The term telemedicine was to describe the practice of delivering health care services through the use of information and communications technology, whereby geographic distance is not as constraining, as in the case of traditional medical practice. Telemedicine is not only used to exchange valid information for the diagnosis, treatment, and prevention of disease and injuries and research and evaluation, but also for the continuing the education of healthcare providers to advance individual and community health.
1. Introduction
Telemedicine has been shown to improve access to healthcare and reduce costs, especially in areas with a limited healthcare infrastructure due to geographical barriers [1]. Recently, increased digitalization and the development of telehealth applications have finally reached the field of medical imaging. As telemedicine has evolved over the last few decades, ultrasound technology matured in parallel [2]. Ultrasound became a bedside tool in the 1990s that physicians, such as those who work in the emergency department, could use regularly because it is a fast, robust, and reliable way of determining a patient’s status at the outset of treatment. Tele-ultrasound is defined as the use of ultrasound with telecommunications and/or an additional instructor who is telemedically connected to the process. The utilization of tele-ultrasound has been rapidly increasing worldwide since the 1990s and is commonly used for emergency, abdominal, and obstetrical ultrasound by general practitioners in remote areas worldwide. One of the beneficiaries of this is other doctors, but in a broader sense, it benefits patients as well. Moreover, it can be a cost-saving measure as it eliminates both long transportation times and extra doctor visits. A lack of access to ultrasound doctors, despite technological advancements and mobile devices with high bandwidth that allow for seamless live-image transmission, is a concern in both low-income and high-income countries. Moreover, the main challenge in telemedicine remains an organizational one, knowing how and when to take advantage of the technology.
2. Practicality of Use
Tele-ultrasound can be used in urban as well as in rural areas. It can improve the healthcare system and patient outcomes, especially in under-resourced areas
[3]. From the point of view of medical education, it can enhance ultrasound skills and establish a basic knowledge of ultrasound. By expanding this method with tele-applications, practical ultrasound could be taught anywhere in the world.
In times of pandemics, such as COVID-19, with social distancing regulations and isolation measures, it can help to ease the pressure on healthcare systems by providing diagnostic alternatives. Rapid technical development and competition in the field of medical software engineering have made the cost of tele-ultrasound manageable. Even low-cost, readily available tools such as web interfaces or commercial messenger tools can be used for tele-supported ultrasound, with the advantage of being independent of any special setting and providing the flexibility to perform ultrasound when and wherever it may be necessary
