Conventional chemotherapy is the most common therapeutic method for treating cancer by the application of small toxic molecules that interact with DNA and cause cell death. Unfortunately, these chemotherapeutic agents are non-selective and can damage both cancer and healthy tissues, producing diverse side effects, and they can have a short circulation half-life and limited targeting. Many synthetic polymers have found application as nanocarriers of intelligent drug delivery systems (DDSs). Their unique physicochemical properties allow them to carry drugs with high efficiency, specifically target cancer tissue and control drug release. In recent years, considerable efforts have been made to design smart nanoplatforms, including amphiphilic block copolymers, polymer-drug conjugates and in particular pH- and redox-stimuli-responsive nanoparticles (NPs).
- block copolymers
- polymer-drug conjugates
- polymeric nanocarriers
- cancer therapy
1. Introduction
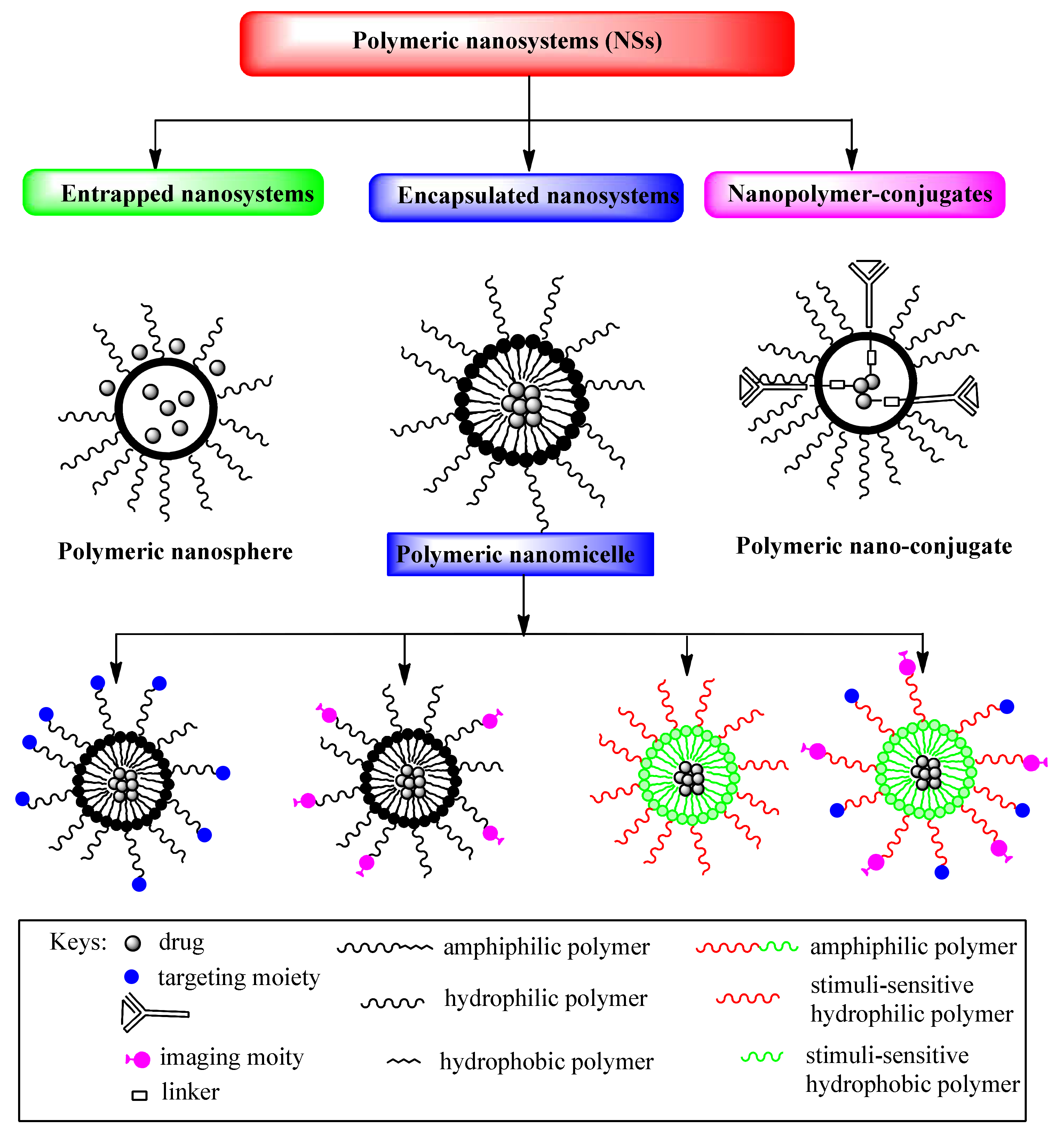
2. Polymeric Nanoparticles (NPs)
3. Amphiphilic Block Copolymers as Carriers in Drug Delivery Systems
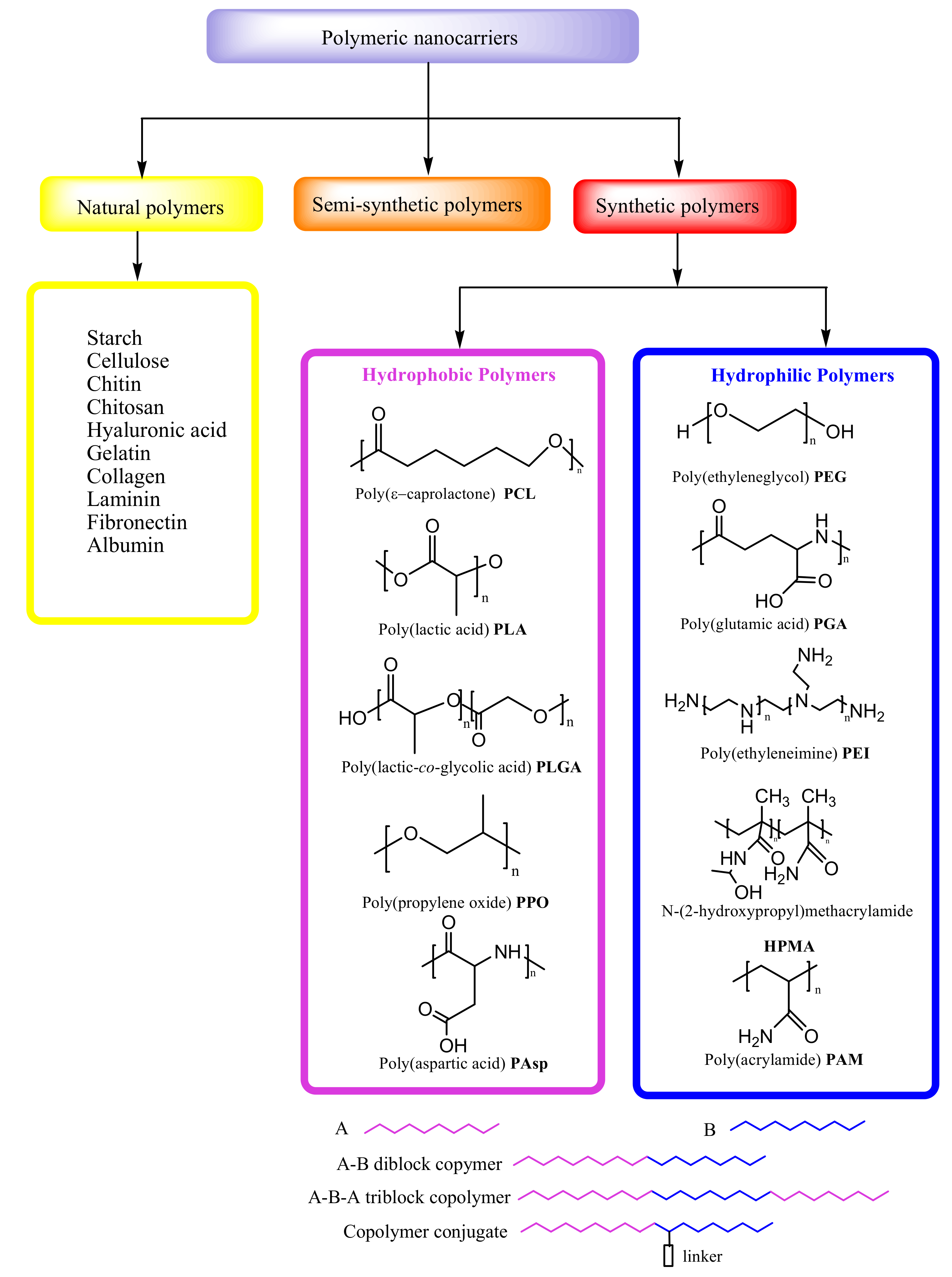
