2. Patients Centered Conversation on End-of-Life Care
The debilitating symptoms of COPD have a significant impact on the lives of patients with COPD and lead to decreased quality of life [
73]. These symptoms include breathlessness, cough, pain, anorexia, fatigue, and psychological symptoms [
74]. The burden of these symptoms is high and thus patients with advanced COPD symptoms should be informed of the benefits of end-of-life and palliative care. Palliative care not only reduces COPD symptoms leading to increased quality of life, but can also decrease the use of invasive procedures, increase psychosocial support and mood, and decrease health care costs. Many patients may also benefit from the early introduction of palliative care before severe symptoms are present [
73]. As each person’s COPD is different, a patient-centered management plan is important. A patient-centered COPD treatment team may include a primary care physician, pulmonologist, respiratory therapist, dietician or nutritionist, therapist or counselor, and palliative care specialist [
75,
76]. Patients’ family members need to be involved as part of the treatment team for COPD patients, as they can be an extension of the physician’s voice. Family members and caregivers can be very instrumental in monitoring COPD patients’ treatment management plan by making sure the patient takes his or her medications, recognizes signs of exacerbation, and helps them to carry out tasks in the home environment. For patients with advanced COPD, a family member can act on behalf of the patient [
77].
However, the lack of an effective end-of-life care strategy for patients with advanced COPD may bring dissatisfaction to the patients and relevant stakeholders associated with the treatment and palliative care. One of the main reasons for dissatisfaction or poor outcome of end-of-life care is the lack of good communication between patients, families, and physicians while planning for the advanced directives [
8,
78]. Studies show that advanced directives are useful among patients with COPD because of their likely illness, potential risk for severe illness, and sudden death of critically ill patients due to disease exacerbation [
79]. In some cases, patients with COPD may have an opinion about the decision to forgo CPR and mechanical ventilation for acute respiratory failure [
80]. Several studies have suggested that advanced directives can reduce stress among family members of dying patients [
81,
82].
Many clinicians acknowledge the importance of end-of-life planning early in the process of COPD, however; for chronic respiratory diseases, such as COPD, advanced care planning is rare [
83]. Furthermore, it appears that patients diagnosed with COPD often “underutilize” palliative care when compared to other lung diseases such as lung cancer and thus may have “worse dying experiences” [
84]. Patients with advanced COPD are more likely to undergo invasive procedures such as mechanical ventilation and are less likely to receive hospice care and end-of-life planning compared to patients with lung cancer [
85]. Thus, delaying access to end-of-life care reduces the ability to increase the quality of life and promote end-of-life discussions [
83].
Clinicians play a central role in the quality of care received during the end stages of COPD, but there are major barriers that they face toward providing quality end-of-life care for patients with advanced COPD. These barriers include a lack of continuity of care affecting the relationship of physicians and patients, as well as a lack of education on the roles and goals of palliative care. Most patients would like to receive comprehensive and accurate information about disease progression, treatment options, and prognosis; however, this information is often lacking [
73]. Pulmonologists have skills and expertise for overcoming difficulties in COPD diagnosis and for providing the best treatment for managing COPD. Many pulmonology providers have acknowledged misconceptions toward palliative care, including the fear that palliative care clinicians would manage symptoms with high doses of opioids and benzodiazepines. Other barriers include a lack of education regarding when and how to have end-of-life discussions with patients [
83]. Poor communication is more likely to lead to poor palliative care in COPD [
8]. Despite these barriers, it has been shown that COPD patients benefit from prompt access to palliative care [
74]. The goal of palliative care is to prevent and relieve suffering from COPD exacerbation regardless of the stage of the disease [
86]. However, the unpredictable nature of disease progression in patients with COPD makes proper planning of end-of-life care difficult. This unpredictability is further complicated during periods of acute exacerbations, where an initial complaint of respiratory discomfort can progress rapidly into respiratory failure. This often puts the patient in an incapacitated state, depriving them of the opportunity to actively participate in the process of end-of-life care planning. For this reason, improving prognostication skills is key, so clinicians may identify COPD patients that are at greater risk for worse outcomes, and promptly commence end-of-life care planning from the initial encounter [
87].
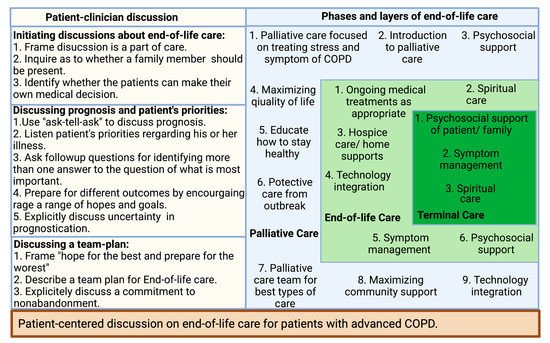
Many clinicians find communicating about end-of-life care difficult due to the nature of the discussion, especially with patients in the early stages of COPD. Therefore, adopting the right communication technique is crucial in the overall improvement of end-of-life care (
Figure 1) [
8]. Patients with COPD more than often want to know information about five specific areas: diagnosis and disease process, treatment, prognosis, what dying might be like, and advance care planning [
8]. There are several published studies that provide some specific directions for clinicians in their communications about end-of-life discussion to their patients with advanced COPD. For example, most COPD patients would like more information about prognosis, while patients with advanced COPD and limited life expectancy want to know more about their life expectancy [
88,
89,
90]. It is not unusual that family members request this information even the patient themself does not want to know [
91]. Therefore, clinicians should be aware of patients’ and family members’ interests in obtaining information about the disease. It has been found that describing information about a disease with numeric experiences of risk (e.g., eight out of ten people will have side effects from this drug) allowed for better comprehension than describing information about a disease with qualitative expressions of risk [
92].
Figure 1. Patient-centered discussion on end-of-life care for patients with advanced COPD.
Patients with COPD may receive poor-quality palliative care due to the lack of patient–physician communication about end-of-life care, or if it occurs too late in the illness [
93,
94,
95]. By understanding the barriers to communication, clinicians can improve patient–clinician discussions about end-of-life care [
8]. A recent study suggests that inpatient palliative care consultation has a positive impact on patient outcomes and transitions to the community [
96]. A short survey from both pulmonary and palliative clinicians suggested early care adds value to disease-focused COPD care. In the study, the clinicians from both specialties not only supported early palliative care in COPD but also emphasized addressing pulmonologists’ misconception of palliative care, establishing consensus referral criteria, and executing a novel early palliative care model [
83]. Clinicians should be prepared to listen and provide appropriate information in the most caring and respectful manner. Practical strategies that can be employed begin with building a relationship based on trust between a COPD patient and their provider. Discussions about end-of-life care must be initiated during the early course of the disease focusing on the implication of the patient’s diagnosis and interventions to be taken at every step of disease progression [
97]. A phased introduction of supportive and palliative care can be triggered at key disease milestones during a lifelong journey with COPD, especially during an inpatient visit for an exacerbation [
98]. To ensure patients’ wishes regarding end-of-life care are current, the advanced care directive should be reviewed at every visit [
97]. Clinician–patient conversations can bring a successful end-of-life care plan with active participation by patients, clinicians, and caregivers (
Figure 1) [
8].