Cancer is a chronic disease that is responsible for the high death rate, globally. The administration of anticancer drugs is one crucial approach that is employed for the treatment of cancer, although its therapeutic status is not presently satisfactory. The anticancer drugs are limited pharmacologically, resulting from the serious side effects, which could be life-threatening. Polymer drug conjugates, nano-based drug delivery systems can be utilized to protect normal body tissues from the adverse side effects of anticancer drugs and also to overcome drug resistance. They transport therapeutic agents to the target cell/tissue.
1. Introduction
Cancer is a chronic disease that leads to great mortality around the world and cancer cases are rising continuously [
1]. It is the second cause of death worldwide, followed by cardiovascular diseases [
2]. It is characterized by an abnormal uncontrolled proliferation of any type of cells in the human body [
3]. It is caused by external factors, such as smoking, infectious organisms, pollution, and radiation; it is also caused by internal factors, such as immune conditions, hormones, and genetic mutation [
3]. Although there are several types of cancer, the most common ones are breast, colorectal, and lung cancer [
4]. The most-reported common cancer in women is breast cancer, while in men, it is lung cancer. It has been estimated that the cases of cancer burden in the world increased to 18.1 million, while deaths caused by cancer increased to 9.6 million in 2018 [
5].
Treatment of cancer includes radiotherapy, surgery, hormonal therapy, immunotherapy, and chemotherapy (anticancer drugs) [
3,
6]. The method of treatment employed depends on the location and the stage of the tumor [
7]. The use of anticancer drugs is the most employed method, and they are therapeutic agents that can be used to target proteins, tissue environment, and genes that are responsible for cancer growth. Cancer is treated by combination therapy, involving the use of two or more anticancer agents [
8]. In addition to combination therapy, a polymer-based drug delivery system is another potential strategy that has been reported to enhance the therapeutic efficacy of anticancer agents [
9].
Polymer-based drug delivery systems have been utilized in biomedical applications to deliver therapeutic agents to the target biological environment [
10]. They exhibit distinct features, such as reduced drug toxicity, improved patient compliance, increased drug solubility, enhanced drug bioavailability, biocompatibility, and biodegradability, control drug release mechanism, protect the drug from deactivation, and preserve drug activity during circulation [
11]. There are several polymer-based drug delivery systems that have been formulated to improve therapeutic outcomes of anticancer drugs, such as polymer capsules [
12,
13,
14,
15,
16,
17], polymeric nanoparticle [
18,
19,
20,
21,
22,
23], dendrimers [
24,
25,
26,
27,
28,
29], micelles [
30], hydrogels [
31], nanogels [
32], in situ gels [
33], polymer-drug conjugates [
34,
35,
36,
37], and nanoliposomes [
38,
39,
40,
41,
42,
43].
2. Classification of Anticancer Chemotherapeutics Based on Their Mechanism of Actions
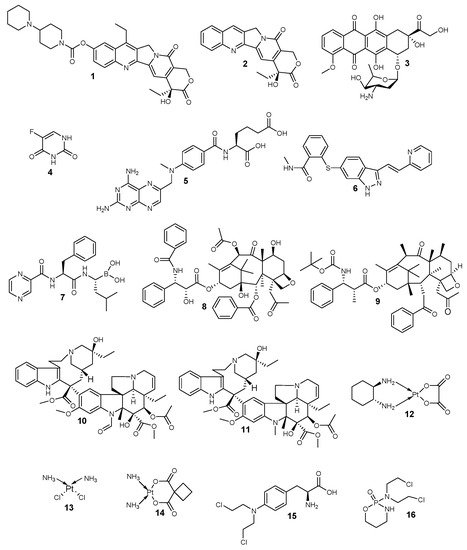
Anticancer drugs are categorized based on their mechanism of action into four distinct classes: topoisomerase inhibitors, antimetabolites, anti-tubulin agents, and alkylating agents (
Figure 1 and
Table 1). Topoisomerase inhibitors hinder the replication of deoxyribonucleic acid (DNA), and their examples include irinotecan
1, camptothecin
2, and doxorubicin
3 [
44,
45,
46]. They act by binding to the topoisomerase active site resulting in the hindrance of the binding of the DNA substrate. They also form a cleavage complex, which prevents enzyme turnover and the build-up of high levels of the cytotoxic cleavage complex within the cell [
47].