3.1. Hydrophobic and Hydrophilic Polymeric Nanocarriers
3.2. Block Copolymers of DDSs in Cancer Therapy
|
Polymer |
Drug |
Loading Mode |
Function |
Reference |
|---|---|---|---|---|
|
PEG-PCL |
Camptothecin (CPT) |
Entrapment |
Colon, breast, ovarian, lung and brain cancers |
[39] |
|
PCL-PEG-PCL |
Paclitaxel (PTX) |
Encapsulation |
Lung cancers in combination with chrono-modulated chemotherapy |
[40] |
|
PLGA-PEG |
Paclitaxel (PTX) |
Encapsulation |
Breast, pancreatic and ovarian and brain cancers |
[44] |
|
PLGA-TPGS |
Doxorubicin(DOX)- Metformin (Met) |
Encapsulation |
Multidrug resistance P388 cancer cell lines |
[45] |
|
PEG-PGlu |
Cisplatin |
Encapsulation |
Solid cancers |
|
|
mPEG-PLGA-PGlu |
Doxorubicin(DOX) |
Encapsulation |
Breast cancer |
[49] |
|
PEG-PAsp |
Paclitaxel (PTX) |
Entrapment |
Advanced stomach cancer |
|
|
PEO-b-PAsp |
Doxorubicin |
Entrapment |
Pancreatic cancer |
[53] |
|
PEO-PPO-PEO |
Doxorubicin. |
Encapsulation |
Metastatic adenocarcinoma of the esophagus and gastroesophageal junction |
|
|
PCLLA-PEG-PCLLA |
Doxorubicin (DOX) |
Encapsulation |
Breast cancer |
[56] |
|
PEI-PLA |