[4]. Recently, new software applications have been introduced that support the teaching of knobology and handling of the probe. Thus, one can even practice at home, independently of any course sessions (
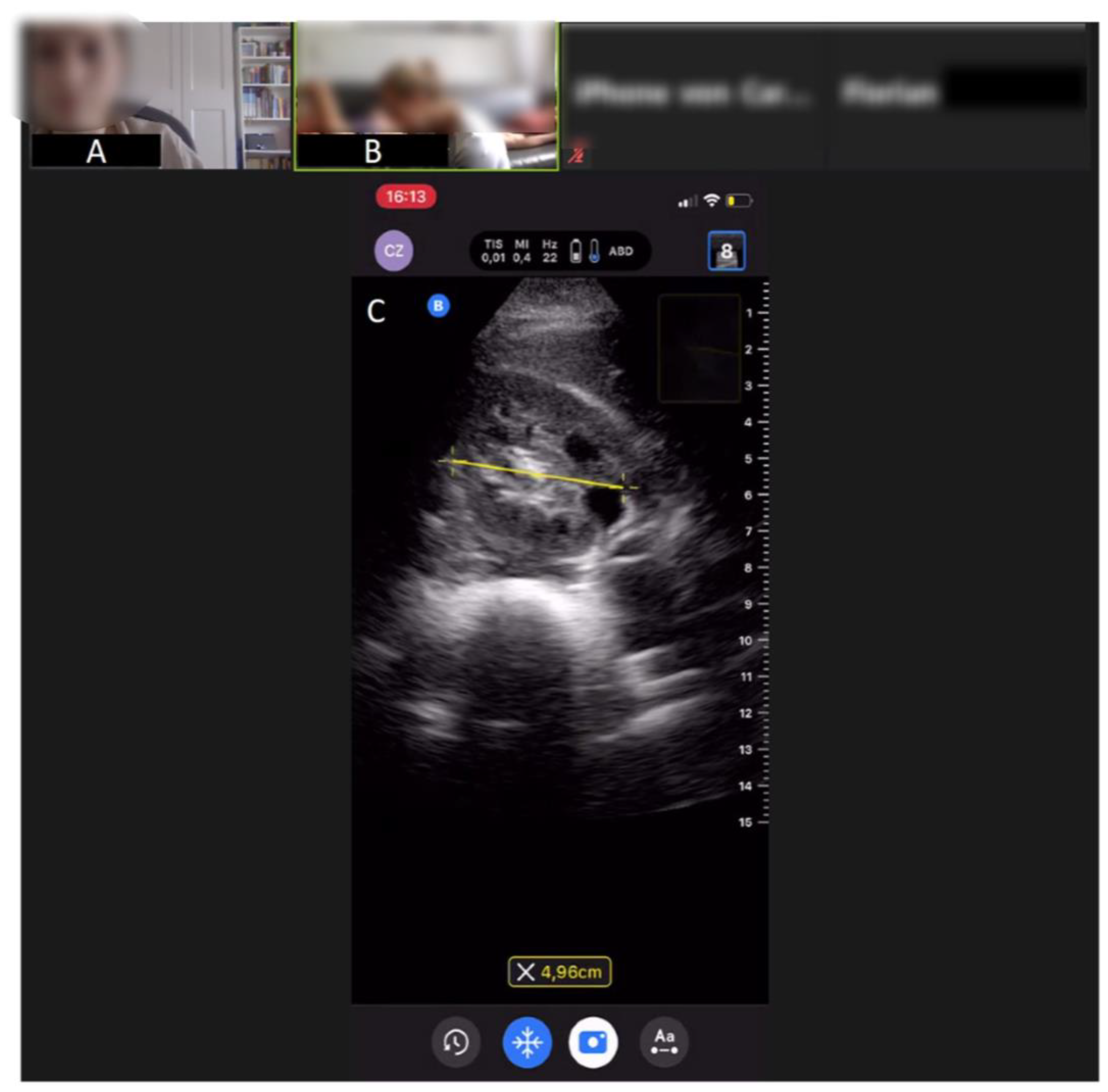
Figure 1).
Figure 1. Ultrasound image from a tele-didactic ultrasound teaching study on abdominal ultrasound from the medical faculty of the University of Bonn, Germany. (A) Peer tutor, (B) student exercising ultrasound on another student, (C) ultrasound image of the right kidney, which will be improved via tele-guidance by the peer tutor. An experienced ultrasonographer is also online in order to assist if any questions arise.
3. Cost Efficiency
In the scenario of real-time tele-ultrasound consultations and tele-education, savings in the conventional costs of patient transfer (e.g., transfer from GP to clinic) and human resources (e.g., clinical specialist in remote areas) need to be balanced against accruing telecommunication costs. An Australian study demonstrated that tele-ultrasound can result in a net saving of AUD 6340 and, at the same time, enabled almost four times the number of consultations than if the service had not been available
[5]. A real-time fetal tele-ultrasound consultation service had been implemented and integrated into the daily clinical practice. Patients in Townsville could be assessed by subspecialists in Brisbane, 1500 km away, using the service. Ninety percent of the babies born during the 90 tele-ultrasound consultations for the first 71 patients showed good outcome data. The existence of all key anomalies and diagnoses was established. Without telemedicine, 24 of the 71 patients would have been physically referred to Brisbane. Thus, underlined the cost effectiveness of the practice in a rural region.
As technology improves, wireless networks and cell phone access become more reliable, and companies such as Apple, Skype and many start-ups provide commercially available real-time audiovisual software in compliance with patient protection laws such as the American HIPAA (“Health Insurance Portability and Accountability Act”), making tele-ultrasound a feasible proposition.
Cost is a commonly expressed concern regarding tele-ultrasound with a special emphasis on the need for affordable tele-ultrasound platforms to make its use feasible. In the literature, numerous studies have used telemedicine platforms with open-source, low-cost, commercially available software such as over-the-counter hardware and low-cost portable ultrasound machines to minimize costs. Two studies explored the issue from the patients’ perspective and found that the introduction of tele-ultrasound was associated with lower out-of-pocket costs for the patient due to a reduced need for travel to larger medical centers with formal imaging capacity
[6][7]. In another study, e-learning was found to be more effective than conventional education and superior to self-learning for enhancing novice learners’ ultrasound technical skills without increasing their workload
[8].
