NoV variants related to severe infection and complications have been reported sporadically, and the rapid genetic evolution of NoV is believed to drive changes in its clinical manifestations [10][11][12]. In addition to gastrointestinal (GI) symptoms, NoV infection is associated with several complications, including benign infantile convulsion [13], encephalopathy [14][15][16], necrotizing enterocolitis [17][18], dysregulation of the enteric nervous and immune system [19][20], exacerbation of inflammatory bowel disease [21], and chronic, serious outcomes in immunocompromised patients [22][23].
2. Associated Complications Related to Norovirus Infection
According to the volunteer challenge studies, the asymptomatic infections were estimated at 32.1% [24]. In Taiwan, from winter 2004 to winter 2005, the most common complications were electrolyte imbalance (14.3%) and hypoglycemia (11.4%). After the rotavirus vaccination introduction (from late 2006), the most common complications were convulsive disorder (28%) and hypoglycemia (20%) from winter 2006 to winter 2007. In the 2008/09/10 winters, major complications included GI hemorrhage (22.2%) and prominent hyperthermia (13.8%). From winter 2011 to winter 2012, hyperthermia (34.9%) and GI hemorrhage (23.3%) were the most prominent complications caused by NoV infection [25]. Figure 1 demonstrates the overall complications of NoV infection in different periods in northern Taiwan.
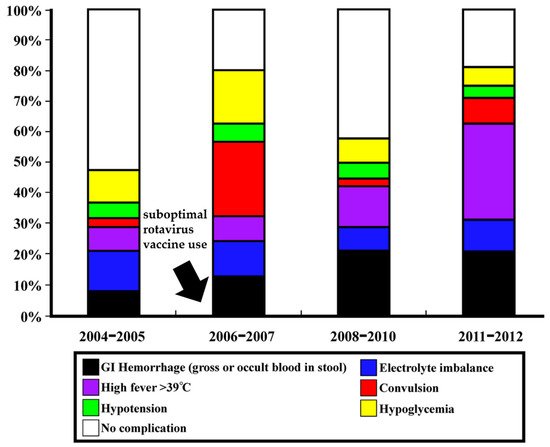
Figure 1. Complications in different periods of NoV outbreaks in northern Taiwan before and after suboptimal rotavirus vaccine introduction from late 2006 (highlight by arrow). The figure has been modified and originated from the research by Wang et al. [25].
Although the specific NoV subgenotypes related to severe infection and complications were only sporadically reported, the rapid genetic evolution of NoV is believed to be the main factor driving the changing clinical manifestations in infected patients. In the 2006/2007 winters, the NoV subgenotype or variant GII.4 Den_Haag_2006b (40%) caused the most complications of convulsion (67.9%) in infected children. The major subgenotype in the 2008/09/10 winters, GII.4 2010 (New Orleans) (48.5%), caused GI hemorrhage (37.5%). Furthermore, GII.4 2012 subgenotypes (56.8%), the predominant NoV strains in the 2011/2012 winter, caused more high fever (57.1%) and GI hemorrhage (33.3%) [25]. Research in northern Taiwan for the clinical relevance and genotypes of circulating NoVs found that patients infected by NoV GII.4 2006b had a higher frequency of diarrhea, longer duration of diarrhea, and more frequent hypoglycemia and electrolyte imbalance compared with those with gastroenteritis caused by NoV GII.4 2010 [26].
Studies in the last 15 years have reported that NoV infection is also associated with a range of sequelae and complications other than gastroenteritis. A recently developed model for NoV infection contributed critical knowledge for extraintestinal or unusual complications. There is still a paucity of research into associated complications in Taiwan. The details of possible associated sequelae or complications with NoV are given below.
