The posterior segment of the eye comprises the back two-thirds of the eye, including the vitreous humor, the retina, the choroid and the optic nerve. Posterior Segment Eye Diseases (PSEDs) are then defined as the disorders that affect these tissues with the common main outcome of varying degrees of visual impartment and blindness. The most prevalent diseases are glaucoma, age-related macular degeneration (AMD) and diabetic retinopathy (DR). This specialized organ is composed of various static and dynamic barriers that restrict drug delivery into the target site of action. Despite numerous efforts, effective intraocular drug delivery remains unresolved and, therefore, it is highly desirable to improve the current treatments of diseases affecting the posterior cavity.
1. Introduction
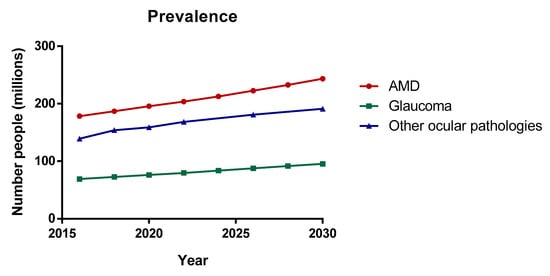
The posterior segment of the eye comprises the back two-thirds of the eye, including the vitreous humor, the retina, the choroid and the optic nerve. Posterior Segment Eye Diseases (PSEDs) are then defined as the disorders that affect these tissues with the common main outcome of varying degrees of visual impartment and blindness. The most prevalent diseases are glaucoma, age-related macular degeneration (AMD) and diabetic retinopathy (DR) (see Figure 1). Nowadays, millions of people are suffering from retinal and choroid diseases and the number is increasing every year, as the incidence significantly increases with age. Both disorders are characterized by their severity and difficulty of treating. Despite numerous efforts, effective intraocular drug delivery remains unresolved and therefore, it is highly desirable to improve the current treatments of diseases affecting the vitreous cavity.
Figure 1. Prevalence of the main ocular pathologies. Data from the world report on vision published by the World Health Organization (WHO), 2019 [
1].
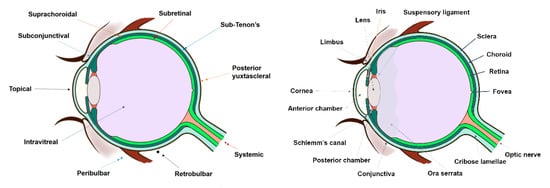
In clinical practice, the standard procedure in treating these disorders is the intravitreal administration of injected drugs, although topical and systemic administration have also been addressed with limited results. Thus, other approaches have been developed for the treatment of posterior segment diseases such as periocular, suprachoroidal, and subretinal administration (Figure 2). All these routes of drug administration consist of the drug/system injection in the surroundings of the target site. Periocular administration includes subconjunctival, sub-Tenon’s, peribulbar, retro bulbar, and posterior juxtascleral injection. However, these injections might not result in therapeutic drug levels in the target site due to the necessity of crossing several barriers to reach the intended site of action. This limitation could be overcome by using more effective drug delivery systems, where improved therapies may also be achieved.
Figure 2. The first image represents a scheme of the different routes of drug administration to the posterior segment (dots symbolize the injection site of each route), while second image exemplifies the anatomy of the eye.
One of the main drawbacks of drug delivery to the back of the eye is the narrow interval dosing because of the low effectiveness and bioavailability of the administered drug. Also, it should be taken into consideration that intravitreal and periocular routes are highly invasive, being associated to discomfort and patient compliance. Intraocularly, a prolonged drug release not only entails the patient acceptability by increasing their quality of life, but also, a notable reduction in the economic costs associated to the hospital stays due to the frequently repeated injections that are necessary to complete the treatment.
Drug delivery to the posterior segment of the eye still remains a great challenge in the pharmaceutical industry due to the complexity and particularity of the anatomy and physiology of the eye. Some advances have been made with the purpose of maintaining constant drug levels in the site of action. The anatomical ocular barriers have a great impact on drug pharmacokinetics and, subsequently, on the pharmacological effect.
2. Routes of Drug Delivery to the Posterior Segment of the Eye
2.1. Intravitreal Administration
Intravitreal injection is the mainstream route of administration to treat diseases affecting the posterior segment of the eye. The drug is placed directly into the vitreous humor, though it is a highly targeted drug route. It has the inconvenience of being an invasive route. However, intravitreal drug administration is always selected to deliver to the posterior ocular segment due to the possibility of overcoming systemic exposure and obtaining high drug levels into the vitreous chamber.
2.2. Topical Administration
Ophthalmic topical administration by eye drops is commonly used for the treatment of anterior-segment diseases [
98,
99]. Most of the topically applied drugs are intended for the treatment of diseases that affect different layers of the cornea, the conjunctiva, iris, or the ciliary body [
5]. However, topical administration for the treatment of posterior ocular diseases is considered an ineffective pharmacological strategy since therapeutic drug concentrations are not reached in the posterior segment of the eye due to low drug penetration.
2.3. Systemic Administration
Systemic administration route constitutes an alternative route in the treatment of eye’s posterior segment pathologies. It is normally used as a coadjutant treatment or as a second choice after the failure of intravitreal or subconjunctival injections treatment. It is based on drug administration by conventional routes (e.g., oral, intravenous, or intramuscular). Once the drug reaches the bloodstream, the absorption will take place through conjunctival, episcleral and/or choroidal vessels to get the vitreous cavity, although most of the drugs do not pass the main blood–ocular barriers [
6].
2.4. Periocular Administration
The periocular route has been considered as a promising drug administration route for the posterior ocular segment diseases treatment due to the high concentrations obtained with this kind of formulations’ inoculation. This route allows the drug deposition on the scleral external surface and includes the following administration routes: subconjunctival, subTenon´s, retrobulbar, peribulbar and posterior juxtascleral. These pathways differ from one another in the location and/or injection direction in the proximity of the sclera.
3. Conclusions
The eye is one of the most inaccessible organs in terms of obtaining therapeutic drug concentrations, especially in the treatment of posterior segment ocular pathologies. Conventional administration pathways, such as topical or systemic routes, usually show important limitations, either by low ocular penetration or by the appearance of side effects linked to the posology, among others.
New drug delivery systems (DDS) are needed to prolong the administration intervals for posterior segment ocular pathologies, even though the development of novel DDS is particularly complicated due to several aspects must be considered, such as pharmacokinetics, immunogenicity, biodegradation, tolerability and toxicity, among others. Apart from these, different technological requirements must be taken into account, including reproducible manufacturing, clinical performance and sterility.
In the last few decades, an exponential increase in the design and development of novel DDS intended for the treatment of posterior segment ocular pathologies was observed. Biodegradable and non-biodegradable implants, microparticles, nanoparticles, microneedles, and microelectromechanical systems are the most innovative ones. Unfortunately, knowledge about drug targeting to the posterior segment of the eye is still sparse and, thus, there is not many DDS in clinical trials. Even so, memantine ophthalmic formulations as neuroprotective are in III phase studies at the moment, inter alia.
Likewise, huge advances were made in terms of research and development of new alternative administration routes to the posterior segment of the eye, including intravitreal and periocular pathways as the most relevant ones, as well as their subtypes. All of them, including a conventional administration routes (topical and systemic) show a series of specific pharmacokinetic characteristics, making them useful for the treatment of certain posterior segment ocular pathologies. However, these pathways have shown several advantages and limitations, where the election of one or another is dependent on, not just the pathology itself, but the pharmaceutical form, the drug used and the patient´s adherence to treatment, among others.
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics12030269