The high incidence of fungal infections has become a worrisome public health issue, having been aggravated by an increase in host predisposition factors. Despite all the drugs available on the market to treat these diseases, their efficiency is questionable, and their side effects cannot be neglected. Bearing that in mind, it is of upmost importance to synthetize new and innovative carriers for these medicines not only to fight emerging fungal infections but also to avert the increase in drug-resistant strains.
- Nanoparticles
- Fungi
- Drug delivery systems
- Marine
- Biological synthesis
- Myconanotechnology
1. Definition
There is a wide range of fungal infections, from superficial, affecting skin, to systemic infections with invasion of internal organs [1]. Fungal infections affect millions of people every year worldwide. Of these, more or less 1.5 million are invasive fungal infections therefore requiring advanced treatment and hospitalization. Most of these disseminated infections are caused by Candida, Cryptococcus, Aspergillus, and Pneumocystis species, being the cause of cryptococcosis, candidiasis, aspergillosis, and pneumocystis pneumonia, respectively [2].
Superficial fungal infections are rather common and, despite rarely being life threatening, they can spread to other skin regions and even become widespread. Furthermore, they can be transmitted to other people and may cause secondary bacterial skin infections, harming the quality of a person’s life. Skin mycoses are classified according to the causative fungal agents into dermatophytosis, yeast infections, and mold infections [1].
2. Introduction
Invasive fungal infections represent a significant burden to healthcare systems, having high morbidity and mortality rates. These rates are most worrisome among immunocompromised patients that are more prone to opportunistic infections, such as patients with Acquired Immune Deficiency Syndrome (AIDS), transplant patients whose immune systems are suppressed to prevent organ rejection, patients with cancer who are taking immunosuppressive chemotherapy or autoimmune patients undergoing immunosuppressive therapy [2,3].
The currently major available agents to treat invasive fungal infections can be grouped into four main classes according to their mechanism of action: polyenes, azoles, allylamines, and echinocandins (Table 1) [4]. They all present drawbacks when it comes to spectrum of activity, drug–drug interactions, pharmacokinetics and pharmacodynamics, resistance mechanisms, and the toxicity of the compounds themselves. Furthermore, there are some limitations in terms of clinical efficacy and efficiency, mainly because of their physical-chemical properties, like their hydrophobic character that leads to a low solubility in water and also selectivity problems deriving from the similarities between fungi and human cells [3,5].
Table 1. Targets of each group of antifungals [6,7].
| Class | Target (Mechanism of Action) | Antifungal | |
|---|---|---|---|
| Azoles | Ergosterol (inhibition of lanosterol 14-α-demethylase) | Imidazoles | Miconazole |
| Econazole | |||
| Ketoconazole | |||
| Clotrimazole | |||
| Triazoles | Itraconazole | ||
| Fluconazole | |||
| Voriconazole | |||
| Allylamines | Ergosterol (inhibition of squalene epoxidase) | Terbinafine | |
| Naftifine | |||
| Butenafine | |||
| Polyenes | Cell membrane (production of ROS) | Amphotericin B | |
| Ergosterol (inhibition of lanosterol 14-α-demethylase) | Nystatin | ||
| Echinocandines | Cell wall (block of β-1,3 glucan synthesis) | Caspofungin, Micafungin, Anidulafungin | |
| Other antifungals | Chelation of polyvalent metal cations | Ciclopirox | |
| Microtubules (prevention of the formation of the mitotic spindle) | Griseofulvin | ||
| Ergosterol (inhibition of D14 reductase and D7-D8 isomerase) | Amorolfine | ||
Nevertheless, the design and development of new drug delivery systems or even new antifungals is an emerging need, owing to the following facts [8]:
-
There are 20–40% mortality rates with invasive mycoses, therefore these figures need to be improved;
-
The increase in patients undergoing prolonged antifungal therapies reflects the need to develop better fungicidal drugs and thus reduce the length of the treatments and the costs associated;
-
There is still space for improvement in pharmacokinetics and pharmacodynamics, in order to reduce the frequency of drug use;
-
More attention needs to be given to the host toxicities and drug–drug interactions of current therapy so that their effects can be eliminated or, at least, minimized;
-
New therapy groups with different mechanisms of action are needed; this way, these new drugs may synergize with present ones and allow better responses;
-
There is an alarming growth in antifungal resistance in all therapeutic groups [8].