Paclitaxel (PTX) |
Entrapment |
Lung cancer |
[57] |
|
PEG |
Camptothecin (CPT)SN38 Irinotecan (C-11) |
Copolymer-drug conjugation |
Colorectal, metastatic breast cancer, platinum-resistant ovarian cancer and metastatic cervical cancer |
|
|
HPMA |
Doxorubicin (DOX) |
Copolymer-drug conjugation |
Lung and breast cancer |
|
|
HPMA |
Paclitaxel (PTX) |
Copolymer-drug conjugation |
Solid cancers |
[66] |
|
HPMA |
Diaminocyclohexane(DACH)-platinum |
Copolymer-drug conjugation |
Solid cancer, ovarian cancer |
3.3. Polymer-Drug Conjugates in Cancer Therapy
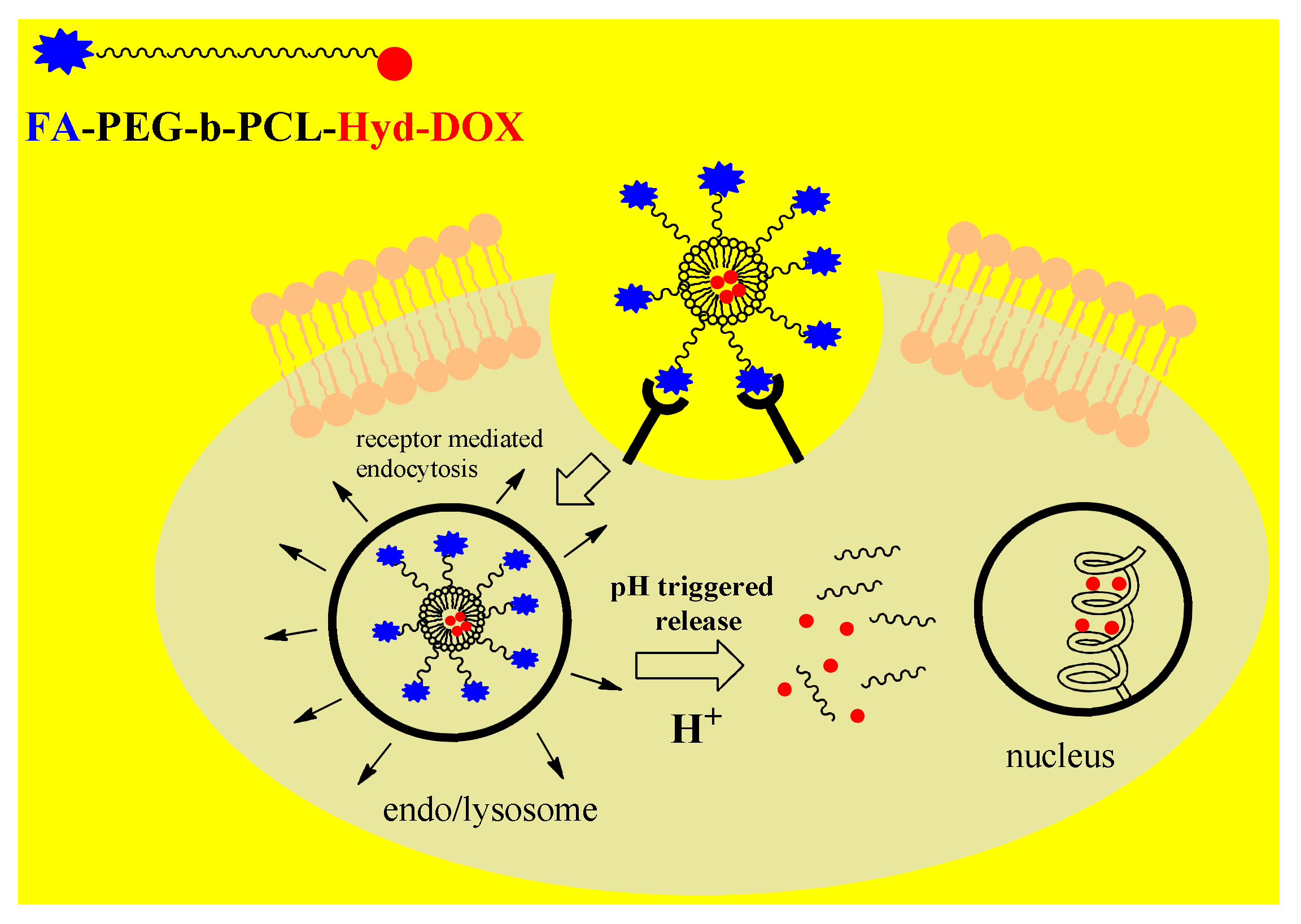
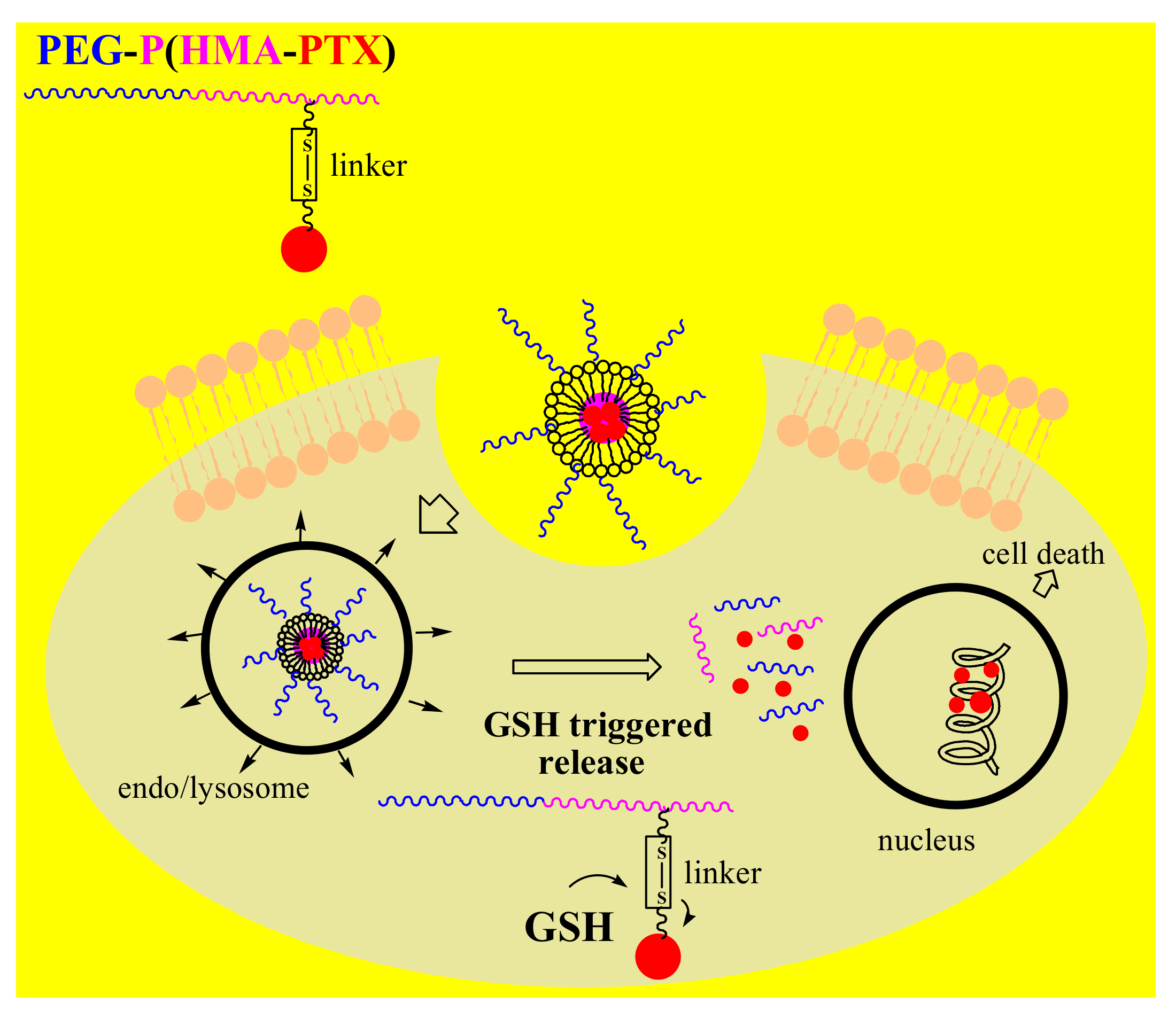
4. Stimuli-Responsive Polymer-Drug Conjugates
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics12040298
References
- Tran, S.; DeGiovanni, P.J.; Piel, B.; Rai, P. Cancer nanomedicine: A review of recent success in drug delivery. Clin. Transl. Med. 2017, 6, 44.
- Bahrami, B.; Hojjat-Farsangi, M.; Mohammadi, H.; Anvari, E.; Ghalamfarsa, G.; Yousefi, M.; Jadidi-Niaragh, F. Nanoparticles and targeted drug delivery in cancer therapy. Immunol. Lett. 2017, 190, 64–83.