Figure 1. Anticancer drugs based on their mode of action.
Table 1. A summary of the classification of anticancer drugs.
|
Classes of Anticancer Drugs
|
Mode of Action
|
General Mechanisms of Resistance
|
Examples
|
|
Topoisomerase inhibitors
|
They hinder the binding of the DNA substrate. They also form a cleavage complex, which prevents enzyme turnover and the build-up of high levels of the cytotoxic cleavage complex within the cell.
|
The altered proliferation and drug targets, reduced sensitivity to apoptosis and cell death, increased ability to repair DNA damage, expression of drug efflux pumps, and detoxification mechanisms.
|
1–3
|
|
Antimetabolites
|
They hinder the biosynthesis of nucleic acids.
|
4–7
|
|
Anti-tubulin agents
|
They disrupt mitotic spindles and terminate mitosis.
|
8–11
|
|
Alkylating agents
|
They bind covalently with the DNA and crosslink them, thereby disrupting the DNA.
|
12–16
|
Antimetabolites hinder biosynthesis of nucleic acids, and the examples of antimetabolites are 5-fluorouracil
4, methotrexate
5, bevacizumab
6, and bortezomib
7 [
48]. Anti-tubulin agents disrupt mitotic spindles and terminate mitosis [
49]. Examples of anti-tubulin agents include paclitaxel
8, docetaxel
9, vincristine
10, and vinblastine
11, and they act on tubulins [
50]. Paclitaxel is the most active anticancer drug that is employed for the treatment of several types of cancer. Alkylating agents covalently bind with the DNA and crosslink them [
51]. Examples of alkylating agents are oxaliplatin
12, cisplatin
13, carboplatin
14, melphalan
15, and cyclophosphamide
16, which result in DNA disruption [
51].
Limitations of Anticancer Drugs and Multi-Drug Resistance
The aforementioned anticancer drugs indicated in
Table 1 are used to target the quick and rapid division of cells. There are several cells in the body that divide rapidly in a normal way, such as the hair follicle cells, bone marrow cells, and digestive tract cells, which are also affected unintentionally by those anticancer chemotherapeutics and result in severe side effects [
52]. The side effects that can be caused by anticancer drugs include neurotoxicity, cardiotoxicity, mucositis, myelosuppression, and immunosuppression [
53]. Furthermore, the widespread distribution and very short half-life of drugs require more dosing of the anticancer drugs, which can lead to an increase in the aforementioned side effects. Another limitation of most of the presently used anticancer drugs is their hydrophobic nature making them insoluble in aqueous media. The major limitation of all anticancer drugs is drug resistance caused by various factors, including several mutations, etc. [
54].
The multidrug resistance (MDR) is the main problem that makes the treatment of cancer challenging. MDR has been reported due to mechanisms, such as the cancer cells that survived the chemotherapeutics, the pumping out of chemotherapeutics by transporters known as ATP-binding cassette (ABC), cell defense mechanism, the evolving adaptation of the cancer cells biological environment, the mutation of oncogenes that are resistant to former treatments that were employed [
55]. The overexpression of the transporters, such as ABCB1, known as P-glycoprotein, P-gp, ABCG2, known as breast cancer resistant protein, BCRP, and ABCC1, known as multidrug resistance-associated protein 1, MRP1, contributes to MDR [
55]. They expel drugs away from the cell, resulting in decreased intracellular accumulation. The strategy that has been proposed to combat P-glycoprotein 1 is the co-administration of anticancer drugs with P-glycoprotein 1 inhibitor loaded in nanoparticles [
56]. Although this strategy is a potential approach to overcome drug resistance, it has a limitation, which is the lower capability of some anticancer drugs to cleave from the nanoparticles or not cleaving at all [
7].