Nanotechnology is an emerging field of science that has shown an undeniable versatility and has boosted a revolution when it comes to medical treatments, quicker diagnosis, cellular regeneration, and drug delivery [9,10]. The material to produce nanoparticles can be divided into three main groups: polymers, lipids, or metals, each one giving rise to a different type of nanoparticle [11]. The main representatives of each of these three different groups of nanoparticles are mentioned in Figure 1 below.
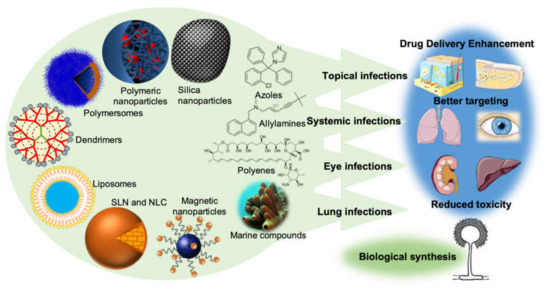
Figure 1. The new drug delivery systems based on nanotechnology that are currently being employed in order to enhance drug delivery, promote a better targeting, and reduce the toxicity of conventional antifungal drugs. It is also important to point out the importance of the production of nanoparticles by fungi (biological synthesis) and the undeniable potential of the sea as a source of new molecules with antifungal activity.
Nanoparticles have been employed in pharmaceutical formulations because of their ability to alter and improve the pharmacokinetic and pharmacodynamic properties of the drugs. This is given to their capability to increase the solubility and stability of the drugs, to allow a controlled release and to exhibit biocompatibility with tissues and cells, which is reflected in an overall improvement on therapeutic efficiency [11,12]. In addition, its subcellular size is compatible with an intravascular injection and its high surface area is amenable to modification so that the drug is released in a specific target, thus reducing the systemic adverse effects and increasing the therapeutic compliance, by decreasing the usual dose and the frequency of administration [13,14]. This targeted-specific action is possible since, at a nanomolecular level, it is possible to incorporate target ligands that allow a preferential binding of certain types of cells, by conjugation with antibodies and peptides on the surface of the transporters [15,16,17]. Hence, the development of new biopharmaceutical systems, especially nanoparticulate carriers, is a good strategy to improve the therapeutic efficacy, safety, and compliance of conventional antifungal drugs.
In Table 2 an overview of the new antifungal drug delivery systems is presented, and the drug chemical group, their route of administration, and their dosage form provided.
Table 2. Some of the novel drug delivery systems already developed for each antifungal drug.