- Pérez-Herrero, E.; Fernández-Medarde, A. Advanced targeted therapies in cancer: Drug nanocarriers, the future of chemotherapy. Eur. J. Pharm. Biopharm. 2015, 93, 52–79.
- Avramović, N.; Ignjatović, N.; Savić, A. Platinum and ruthenium complexes as promising molecules in cancer therapy. Srp. Arh. Celok. Lek. 2019, 147, 105–109.
- Escobar, Q.M.; Maschietto, M.; Krepischi, A.C.V.; Avramovic, N.; Tasic, L. Insights into the Chemical Biology of Childhood Embryonal Solid Tumors by NMR-Based Metabolomics. Biomolecules 2019, 9, 843.
- Radic, T.; Coric, V.; Bukumiric, Z.; Pljesa-Ercegovac, M.; Djukic, T.; Avramovic, N.; Matic, M.; Mihailovic, S.; Dragicevic, D.; Dzamic, Z.; et al. GSTO1*CC Genotype (rs4925) Predicts Shorter Survival in Clear Cell Renal Cell Carcinoma Male Patients. Cancers 2019, 11, 2038.
- Hossen, S.; Hossain, K.M.; Basher, M.K.; Mia, M.N.H.; Rahman, M.T.; Uddin, J.M. Smart nanocarrier-based drug delivery systems for cancer therapy andtoxicity studies: A review. J. Adv. Res. 2019, 15, 1–18.
- Guo, X.; Wang, L.; Wei, X.; Zhou, S. Polymer-Based Drug Delivery Systems for Cancer Treatment. J. Polym. Sci. A Polym. Chem. 2016, 54, 3525–3550.