The biological features of tumors that hinder the accessibility of drugs and protect the cancer cells from drug cytotoxicity are tumor vasculature, which is abnormal and heterogeneous, cell density, interstitium, and interstitial fluid pressure [
57]. The immature vasculature of tumors hinders the delivery of nutrients and oxygen to the cancer cells. The poor supply of nutrients, oxygen, etc. to the tumor cells induces a mechanism known as angiogenesis in which new lymphatic and blood vessels are formed. The acidic microenvironment of the tumor promotes tumor cell dissemination. The adaptation of the cancer cells contributes to the maintained acidic pH of the tumor [
58]. Selected anticancer drugs are easily ionized, resulting in their poor diffusion via the cell membranes. Low pH has been reported to result in tumor resistance to weak basic anticancer drugs [
58]. The application of polymer-based drug delivery systems is one potential approach that can combat the aforementioned limitations of anticancer chemotherapy, including multidrug resistance.
3. Polymer-Drug Conjugates
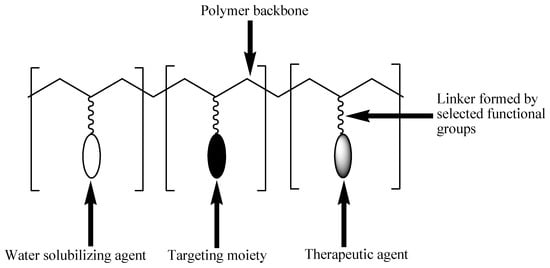
Polymer-drug conjugates, which are also known as polymeric prodrugs, are drug delivery systems that are formulated for the incorporation of therapeutic agents into polymers of choice using selected functionalities [
59]. These delivery systems are unique and composed of three units: solubilizing unit, targeting moiety, and a therapeutic agent. These units are covalently incorporated into the polymer backbone. This model was first proposed by Helmut Ringsdorf in 1975 (
Figure 2) [
60].
Figure 2. Schematic diagram of the Ringsdorf model of polymer-drug conjugates.
The solubilizing unit enhances the water solubility of the conjugates. The targeting moiety improves the transportation of the conjugate to the targeted cell/tissue [
61]. Some targeting moieties used include folic acid, engineered antibodies, sugars, and peptides. Their capability to interact exclusively with specific receptors present on selected cell types makes them very important in the development of polymer-drug conjugates [
62]. The therapeutic agent is usually incorporated into the polymeric backbone via a linker [
61]. The linker plays an important role in the release of the conjugated drug under certain conditions, such as a change in pH, the presence of enzymes or sensitivity, to overexpressed groups of diseased organ/tissue [
63]. The type of linkers used influence the % loading of the drug to the carrier, drug stability, and drug release mechanism. Several linkers, such as hydrazine, azo, peptides, disulfide, etc. have been used for drug conjugation to polymers [
64].
There are three known synthetic routes for the preparation of polymer-drug conjugates, such as the incorporation of a drug to a synthesized polymeric carrier, the incorporation of a drug to a monomer before polymerization, and the incorporation of the drug as monomers or initiators during the polymerization reaction [
65].
The preparation of polymer-drug conjugates via the incorporation of a drug to a monomer before polymerization has been reported to overcome the problem of uncontrolled conjugation to the polymer backbone resulting in a high drug loading and controlled drug loading. The conjugation of the drug to the monomer does not interfere with the polymerization reaction, and the problem of steric hindrance during the conjugation is also overcome [
65,
66].
Polymerization reactions, such as ring-opening metathesis polymerization (ROMP), ring-opening polymerization (ROP), reversible addition-fragmentation transfer polymerization (RAFT), have been used for the preparation of polymer-drug conjugates, whereby the drug is conjugated first to the monomer [
65,
67,
68,
69].
The conjugates prepared via the aforementioned method displayed a good feature, which includes triggered drug release suitable for conjugates loaded with multiple drugs. However, some polymer-drug conjugates prepared by ROMP and RAFT displayed a non-biodegradable backbone [
65,
69,
70]. Employing ROP has been reported to result in polymer-drug conjugates with a biodegradable backbone [
70]. It is important to mention that using a drug as a monomer is not a suitable approach for many drugs, even though it increases the drug conjugation in the polymeric carrier significantly.