| Antifungal Drugs | Novel Drug Delivery Systems | Routes of Administration | Dosage Forms | References |
|---|---|---|---|---|
| Miconazole | Niosomes | Transdermal | Gel | [18] |
| SLN | Oral | N.A. | [19] | |
| Topical | Gel | [20] | ||
| Microemulsion | Topical | N.A. | [21] | |
| Liposomes | Topical | Gel | [22] | |
| Nanoemulsion | Topical | N.A. | [23] | |
| Nanosponges | Vaginal | Gel | [24] | |
| Transfersomes | Topical | Gel | [25] | |
| Econazole | Microemulsion | Percutaneous | N.A. | [26] |
| Topical | Gel | [27] | ||
| SLN | Topical | Gel | [28] | |
| NLC | Topical | Gel | [29] | |
| Liposomes | Topical | Gel | [30] | |
| Ethosomes | Topical | Gel | [31] | |
| Transethosomes | Transdermal | Gel | [32] | |
| Nanosponges | Topical | Hydrogel | [33] | |
| Niosomes | Transdermal | Gel | [34] | |
| Polymeric micelles | Topical | N.A. | [35] | |
| Nanoemulsion | Topical | N.A. | [36] | |
| Ketoconazole | SLN/NLC | Topical | Gel | [37] |
| Niosomes | Topical | Gel | [38] | |
| Microemulsion | Oral | N.A. | [39] | |
| Spanlastics | Ocular | N.A. | [40] | |
| Dendrimers | Topical | Hydrogel | [41] | |
| Liposomes | Topical | N.A. | [42] | |
| Clotrimazole | Liposomes | Topical | Gel | [43] |
| Nanosponges | Topical | Hydrogel | [44] | |
| Ethosomes | Topical | Gel | [45] | |
| Niosomes | Topical | Gel | [46] | |
| Polymeric emulgel | Topical | Gel | [47] | |
| Polymeric micelles | Topical | N.A. | [35] | |
| SLN/NLC | Topical | N.A. | [48] | |
| Microemulsion | Buccal | Gel | [49] | |
| Vaginal | Gel | [50] | ||
| Transfersomes | Transdermal/Topical | N.A. | [51] | |
| Itraconazole | Transfersomes | Transdermal | N.A. | [52] |
| SLN | Ocular | N.A. | [53] | |
| NLC | Inhalation | N.A. | [54] | |
| Niosomes | Topical | N.A. | [55] | |
| Microemulsion | Transdermal | N.A. | [56] | |
| Liposomes | Topical | N.A. | [57] | |
| Polymeric nanoparticles | Oral | N.A. | [58] | |
| Polymersome | Intravenous | N.A. | [54] | |
| Spanlastics | Ocular | N.A. | [59] | |
| Silica nanoparticles | Oral | N.A. | [60] | |
| Fluconazole | Microemulsion | Vaginal | Gel | [61] |
| Niosomes | Ocular | Gel | [62] | |
| Liposomes | Intravitral | N.A. | [63] | |
| SLN | Topical | Gel | [64] | |
| NLC | Oral | N.A. | [65] | |
| Microsponges | Topical | Gel | [66] | |
| Ethosomes | Topical | Gel | [67] | |
| Spanlastics | Ocular | N.A. | [68] | |
| Polymeric amphiphilogel | Topical | Gel | [69] | |
| Polymeric micelles | Topical | N.A. | [35] | |
| Voriconazole | Microemulsion | Ocular | N.A. | [70] |
| Polymeric nanoparticles | Ocular | N.A. | [71] | |
| Pulmonar | N.A. | [72] | ||
| SLN | Topical | Gel | [73] | |
| Transethosome | Topical | N.A. | [74] | |
| Ethosome | Topical | N.A. | [75] | |
| Terbinafine | Liposomes | Topical | Gel | [76] |
| SLN | Topical | N.A. | [77] | |
| Transfersomes | Topical | N.A. | [78] | |
| Spanlastics | Transungual | N.A. | [79] | |
| Polymeric chitosan nanoparticles | Topical | Hydrogel | [80] | |
| Naftifine | Microemulsion | Topical | N.A. | [81] |
| Niosomes | Topical | Gel | [82] | |
| Butenafine | Microemulsion | Topical | Hydrogel | [83] |
| Amphotericin B | Liposomes | Intravenous | N.A. | [84] |
| SLN/NLC | Oral | N.A. | [85] | |
| Topical | N.A. | [86] | ||
| Magnetic nanoparticles | Nasal instilation | N.A. | [87] | |
| Nanoemulsion | Topical | N.A. | [88] | |
| Polymeric nanoparticles | Intravenous | N.A. | [89] | |
| Oral | N.A. | [90] | ||
| Polymersomes | Oral | N.A. | [91,92] | |
| Transfersomes | Topical | N.A. | [93] | |
| Micelles | Intravenous | N.A. | [94] | |
| Silica nanoparticles | Intravenous | N.A. | [95] | |
| Nystatin | SLN | Topical | N.A. | [96] |
| Nanoemulsion | Topical | N.A. | [97] | |
| Liposomes | Intravenous | N.A. | [98] | |
| Niosomes | Parenteral | N.A. | [99] | |
| Griseofulvin | Niosomes | Oral | N.A. | [100] |
| Ciclopirox | Niosomes | Topical | Gel | [101] |
| Caspofungin, Micafungin, Anidulafungin, Amorolfine | No nano-tech studies yet released | |||
N.A.: the dosage form is not mentioned in the reference cited; SLN: Solid Lipid Nanoparticles; NLC: Nanostructured Lipid Carriers.