2.1. Chronic Gastroenteritis
Chronic NoV gastroenteritis is the major sequela of NoV infection in primary immune deficient and oncologic patients, transplant recipients, and those infected with the human immunodeficiency virus [22][23][27]. Chronic NoV gastroenteritis can present specific clinical challenges in immunocompromised patients. Immunosuppressed patients experience prolonged fecal NoV shedding [28]. NoV diarrhea in cancer patients can contribute to decreased quality of life, interruption of cancer care, malnutrition, and altered mucosal barrier function [29]; in primary immune deficient groups, it is associated with protracted diarrhea, weight loss, and the requirement of parenteral nutrition [30]. Transplant recipients have a similar risk for developing recurrent or chronic infection with NoV as other groups [31]. Immunocompromised patients with chronic NoV infection only have limited options beyond supportive care. For cancer or transplant patients, though only few data support this strategy, immunosuppression should be decreased [32]. There is currently no effective antiviral regimen for chronic NoV infections. Several treatments have been attempted, including serum-derived human immunoglobulin, Nitazoxanide, antiviral agents such as Favipiravir, adoptive T-cell therapy, fecal microbial transplantation, probiotics, and complex microbial communities with glycans with affinity to NoV [33][34][35][36][37]. Further studies are needed to determine if those strategies could be suitable therapies to treat chronic NoV.
2.2. Necrotizing Enterocolitis
The gut microbiota composition during infancy or early childhood is variable, dynamic, and influenced by both prenatal and postnatal factors [38]. Many studies have shown that intestinal viral infections may be associated with severe illness such as hemorrhagic enteritis and even necrotizing enterocolitis (NEC) [17][18][39][40]. Although studies mentioned previously indicated an episodic association of enteric viruses in NEC, one study by Skeath et al. [41] in 2016 for 17 NEC infants without detection of any related viruses may suggest that viral etiology is unlikely to be causative for most sporadic forms of NEC. Understanding of the mechanisms in microbiota-immunity-infectious agent axis is necessary to define potential preventive or therapeutic tools against significant infections in children [38].
2.3. Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a prolonged and disabling functional GI syndrome that affects 9–23% of the population across the world [42]. Acute gastroenteritis is a risk factor for postinfectious irritable bowel syndrome. The pathophysiology of IBS includes several possible mechanisms, such as visceral hypersensitivity, irregular gut motility, abnormal brain–gut relations, and the role of infectious agents; a systematic review showed similar risks for bacterial pathogens and indicated that studies are still limited for viral and parasitic pathogens [43]. There are already many studies showing that a number of pathogens correspond with the IBS disease, such as Clostridium difficile, Escherichia coli, Campylobacter jejuni, Chlamydia trachomatis, Helicobacter pylori, Pseudomonas aeruginosa, Salmonella spp., and Shigella spp.; viruses, particularly NoV; and even parasites [44]. Innate and adaptive immune mechanisms are involved in control of human NoV infection. NoVs may serve as viral triggers for IBS in some environmental and genetic contexts and also indicate that the microbiota may be important for NoV pathogenesis [45]. This still needs further work for understanding interactions between NoVs and bacteria in the gut and understanding the phenotypic outcomes from NoV mutation and evolution.
2.4. Inflammatory Bowel Disease
Inflammatory bowel disease (IBD) includes ulcerative colitis and Crohn’s disease. The burden of IBD is rising globally, with substantial variation in levels and trends of the disease in different countries and regions. There are an estimated 6.8 million IBD cases worldwide, and the prevalence rates range from 79.5 to 84.3 per 100,000 individuals [46]. Although there is some evidence that NoV is involved in the dysregulation of enteric nervous and immune system [19][20] or exacerbation of IBD [21], IBD is influenced by gut microbiota, complex inflammatory pathways, and cell–virus interactions. IBD is also affected by confounding variables such as diet, age, smoking, or psychological stress, as demonstrated in monozygotic twins [47]. While the effect of cytomegalovirus infection on IBD has been confirmed, the role of other viruses in IBD pathogenesis or exacerbation of disease symptoms is still controversial [48][49]. A recent study by Tarris et al. [50] found a strong expression of sialylated Lewis a and Lewis x antigens and human NoV viral-like particles (VLPs) binding in the absence of ABO antigen expression in IBD regenerative mucosa. Further studies are required to explore the implications of NoV in the impairment of epithelial repair and dysregulation of inflammatory pathways [50]. Recent findings regarding human NoV replication in intestinal enteroids and organoids are promising [51][52]. The use of organoids derived from IBD patients might be useful to investigate the virus–host interactions and genetic responses related to NoV [53].