- Parveen, S.; Arjmand, F.; Tabassum, S. Clinical developments of antitumor polymertherapeutics. RSCAdv. 2019, 9, 24699–24721.
- Fathi, M.; Barar, J. Perspective highlights on biodegradable polymeric nanosystems for targeted therapy of solid tumors. Bioimpacts 2017, 7, 49–57.
- Calzoni, E.; Cesaretti, A.; Polchi, A.; Di Michele, A.; Tancini, B.; Emiliani, C. Biocompatible Polymer Nanoparticles for Drug Delivery Applications in Cancer and Neurodegenerative Disorder Therapies. J. Funct. Biomater. 2019, 10, 4.
- Cabral, H.; Kataoka, K. Progress of drug-loaded polymeric micelles into clinical studies. J. Control. Release 2014, 190, 465–476.
- Allen, T.M. Ligand-targeted therapeutics in anticancer therapy. Nat. Rev. Cancer 2002, 2, 750–763.
- Torchilin, V. Antibody-modified liposomes for cancer chemotherapy. Expert Opin. Drug Deliv. 2008, 5, 1003–1025.
- Cheng, W.W.; Allen, T.M. The use of single chain Fv as targeting agents for immunoliposomes: An update on immunoliposomal drugs for cancer treatment. Expert Opin. Drug Deliv. 2010, 7, 461–478.
- Farokhzad, O.C.; Cheng, J.; Teply, B.A.; Sherifi, I.; Jon, S.; Kantoff, P.W.; Richie, J.P.; Langer, R. Targeted nanoparticle-aptamer bioconjugates for cancer chemotherapyin vivo. Proc. Natl. Acad. Sci. USA 2006, 103, 6315–6320.
- Oba, M.; Vachutinsky, Y.; Miyata, K.; Kano, M.R.; Ikeda, S.; Nishiyama, N.; Itaka, K.; Miyazono, K.; Koyama, H.; Kataoka, K. Antiangiogenic gene therapy of solid tumor bysystemic injection of polyplex micelles loading plasmid DNA encoding soluble flt-1. Mol. Pharm. 2010, 7, 501–509.
- Miura, Y.; Takenaka, T.; Toh, K.; Wu, S.; Nishihara, H.; Kano, M.R.; Ino, Y.; Nomoto, T.; Matsumoto, Y.; Koyama, H.; et al. Cyclic RGD-linked polymeric micelles for targeted delivery of platinum anticancer drugsto glioblastoma through the blood-brain tumor barrier. ACS Nano 2013, 7, 8583–8592.
- Bae, Y.; Jang, W.D.; Nishiyama, N.; Fukushima, S.; Kataoka, K. Multifunctional poly-meric micelles with folate-mediated cancer cell targeting and pH-triggered drug releasing properties for active intracellular drug delivery. Mol. Biosyst. 2005, 1, 242–250.
- Torchilin, V.P. Cell penetrating peptide-modified pharmaceuticalnanocarriers for intracellular drug and gene delivery. Biopolymers 2008, 90, 604–610.
- Skatrud, P.L. The impact of multiple drug resistance (MDR) proteins on chemotherapy and drug discovery. Prog. Drug Res. 2002, 58, 99–131.
- Dai, X.; Tan, C. Combination of microRNA therapeutics with small-molecule anticancer drugs: Mechanismof action and co-delivery nanocarriers. Adv. Drug Deliv. Rev. 2015, 81, 184–197.
- Teo, P.Y.; Cheng, W.; Hedrick, J.L.; Yang, Y.Y. Co-delivery of drugs and plasmid DNA for cancer therapy. Adv. Drug Deliv. Rev. 2016, 98, 41–63.
- Navarro, G.; Pan, J.; Torchilin, V.P. Micelle-like nanoparticles as carriers for DNA and siRNA. Mol. Pharm. 2015, 12, 301–313.
- Alinejad, V.; Hossein Somi, M.; Baradaran, B.; Akbarzadeh, P.; Atyabi, F.; Kazerooni, H.; SamadiKafil, H.; AghebatiMaleki, L.; Siah Mansouri, H.; Yousefi, M. Co-delivery of IL17RB siRNA and doxorubicin bychitosan-based nanoparticles for enhanced anticancer efficacy in breast cancer cells. Biomed. Pharmacother. 2016, 83, 229–240.
- Wei, W.; Lv, P.P.; Chen, X.M.; Yue, Z.G.; Fu, Q.; Liu, S.Y.; Yue, H.; Ma, G.H. Codelivery of mTERT siRNA and paclitaxel by chitosan-based nanoparticles promoted synergistic tumor suppression. Biomaterials 2013, 34, 3912–3923.
- Li, N.; Huang, C.; Luan, Y.; Song, A.; Song, Y.; Garg, S. Active targeting co-delivery system based onpH-sensitive methoxy-poly(ethylene glycol)2K-poly(epsilon-caprolactone)4K-poly(glutamic acid)1K forenhanced cancer therapy. J. Colloid Interface Sci. 2016, 472, 90–98.
- Pan, J.; Palmerston Mendes, L.; Yao, M.; Filipczak, N.; Garai, S.; Thakur, G.A.; Sarisozen, C.; Torchilin, V.P. Polyamidoamine dendrimers-based nanomedicine for combination therapy with siRNAand chemotherapeutics to overcome multidrug resistance. Eur. J. Pharm. Biopharm. 2019, 136, 18–28.