However, the efficacy and human safety of these new therapies remain uncertain in most of the articles found in literature. They generally lack controlled clinical trials and sometimes the suggested routes of administration are less practical, or the production cost may hinder the replacement of the conventional treatment. Nevertheless, in other cases, the opposite is verified, and some options have potential to become a viable first line treatment [102]. Moreover, given the widespread use of antifungal agents and the limited therapeutic offer, fungi have developed resistance mechanisms, like overexpression of efflux pump proteins and formation of biofilms. These mechanisms can mean not only a decrease in a drug’s effective concentration, but also changes and subexpression of drug targets and metabolic bypass [6]. It is important to add that resistance is a cross-cutting issue to all of the currently available classes of antifungal agents, therefore overcoming antifungal resistance can be considered as the mainstay for improving therapeutic strategies to treat antifungal infections [2,103].
Despite the uprising of these issues in antifungal therapy, there are several mechanisms by which nanoparticles overcome the development of resistance mechanisms:
-
The resistance mechanisms can be prevented by packaging multiple antimicrobial drugs within the same nanoparticle, because the likelihood of multiple simultaneous gene mutations in the same cell is low. The most striking examples are the encapsulation of antifungal drugs in chitosan or silver nanoparticles, combining the antifungal properties of both and decreasing the possibility of drug resistance [104,106];
-
Some nanoparticles, such as liposomes and dendrimers, are able to overcome the resistance mechanisms of decreased uptake and increased efflux of drug from the microbial cell. Liposomes are able to quickly fuse with the plasma membrane of the microbial cell and release a high concentration of drug into its plasma membrane or cytoplasm, thereby circumventing the decreased uptake mechanism of resistance. This means a faster delivery and avoidance of the transmembrane pumps that catalyze increased efflux of drugs. Dendrimers, on the other hand, are extensively branched molecules, whose surface can be filled with positively charged quaternary ammonium compounds, which bind to negatively charged microbial cell envelopes and increase membrane permeability. This allows the entrance of more dendrimers to the microbial cell, the flow of its cytoplasmic contents to the exterior, and the ultimate destruction of the microbial cell membrane. This goes to show that dendrimers are also able to surpass the resistance mechanism of decreased uptake of drug [107]. Other nanoparticles, specifically nitric oxide nanoparticles made of silica and zinc oxide nanoparticles are able to overcome biofilm formation by killing the microbes present in already formed biofilms or by inhibiting biofilm formation through the generation of reactive oxygen species, respectively [108,109];
-
Nanoparticles have been used to target antifungal drugs to the specific site of infection, allowing the local release of high concentrations of drug, while keeping the total dose of drug administered low. This high local dose is able to destroy the infecting fungi before they can develop resistance, thereby overcoming this worrisome issue and translating into fewer side effects upon the patient [104].
That being said, it is also important that the research done, not only focuses on formulating these systems, but also in overcoming the major challenges that their placing on the market faces: the physical instability of nanoparticles, their small capacity of drug loading, the cytotoxicity/immunogenicity, and the high cost of production and standardization, given the complexity of the formulations. Besides that, there is almost a complete lack of studies in vivo as reaching the therapeutic range needed to perform these studies has proven to be an arduous job. That lies in the fact that, in many cases, there is an anticipated release of the drug, aggregation and precipitation of the nanoparticles, and the accumulation in non-target tissues.
This entry is adapted from the peer-reviewed paper 10.3390/ph13090248