Some of the functional groups suitable for the conjugation of drugs in polymer-drug conjugates include amines, alcohols, and carboxylic groups etc. [
71]. Polymer-drug conjugates can be prepared using branched or linear polymeric carriers. Linear carriers include polyaspartimide, poly(malic acid), poly(vinyl pyrrolidone), poly(ethylene glycol) (PEG), and poly(vinyl alcohol) (PVP) polymers [
72]. Branched carriers include poly(amidoamine) and poly(ethyleneimine) polymers [
71]. There are several advantages that are displayed by polymer-drug conjugates, such as improved drug bioavailability and biodegradability [
73], reduced drug toxicity [
74], improved drug stability and water solubility, enhanced drug biocompatibility and drug delivery by sustaining and controlling the drug release mechanism [
75], and they have the ability to overcome drug resistance. However, polymer-drug conjugates have few limitations in combination therapy, such as difficulties in the identification of ratios of incorporated therapeutic agents and poor drug loading capacity [
76]. The conventional anticancer drugs suffer from pharmacological limitations, such as poor oral bioavailability; poor water solubility in which most of them are hydrophobic, and as such, they can not penetrate the biological membranes; instability in circulation and short circulation time due to some of them being engulfed by the macrophages, and thus their short circulation time makes their interaction with the cancerous cells ineffective; poor selectivity towards cancer cells resulting in the normal cells being exposed to the toxic side effects of the drugs; overexpression of a multidrug resistance protein, P-glycoprotein on the surface of the cancerous cells, which act as an efflux pump, preventing the accumulation of anticancer drugs inside the tumor resulting in drug resistance [
77,
78,
79].
Physicochemical Properties of Polymer-Drug Conjugates for Enhanced Tumor Uptake
The physicochemical properties of polymer-drug conjugates, such as the surface charge, conformation, size, and biocompatibility, influence factors, such as their absorption, distribution, excretion, etc. [
65].
Cancer cell surfaces have been reported to be negatively charged resulting from the movement of negatively charged constituents, such as phosphatidylserine, anionic phospholipids, glycoproteins, etc. to the cell surface of cancer [
80]. The pH of most solid tumors is in the range of 5.7–7.8 [
81]. Tumor tissues display acidic plasma pH when compared to normal tissues, which exhibit alkaline-outside pH gradients [
82], resulting in the significantly lower extracellular pH of malignant tumors when compared to normal tissues [
83]. Positively charged nanoparticles are preferentially taken up by the tumors [
84,
85], and they are retained over an extended period when compared to negatively charged or neutral nanoparticles [
84,
86]. Positively charged nanoparticles can penetrate the tumor deeper when compared to anionic and neutral nanoparticles [
65,
87,
88,
89]. Cationic drug carriers improve the interaction of anticancer drugs with transmembrane receptors, such as integrins, which are involved in cell invasion and metastasis and in signaling processes [
90].
The uptake of nanoparticles by the tumor tissue is also influenced by the particle size. Nanoparticles, which are small-sized, penetrate deeper into the tumor tissue and are not cleared rapidly from the tumor [
65]. However, the design of small-sized nanoparticles is challenging, and they do not exhibit high drug loading capability. In order to overcome the above-mentioned challenge, stimuli-responsive nanoparticles that have the capability to shrink their sizes for enhanced tumor penetration have been developed.
Nanocarriers with sizes below 100 nm are suitable for systemic distribution. In order to avoid the rapid clearance of the nanocarriers by the kidneys, the particle size of nanocarriers should be larger than 6 nm. However, some polymer-drug conjugates in clinical trials have been reported to be below 10 nm [
91]. During circulation, nanocarriers can bind with the proteins in the blood, leading to aggregation, and they can be taken up by the macrophages. The aforementioned factor reduces the amount of the drug that is taken up into the tumor tissue. The particle size of the conjugates determines their penetration into tumor tissue. Selected particle sizes have been reported to enhance tumor tissue penetration when compared to larger particle sizes [
92,
93]. Sub-100 nm is a size range of nanocarriers suitable for passive tumor targeting, which is also influenced by their composition [
94].
The molecular weight of polymer conjugates has been reported to influence their circulation in vivo. Polymer-drug conjugates with high molecular weight display extended intravascular half-life with slower excretion from the tumor and body [
65,
95]. Researchers have reported the high tumor accumulation of high-molecular-weight greater than 50 kDa in clinical trials [
96,
97,
98]. However, high-molecular-weight polymers can also hinder conjugated drugs from reaching their target cell/tissue [
97]. Lower molecular weight polymer-drug conjugates have also been reported for combination therapy and enhanced cellular uptake [
99,
100].