- Wang, X.; Liow, S.S.; Wu, Q.; Li, C.; Owh, C.; Li, Z.; Loh, X.J.; Wu, Y.L. Codelivery for Paclitaxel and Bcl-2 Conversion Gene by PHB-PDMAEMA Amphiphilic Cationic Copolymer for Effective Drug Resistant Cancer Therapy. Macromol. Biosci. 2017, 17, 1700186.
- Cheng, Q.; Du, L.; Meng, L.; Han, S.; Wei, T.; Wang, X.; Wu, Y.; Song, X.; Zhou, J.; Zheng, S.; et al. The Promising Nanocarrier for Doxorubicin and siRNA Co-delivery by PDMAEMA-based Amphiphilic Nanomicelles. ACS Appl. Mater. Interfaces 2016, 8, 4347–4356.
- Cheng, H.; Yang, W.; Chen, H.; Liu, L.; Gao, F.; Yang, X.; Jiang, Q.; Zhang, Q.; Wang, Y. Surface modificationof mitoxantrone-loaded PLGA nanospheres with chitosan. Colloids Surf. B Biointerfaces 2009, 73, 212–218.
- Wang, L.; Hao, Y.; Li, H.; Zhao, Y.; Meng, D.; Li, D.; Shi, J.; Zhang, H.; Zhang, Z.; Zhang, Y. Co-delivery of doxorubicin and siRNA for glioma therapy by a brain targeting system: Angiopep-2-modifiedpoly(lactic-co-glycolic acid) nanoparticles. J. Drug Target 2015, 23, 832–846.
- Cao, N.; Cheng, D.; Zou, S.; Ai, H.; Gao, J.; Shuai, X. The synergistic effect of hierarchical assemblies of siRNA and chemotherapeutic drugs co-delivered into hepatic cancer cells. Biomaterials 2011, 32, 2222–2232.
- Navarro, G.; Sawant, R.R.; Biswas, S.; Essex, S.; Tros de Ilarduya, C.; Torchilin, V.P. P-glycoprotein silencingwith siRNA delivered by DOPE-modified PEI overcomes doxorubicin resistance in breast cancer cells. Nanomedicine 2012, 7, 65–78.
- Huang, H.Y.; Kuo, W.T.; Chou, M.J.; Huang, Y.Y. Co-delivery of anti-vascular endothelial growth factorsiRNA and doxorubicin by multifunctional polymeric micelle for tumor growth suppression. J. Biomed. Mater. Res. A 2011, 97, 330–338.
- Knop, K.; Hoogenboom, R.; Fischer, D.; Schubert, U.S. Poly(ethylene glycol) in drug delivery: Pros and cons as well as potential alternatives. Angew. Chem. Int. Ed. 2010, 49, 6288–6308.
- Zhou, S.; Deng, X.; Yang, H. Biodegradable poly(epsilon-caprolactone)-poly(ethylene glycol) block copolymers: Characterization and their use as drug carriers for a controlled delivery system. Biomaterials 2003, 24, 3563–3570.
- Zhang, Z.; Qu, Q.; Li, J.; Zhou, S. The Effect of the Hydrophilic/Hydrophobic Ratio of Polymeric Micelles on their Endocytosis Pathways into Cells. Macromol. Biosci. 2013, 13, 789–798.
- Çırpanlı, Y.; Allard, E.; Passirani, C.; Bilensoy, E.; Lemaire, L.; Çalış, S.; Benoit, J.P. Antitumoral activity ofcamptothecin-loaded nanoparticles in 9L rat glioma model. Int. J. Pharm. 2011, 403, 201–206.
- Hu, J.; Fu, S.; Peng, Q.; Han, Y.; Xie, J.; Zan, N.; Chen, Y.; Fan, J. Paclitaxel-loaded polymeric nanoparticles combined with chronomodulated chemotherapy on lung cancer: In vitro and in vivo evaluation. Int. J.Pharm. 2017, 516, 313–322.
- Hong, G.; Yuan, R.; Liang, B.; Shen, J.; Yang, X.; Shuai, X. Folate-functionalized polymeric micelle as hepatic carcinoma-targeted, MRI-ultrasensitive delivery system of antitumor drugs. Biomed. Microdevices 2008, 10, 693–700.
- Wen, X.; Wu, Q.P.; Ke, S.; Ellis, L.; Charnsangavej, C.; Delpassand, A.S.; Wallace, S.; Li, C. Conjugation with (111)In-DTPA-poly(ethylene glycol)improves imaging of anti-EGF receptor antibody C225. J. Nucl. Med. 2001, 42, 1530–1537.
- Lee, H.; Hoang, B.; Fonge, H.; Reilly, R.M.; Allen, C. In vivo distribution of polymeric nanoparticles at the whole-body, tumor, and cellular levels. Pharm. Res. 2010, 27, 2343–2355.
- Guo, J.; Gao, X.; Su, L.; Xia, H.; Gu, G.; Pang, Z.; Jiang, X.; Yao, L.; Chen, J.; Chen, H. Aptamer-functionalized PEG–PLGA nanoparticles for enhance danti-glioma drug delivery. Biomaterials 2011, 32, 8010–8020.