2.5. Convulsions and Encephalopathy
Some patients with acute gastroenteritis develop convulsions that may be febrile or afebrile convulsions [54]. Specific enteric pathogens have been linked to convulsions in children, such as rotavirus, NoV, Campylobacter, and Shigella [13][14][15][55][56][57][58]. The change in the prevalence of convulsions related to gastroenteritis might be associated with rotavirus vaccination [59]. Several reports have shown that NoV related to mild gastroenteritis causes convulsions without fever, severe dehydration, electrolyte imbalance, and hypoglycemia [13][60][61][62]. Severe central nervous system complications such as meningitis, encephalitis, and encephalopathy have been also described [14][15][16][63][64][65]. A study in the era of post-rotavirus vaccination in Taiwan for molecular epidemiology of NoV gastroenteritis showed that seizures occurred in 20.9% of children with NoV infection. GII.4 Den_Haag_2006b (42.3%) and GII.4 Sydney 2012 (19.2%) were major variants correlated with convulsions. Compared with GII.4 Den_Haag_2006b, the GII.4 Sydney 2012-associated convulsions had similar manifestations except without significant winter preponderance. The NoV infection with convulsions had less febrile course, specific genotype (GII.4) infections, and shorter instances of vomiting [66]. More studies and continuous surveillance are essential for uncommon convulsions associated with emerging NoV strain infections.
2.5.1. Benign Convulsions with Mild Gastroenteritis
Benign convulsions with mild gastroenteritis (CwG) were first reported by Morooka in 1982 [67]. CwG is characterized by afebrile convulsions within 5 days of acute viral gastroenteritis in previously healthy infants and children between the ages of 6 months and 3 years without electrolyte balance or abnormal blood sugar level or abnormal result of cerebrospinal fluid analysis. Several reports have broadened the range of definitions for children aged <6 years with CwG [61][62][68][69][70][71][72][73]. Convulsions in CwG are mostly generalized, usually clustered, and last less than 5 min. Although clustering seizures frequently occur in the acute phase of CwG, the prognosis is good and long-term treatment is usually not required [68].
After rotavirus vaccination, some changes in epidemiology and clinical characteristics occurred in NoV-associated CwG [61][62][71][72][74]. The ratio of NoV-associated CwG to NoV gastroenteritis and that of rotavirus-associated CwG to rotavirus gastroenteritis were different among studies [72][75]. One nationwide dataset from health insurance reviews and associated services in South Korea showed that the prevalence of rotavirus-associated CwG did not change (0.013–0.024%) but the annual prevalence of NoV-associated CwG is increasing by 1.790 times each year from 0.00001% [71][72]. However, these studies have limitations as they use diagnostic codes without compiling data directly from patient charts. Therefore, further studies are necessary to determine the actual prevalence after rotavirus vaccination.
There are many reports on the pathophysiological mechanism of CwG but most of them are for rotavirus [76][77][78][79][80][81]. Several studies have attempted to identify the mechanisms of NoV-associated CwG. NoV penetration into the gastrointestinal tract and RNA in the serum and cerebrospinal fluid have been observed [64][82]. There is still a paucity of studies on the pathophysiology of NoV-associated CwG.
2.5.2. Encephalopathy/Encephalitis
Encephalitis is associated with significant mortality despite intensive care [83]. There were few reports or case series, mainly from Japan, related to NoV-associated encephalopathy or encephalitis [16][64][65][84]. A nationwide survey of NoV-associated encephalitis/encephalopathy in Japan showed that the outcome of children with NoV-associated encephalitis was poor. Poor prognosis included early onset of neurological symptoms, an elevated serum creatinine level, and an abnormal blood glucose level [16]. Elevated concentrations of cerebrospinal fluid interleukin-6, interleukin-10, interferon-γ, and tumor necrosis factor-α indicated that the encephalopathy may be related to hypercytokinemia rather than direct viral invasion [84]. Future studies are required since there is no effective treatment and the definite pathophysiology of NoV-associated encephalitis/encephalopathy is still unknown.
2.6. Other Possible Associated Extraintestinal Complications
There have been reports that NoV infection is associated with Guillain–Barre syndrome and its variant Miller Fisher syndrome [85][86]. Although it is still unclear if NoV is the one of the antecedent infections in Guillain–Barre syndrome, it might be linked to the molecular mimicry [87]. As NoV serology is usually unavailable in routine clinical practice, further studies related to this response are needed.
This entry is adapted from the peer-reviewed paper 10.3390/pathogens11040451
This entry is offline, you can click here to edit this entry!