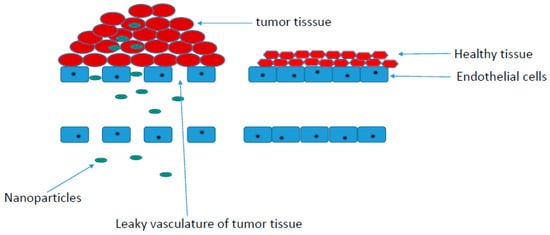
Tumors consist of vasculature and supporting cells. Their capillaries are irregular when compared to a normal tissue vasculature, which is characterized by tight endothelial cells, preventing the penetration of nanoparticles [
101]. Tumor tissue vasculatures are leaky and highly permeable. Their permeability promotes enhanced permeation retention (EPR) accumulation effects of polymer-drug conjugates in solid tumors. The accumulation of polymer-drug conjugates in the tumor is influenced by the high interstitial fluid pressure in tumor tissues when compared to the normal tissues (
Figure 3) [
101]. EPR-mediated accumulation of nanoparticles has been reported to be high in tumors, such as breast, lung, and ovary tumors when compared to other tumors [
102].
Figure 3. EPR (enhanced permeation retention) uptake of polymer-drug conjugates.
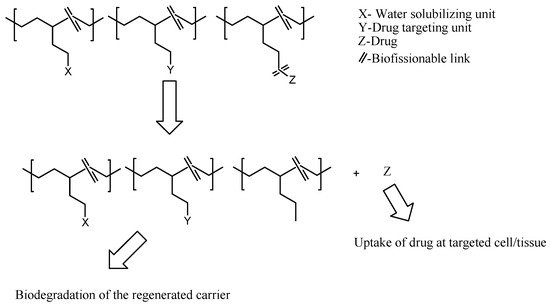
Active targeting of nanoparticles can also be influenced by the conjugation of targeting molecules overexpressed on the tumor cell surface [
103]. The targeting molecules conjugated on nanoparticles bind to cells via an endosome-dependent mechanism. This mechanism bypasses the drug efflux pump resulting in a high intracellular uptake [
101]. Drug release from polymer-drug conjugates resulting from the biological stimulus, such as enzyme or pH, has been widely reported by employing stimulus sensitive linkers, which trigger drug release (
Figure 4) [
104,
105]. Some examples of pH-sensitive linkers are hydrazine, amide, imine, cis-aconityl, oxime, thiopropionate, etc. [
65].
Figure 4. In vivo pharmacokinetic release of drug from the polymer-drug conjugates.
4. Polymer-Anticancer Drug Conjugates Effective against Breast Cancer (In Vivo and In Vitro)
Breast cancer progresses from the breast tissue. This type of cancer is the most commonly diagnosed cancer, and it results in 25% of all cases, and it causes 15% of cancer deaths in women worldwide [
106]. The triple-negative breast cancer (TNBC) is the most severe subtype of breast cancer, and it lacks the expression of human epidermal growth factor receptor 2 (HER2), estrogen receptor (ER), and progesterone receptor (PR) [
106]. Symptoms of breast cancer may include a lump in the breast, dimpling of the skin, change in the shape of the breast, red patch of the skin, swollen lymph nodes, shortness of breath, bone pain, discharge of fluid from the nipple, and change in breast size [
107]. Breast cancer is caused by factors, such as lack of exercise, obesity, smoking, ionizing radiation, menstruation at an early age, hormone replacement therapy during menopause, family genetic transmission, etc. [
108]. The currently used breast cancer therapy includes monoclonal antibody therapy, immunotherapy, hormone therapy, radiation therapy, surgery, and chemotherapy [
109]. There are several chemotherapeutic agents that are useful for the treatment of breast cancer, including paclitaxel, docetaxel, doxorubicin, and platinum agents (e.g., cisplatin, etc.) [
110]. They all suffer from severe pharmacological limitations, and hence, there is an urgent need to enhance their chemotherapeutic outcomes by incorporating them into the polymers to form polymer-drug conjugates. Researchers have developed polymer-drug conjugates effective against breast cancer in vitro and in vivo (
Table 2).