- Shafiei-Irannejad, V.; Samadi, N.; Salehi, R.; Yousefi, B.; Rahimi, M.; Akbarzadeh, A.; Zarghami, N. Reversion of Multidrug Resistance by Co-Encapsulation of Doxorubicin and Metformin in Poly(lactide-co-glycolide)-D-α-tocopheryl Polyethylene Glycol 1000 Succinate Nanoparticles. Pharm. Res. 2018, 35, 119.
- Matsumura, Y. Polymeric Micellar Delivery Systems in Oncology. Jpn. J. Clin. Oncol. 2008, 38, 793–802.
- Wilson, R.H.; Plummer, R.; Adam, J.; Eatock, M.; Boddy, A.V.; Griffin, M.; Miller, R.; Matsumura, Y.; Shimizu, T.; Calvert, H. Phase I and pharmacokinetic study of NC-6004, a new platinum entity of cisplatin-conjugated polymer forming micelles. Clin. Oncol. 2008, 26, 2573.
- Plummer, R.; Wilson, R.H.; Calvert, H.; Boddy, A.V.; Griffin, M.; Sludden, J.; Tilby, M.J.; Eatock, M.; Pearson, D.G.; Ottley, C.J. A Phase I clinical study of cisplatin-incorporated polymeric micelles (NC-6004) in patients with solid tumours T. Br. J. Cancer 2011, 104, 593–598.
- Yuan, J.D.; ZhuGe, D.L.; Tong, M.Q.; Lin, M.T.; Xu, X.F.; Tang, X.; Zhao, Y.Z.; Xu, H.L. pH-sensitive polymericnanoparticles of mPEG-PLGA-PGlu with hybrid core for simultaneous encapsulation of curcumin anddoxorubicin to kill the heterogeneous tumour cells in breast cancer. Artif. Cells Nanomed. Biotechnol. 2018, 46, 302–313.
- Matsumura, Y. Poly (amino acid) micelle nanocarriers in preclinical and clinical studies. Adv. Drug Deliv. Rev. 2008, 60, 899–914.
- Hamaguchi, T.; Matsumura, Y.; Suzuki, M.; Shimizu, K.; Goda, R.; Nakamura, I.; Nakatomi, I.; Yokoyama, M.; Kataoka, K.; Kakizoe, T. NK105, a paclitaxel-incorporating micellar nanoparticle formulation, can extend in vivo antitumour activity and reduce the neurotoxicity of paclitaxel. Br. J. Cancer 2005, 92, 1240–1246.
- Hamaguchi, T.; Kato, K.; Yasui, H.; Morizane, C.; Ikeda, M.; Ueno, H.; Muro, K.; Yamada, Y.; Okusaka, T.; Shirao, K.; et al. A phase I and pharmacokinetic study of NK105, a paclitaxel-incorporating micellar nanoparticle formulation. Br. J. Cancer 2007, 97, 170–176.
- Vilar, G.; Puche, J.T.; Albericio, F. Polymers and drug delivery systems. Curr. Drug Deliv. 2012, 9, 367–394.
- Venne, A.; Li, S.; Mandeville, R.; Kabanov, A.; Alakhov, V. Hypersensitizing effect of pluronic L61 on cytotoxic activity, transport and subcellular distribution of doxorubicin in multiple drug-resistant cells. Cancer Res. 1996, 56, 3626–3629.
- Valle, J.W.; Armstrong, A.; Newman, C.; Alakhov, V.; Pietrzynski, G.; Brewer, J.; Campbell, S.; Corrie, P.; Rowinsky, E.K.; Ranson, M. A phase 2 study of SP1049C, doxorubicin in P-glycoprotein-targeting pluronics, in patients with advanced adenocarcinoma of the esophagus and gastroesophageal junction. Investig. New Drugs 2010, 29, 1029–1037.
- Hu, D.; Chen, L.; Qu, Y.; Peng, J.; Chu, B.; Shi, K.; Hao, Y.; Zhong, L.; Wang, M.; Qian, Z. Oxygen-generating Hybrid Polymeric Nanoparticles with Encapsulated Doxorubicin and Chlorin e6 for Trimodal Imaging-Guided Combined Chemo-Photodynamic Therapy. Theranostics 2018, 8, 1558–1574.
- Jin, M.; Jin, G.; Kang, L.; Chen, L.; Gao, Z.; Huang, W. Smart polymeric nanoparticles with pH-responsive and PEG-detachable properties for co-delivering paclitaxel and survivin siRNA to enhance antitumor outcomes. Int. J. Nanomed. 2018, 13, 2405–2426.
- Greenwald, R.B.; Pendri, A.; Conover, C.D.; Lee, C.; Choe, Y.H.; Gilbert, C.; Martinez, A.; Xia, Y.; Wu, D.; Hsue, M. Camptothecin-20-PEG ester transport forms: The effect of spacer groups on antitumor activity. Bioorg. Med. Chem. 1998, 6, 551–562.
- Fraier, D.; Frigerio, E.; Brianceschi, G.; Casati, M.; Benecchi, A.; James, C. Determination of MAG-Camptothecin, a new polymer-bound Camptothecin derivative, and free Camptothecin in dog plasma by HPLC with fluorimetricdetection. J. Pharm. Biomed. Anal. 2000, 19, 505–514.