Table 2. Summary of polymer-drug conjugates efficacy on breast cancer in vitro and in vivo.
|
Polymer-Drug Conjugates
|
Carrier/
Monomers Used
|
Drugs
|
Biological Outcomes
|
Molecular Design
|
Reference |
|
N-(2-hydroxypropyl methyl) acrylamide copolymer-gadolinium-paclitaxel-Cyanine5.5
|
N-(2-hydroxypropyl methyl) acrylamide
|
Paclitaxel
|
Mode of administration in vivo: Intravenous.
Prolonged residence time, high accumulation of the conjugate at the tumor site. Inhibition of proliferation and induced apoptosis of the 4T1 murine breast cancer cells.
|
The amphiphilic block polymer was prepared via a two-step Reversible Addition-Fragmentation chain Transfer polymerization and self-assembled into a nanoparticle. Enzyme-sensitive tetrapeptide linker was used as a spacer in the conjugate to promote the degradation of high molecular weight conjugates into low molecular weights with the release of the drug in the cancer microenvironment.
|
[111] |
|
Hyaluronic acid-Doxorubicin-Gemcitabine
|
Hyaluronic acid
|
Doxorubicin and gemcitabine
|
Mode of administration in vivo: Intravenous and subcutaneous.
The conjugates loaded with both drugs were active in inhibiting the formation of an orthotopic, aggressive 4T1 tumor model in vivo when compared to individual drugs and the polymer-conjugates loaded with a single drug.
|
The amine on gemcitabine was conjugated to the carboxylic acid on amino acids to form a prodrug. The prodrug was conjugated to hyaluronic acid via carbodiimide chemistry. Doxorubicin was conjugated to hyaluronic acid via carbodiimide chemistry.
|
[112] |
|
PEG-folic acid-trastuzumab
|
Polyethylene glycol
|
Folic acid and trastuzumab
|
The in vitro cellular uptake of the prodrugs conjugated with both drugs was high when compared to the non-targeted polymeric prodrugs. The conjugate displayed apoptosis of 80% with enhanced tumor regression in vivo.
|
The copolymer was prepared
by ring-opening polymerization of PEG and lactide followed by isomerization polymerization of the triblock copolymer and 2-hydroxyethyl disulfide using dibutyltin dilaurate as a catalyst.
|
[113] |
|
N-(2-hydroxypropyl) methacrylamide -Doxorubicin
|
N-(2-hydroxypropyl) methacrylamide
|
Doxorubicin
|
Mode of administration in vivo: Intravenous.
The conjugate exhibited reduced glycolysis, increased apoptosis, and reduced degree of phospholipids when compared to the free doxorubicin. The in vivo studies on the 4T1 breast tumor mouse model using the conjugate revealed a high reduction in the growth of tumors when compared to free DOX-treated mice.
|
DOX was incorporated into the carriers, and enzyme-sensitive tetrapeptide linker was used as a spacer in the conjugate to promote the degradation of high molecular weight conjugates into low molecular weights with the release of the drug in the cancer microenvironment.
|
[114] |
|
Poly-l-glutamic acid-Doxorubicin-Aminoglutethimide
|
Poly-l-glutamic acid
|
Doxorubicin and aminoglutethimide
|
Mode of administration in vivo: Intravenous.
The conjugates displayed enhanced tumor cell death and inhibited tumor-related activities. However, the conjugates containing [N-ε-maleimidocaproic acid hydrazide] moiety displayed a higher survival rate and pro-apoptotic activity, lower anti-apoptotic signals, and inhibition of metastasis.
|
The conjugates loaded with Dox and aminoglutethimide were prepared with pH-sensitive linkers—hydrazine moiety or complex EMCH [N-ε-maleimidocaproic acid hydrazide] moiety—for the release of Dox in the tumor microenvironment.
|
[115] |
|
Polyethylene glycol -Doxorubicin (PEG-DOX)
|
Polyethylene glycol
|
Doxorubicin
|
Mode of administration in vivo: Intraductal.