- Singer, J.W.; Bhatt, R.; Tulinsky, J.; Buhler, K.R.; Heasley, E.; Klein, P.; James, C. Water-soluble poly-(l-glutamic acid)–Gly-camptothecin conjugates enhance camptothecin stability and efficacy in vivo. J. Control. Release 2001, 74, 243–247.
- Pastorino, F.; Loi, M.; Sapra, P.; Becherini, P.; Cilli, M.; Emionite, L.; Ribatti, D.; Greenberger, L.M.; Horak, I.D.; Ponzoni, M. Tumor Regression and Curability of Preclinical Neuroblastoma Models by PEGylated SN38 (EZN-2208), a Novel Topoisomerase I Inhibitor. Clin. Cancer Res. 2010, 16, 4809–4821.
- Sapra, P.; Zhao, H.; Mehlig, M.; Malaby, J.; Kraft, P.; Longley, C.; Greenberger, L.M.; Horak, I.D. Novel Delivery of SN38 Markedly Inhibits Tumor Growth in Xenografts, Including a Camptothecin-11–Refractory Model. Clin. Cancer Res. 2008, 14, 1888–1896.
- Crozier, J.A.; Advani, P.P.; Plant, B.L.; Anthony, T.H.; Jaslowski, J.; Moreno-Aspitia, A.; Perez, E.A. N0436 (Alliance): A phase II trial of irinotecan plus cetuximab in patients with metastatic breast cancer previously exposed to anthracycline and/or taxane-containing therapy. Clin. Breast Cancer 2016, 16, 23–30.
- Duncan, R.; Vicent, M.J. Do HPMA copolymer conjugates have a future as clinically useful nanomedicines? A critical overview of current status and future opportunities. Adv. Drug Deliv. Rev. 2010, 62, 272–282.
- Seymour, L.W.; Ferry, D.R.; Kerr, D.J.; Rea, D.; Whitlock, M.; Poyner, R.; Boivin, C.; Hesslewood, S.; Twelves, C.; Blackie, R.; et al. Phase II studies of polymer-doxorubicin (PK1, FCE28068) in the treatment of breast, lung and colorectal cancer. Int. J. Oncol. 2009, 34, 1629–1636.
- Terwogt, J.M.M.; ten BokkelHuinink, W.W.; Schellens, J.H.M.; Schot, M.; Mandjes, I.; Zurlo, M.; Rocchetti, M.; Rosing, H.; Koopman, F.M.; Beijnen, J.H. Phase I clinical and pharmacokinetic study of PNU166945, a novel water-soluble polymer-conjugated prodrug of paclitaxel. Anticancer Drugs 2001, 12, 315–323.
- Campone, M.; Rademaker-Lakhai, J.M.; Bennouna, J.; Howell, S.B.; Nowotnik, D.P.; Beijnen, J.H.; Schellens, J.H. Phase I and pharmacokinetic trial of AP5346, a DACH-platinum-polymer conjugate, administered weekly for three out of every 4 weeks to advanced solid tumor patients. Cancer Chemother. Pharmacol. 2007, 60, 523–533.
- Rice, J.R.; Howell, S.B. AP-5346. Drugs Future 2004, 29, 561.
- Kelland, L. Broadening the clinical use of platinum drug–based chemotherapy with new analogues. ExpertOpin. Investig. Drugs 2007, 16, 1009–1021.
- Nowotnik, D.P.; Cvitkovic, E. ProLindac™(AP5346): A review of the development of an HPMA DACH platinum Polymer Therapeutic. Adv. Drug Deliv. Rev. 2009, 61, 1214–1219.
- Pasut, G.; Veronese, F.M. PEG conjugates in clinical development or use as anticancer agents: An overview. Adv. Drug Deliv. Rev. 2009, 61, 1177–1188.
- Kopecek, J.; Kopeckova, P. HPMA copolymers: Origins, early developments, present, and future. Adv. Drug Deliv. Rev. 2010, 62, 122–149.
- Bae, Y.; Nishiyama, N.; Fukushima, S.; Koyama, H.; Yasuhiro, M.; Kataoka, K. Preparation and biological characterization of polymeric micelle drug carriers with intracellular pH-triggered drug release property: Tumor permeability, controlled subcellular drug distribution, and enhanced invivo antitumor efficacy. Bioconjug.Chem. 2005, 16, 122–130.
- Xiong, X.B.; Ma, Z.; Lai, R.; Lavasanifar, A. The therapeutic response to multifunctional polymeric nano-conjugates in the targeted cellular and subcellular delivery of doxorubicin. Biomaterials 2010, 31, 757–768.
- Wu, P.; Opadele, A.E.; Onodera, Y.; Nam, J. Targeting Integrins in Cancer Nanomedicine: Applications in Cancer Diagnosis and Therapy. Cancers 2019, 11, 1783.
- Shi, C.; Guo, X.; Qu, Q.; Tang, Z.; Wang, Y.; Zhou, S. Actively targeted delivery of anticancer drug to tumor cells by redox-responsive star-shaped micelles. Biomaterials 2014, 35, 8711–8722.
- Chen, W.; Shah, L.A.; Yuan, L.; Siddiq, M.; Hu, J.; Yang, D. Polymer–paclitaxel conjugates based on disulfide linkers for controlled drug release. RSC Adv. 2015, 5, 7559–7566.