Increased molecular weight and decreased branching prolonged the retention of the drug in the mammary gland after administration.
|
Dox was conjugated to PEG polymers with varied molecular weights (5, 10, 20, and 40 kDa) and architectures of linear, four-arm, and eight-arm.
|
[116] |
|
Poly(l-glutamic acid)-g-methoxy poly(ethylene glycol) (PLG-g-Mpeg-PTT
|
Poly(l-glutamic acid)-g-methoxy poly(ethylene glycol)
|
Podophyllotoxin
|
The conjugates decreased the hemolytic activity of the drug. The conjugates’ antitumor activity against MCF-7/ADR xenograft tumors was high, with a tumor suppression rate of 82.5%.
|
The drug was conjugated into poly(l-glutamic acid)-g-methoxy poly(ethylene glycol) (PLG-g-mPEG) via ester bonds.
|
[117] |
|
Polyamidoamine-Pamidronate-Platinum (PAMAM-PAM-Pt)
|
Polyamidoamine
|
Pamidronate and platinum
|
The conjugates were not toxic when compared to the free drugs.
|
The conjugates were synthesized by aqueous phase Michael-addition polymerization reaction.
|
[118] |
|
Beta-cyclodextrin- Polyethylene glycol-Folic Acid-doxorubicin (β-CD-PEG-FA-DOX)
|
Polyethylene glycol, Beta-cyclodextrin
|
Doxorubicin
|
Mode of administration in vivo: Intravenous.
Reduced tumor volume, no systemic toxicity, and cardiotoxicity.
|
Beta-cyclodextrin (β-CD)-based carrier was composed of β-CD, polyethylene glycol, and folic acid for enhanced drug delivery.
|
[119] |
|
Methoxy Polyethylene glycol-Polylactic acid-Doxorubicin (mPEG-b-PLA-g-DOX)
|
Polyethylene glycol, Polylactic acid
|
Doxorubicin
|
The cytotoxicity studies showed the cytocompatibility of polymeric carriers to MCF-7 breast cancer cell lines with the viability of cells greater than 80%.
|
The conjugates were prepared by ring-opening polymerization and condensation followed by click reaction. The carriers were grafted with a triazo group. Doxorubicin was modified with cyclooctyne and conjugated to the carriers by strain-promoted alkyne-azide cycloaddition click reaction.
|
[120] |
|
poly(oligoethylene glycol acrylate)
(POEG-VBC-DOX)
|
poly(oligoethylene glycol acrylate)
|
Doxorubicin
|
Mode of administration in vivo: Intravenous.
Synergistic anti-tumor and anti-metastasis activity in vitro and in vivo.
|
DOX was incorporated POEG-VBC backbone.
|
[121] |
|
N-(1,3-dihydroxypropan-2-yl) methacrylamide-Doxorubicin
|
N-(1,3-dihydroxypropan-2-yl) methacrylamide
|
Doxorubicin
|
Extended blood circulation time with an elimination half time of 9.8 h. High accumulation in the tumors and improved in vivo therapeutic efficacy against 4T1 xenograft tumors compared to the free DOX. Tumor inhibition was via inhibition of cell proliferation and antiangiogenic effects.
|
The conjugates were synthesized by RAFT polymerization, followed by drug conjugation.
|
[122] |
|
Polymalic acid-Trastuzumab
|
Polymalic acid
|
Trastuzumab
|
Mode of administration in vivo: Intravenous.
Enhanced tumor growth inhibition.
|
Polyethylene glycol (PEG) and poly (β-l-malic acid)-drug conjugates were prepared by covalently incorporating anti-HER2/neu peptide.
|
[123] |
|
Polyamidoamine-Procaine-Platinum-Alendronate
|
Polyamidoamine
|
Procaine, Platinum (II), Alendronate
|
Selective inhibitory effects of the conjugates towards the cancer cell lines.
|
The conjugates were synthesized by aqueous phase Michael-addition polymerization reaction.
|
[124] |
|
Polyamidoamine-Procaine-Pt-Alendronate
|
Polyamidoamine
|
Ferrocene, Pt (II)
|
Selective inhibitory effects of the conjugates towards the cancer cell lines.
|
The conjugates were synthesized by aqueous phase Michael-addition polymerization reaction.
|
[125] |
5. Polymer-Anticancer Drug Conjugates for Lung Cancer Treatment
Lung cancer is an infectious lung tumor, which is also known as lung carcinoma. It is caused by uncontrollable cell growth in the tissues of the lungs. The cell growth spreads by a process known as metastasis to other parts of the body. There are two types of primary lung cancers: small-cell lung cancer (SCLC) and non-small-cell lung cancer (NSCLC) [
126,
127]. Common symptoms of lung cancer include weight loss, chest pains, short breath, coughing (sometimes coughing blood), etc. [
128]. An estimated 85% majority of patients diagnosed with lung cancer are due to long-term smoking, whereas about 10–15% of patients diagnosed with lung cancer never smoked [
129]. These cases are often caused by a combination of genetic factors and exposure to radon gas, second-hand smoke, asbestos, or exposure to air pollution, etc. Lung cancer can be diagnosed by chest radiographs and computed tomography (CT) scans. Biopsy also confirms the diagnosis of lung cancer, and it is usually performed by bronchoscopy or CT-guidance [
130]. The anticancer drugs used to treat lung cancer suffer from limitations, which can be overcome by polymer-drug conjugates. Some researchers reported the efficacy of polymer-drug conjugates for lung cancer treatment in vitro and in vivo (
Table 3).
Table 3. Summary of polymer-drug conjugates, which are effective in vitro and in vivo against lung cancer.
|
Polymer-Drug Conjugates
|
Carrier/Monomers Used
|
Drugs
|
Biological Outcomes
|
Molecular Design
|
Reference
|
|
Hyaluronic acid-dihydroartemisinin (HA-DHA)
|
Hyaluronic acid
|
Dihydroartemisinin
|
The conjugates displayed high apoptosis when compared to the free drug
|
The hydroxyl group of the drug was covalently linked to the carboxylic group of hyaluronic acid.
|
[131]
|
|
Hyaluronic acid-Paclitaxel (HA-PLX)
|
Hyaluronic acid
|
Paclitaxel
|
Significant cytotoxicity and apoptosis-inducing effect resulting from increased cellular uptake of the drug via HA-receptor mediated endocytosis.
|
Paclitaxel was conjugated to the C-6 position of N-acetyl-D-glucosamine of the hyaluronic acid using hexanediamine as a linker.
|
[132]
|
|
MPEG-b-norbornene functional PLA-b-P(α-BrCL)
|
Polylactic acid, Polyethylene glycol
|
Doxorubicin and paclitaxel
|
The incorporation of both drugs into the carrier resulted in a synergistic effect in inhibiting the proliferation of A549 cancer cells.
|
Both drugs were covalently incorporated into the polymer backbone
|
[133]
|
|
Polylactide-Paclitaxel (PLA-PTX)
|
Allyl-functionalized polylactide
|
Paclitaxel
|
Enhanced cytotoxic effect in vitro.
|
A polymer-drug conjugate was also obtained by thiol-ene reaction of both thiol-functionalized SB and PTX with allyl-functionalized PLA.
|
[134]
|
|
Polyethylene glycol-Paclitaxel (PEG-PTX)
|
Polyethylene glycol
|
Paclitaxel
|
The conjugates exhibited sustained drug release with anti-tumor activity, which was less than the free drugs.
|
The conjugates were prepared with either an azide linker or a succinic linker. The linear PEGs were modified with PTX at the hydroxyl. PTX was incorporated into the PEG molecule via an ester bond at the C-2′ position on the PTX side chain.
|
[135]
|
|
N-(2-hydroxypropyl)methacrylamide-Doxorubicin
|
N-(2-hydroxypropyl)methacrylamide
|
Doxorubicin
|
High cytotoxic activity against the lung cancer cells, which were 10-fold higher cytotoxic against B16-F10, 3LL, and HT29 cells when compared to peptide-doxorubicin.
|
Doxorubicin was incorporated into N-(2-hydroxypropyl)methacrylamide.
|
[136]
|
|
Poly-l-lysine-lipoic acid-Doxorubicin
|
Poly-l-lysine-lipoic acid
|
Doxorubicin
|
The conjugates exhibited enhanced internalization and cytotoxicity effects in vitro. It also exhibited excellent good tumor-targeting capability.
|
It was prepared by the modification of dimethylmaleic anhydride for enhanced cell internalization
|
[137]
|
This entry is adapted from the peer-reviewed paper 10.3390/pharmaceutics12050406