4. Medical Education
In terms of medical education, e-learning can serve as both a self-study tool, as well as a teaching device, when used in conjunction with colleagues or supervisors. With the emergence of faster network technology (5G/6G) and mobile app platforms for live interaction and handheld ultrasound devices, tele-ultrasound and new fields of applications in pre-clinical settings and outpatient areas such as midwifery, geriatric facilities, and therapeutic use will be enabled with these developments
[9].
The existing literature indicates that e-learning can provide an effective way of improving educational outcomes for healthcare professionals. Several studies have shown that tele-learning methods lead to similar results to traditional, face-to-face, teacher-centered instruction
[10]. Especially when it comes to the field of tele-ultrasound, didactic concepts are particularly important. Theoretical ultrasound knowledge can be learned using a “flipped classroom”, a didactic format of blended learning, whereby students acquire knowledge at home and put it into practice during classes. In the past, attempts to offer targeted, individualized learning environments were abandoned due to the excessive expenditure of money. Nowadays, software-based, highly individualized learning is the norm rather than the exception and has shifted the paradigm. In this ongoing educational evolution, tele-ultrasound devices have several crucial advantages over traditional stationary ultrasound systems. Tele-ultrasound devices are connected to the internet, and interaction between every active participant is made easier, which simplifies communication and ideally speeds up the learning process. The internet, of course, provides access to a plethora of teaching and learning software. The combination of being continuously interconnected, elaborate software, and sufficient computing power has paved the way towards a personalized learning experience. The latest applications and web-based learning platforms can observe and track user profiles. In this way, individual learning behavior can be analyzed and optimized. Especially, theoretical ultrasound knowledge and knobology can be taught in this manner.
However, practical tele-guided ultrasound teaching and assessment comes with costs and challenges. In addition to purchasing the ultrasound equipment, the teacher and student need a video-based platform to show and see the student’s performance and the position of the transducer. Furthermore, the real-time sonogram must be streamed in order to give the student instructions during the training. However, the limited evidence base of this relatively new field of medical education demands further research to corroborate its efficacy in comparison with conventional teaching methods.
The most common components such as the handling and orientation of the probe, as well as image adjustments, may be evaluated with video footage that is recorded and reviewed afterwards or via a live stream.
These applications can be upgraded by augmented reality devices and experimental visual guidance tools that enhance the tele-guided experience and enable a more realistic method of learning
[11]. Visual guidance is a computer-assisted method of demonstrating to an examiner the movement of the ultrasound probe as it is manipulated over a patient’s body toward a desired anatomical location.
The latest technical advancement in the field of tele-ultrasound is tele-guided ultrasound, which enhances and enables tele-educational tools in a more precise way. Tele-guided ultrasound means that someone is controlling the ultrasound probe and has access to all device settings remotely. For assessing not only image quality, but also the proficiency of the tele-mentored ultrasound image acquisition some studies have combined different tools.
Furthermore, progress is being made in educational tele-guidance tools. These serve as image quality indicators that provide real-time feedback from the physician on the healthcare worker’s scan technique. These tools aim to improve the quality and speed of the captured images. Thus, education in medical ultrasound can be expanded in remote areas if basic equipment (US machine, Internet, and telemedicine software) is available.
As an example of the use of tele-ultrasound in medical teaching, a tele-didactic ultrasound course was designed by Höhne et al.
[12] in light of the current COVID-19 pandemic and the end of classical classroom teaching, which was previously considered vital in ultrasound training. It was to determine if online ultrasound teaching was effective. It also aimed to identify a suitable evaluation approach for evaluating US skills from afar. It demonstrated the effectiveness of online lectures in the context of ultrasound medical education. Furthermore, it illustrates that teleguided ultrasound training is feasible and should be addressed in medical schools, as well as the learning possibilities of tele-digital ultrasound.
5. Image Quality
A quality assessment tool was developed a few years ago to standardize sonographic B-images
[13]. As an important feature, it attempts to quantify the sonographer’s influence with regard to the final image quality. This method can also be adopted for tele-ultrasound. Furthermore, the examiner’s skill, as well as the patient’s current state and cooperation, are all known to influence ultrasound imaging. Gallstones, for example, may only be scanned when the patient is in a precise inspiratory position and with extremely specific transducer angles and placements. As a result, even in the absence of tele-transmission, the imaging result is not always consistent. When two examiners look at the same patient, they will almost always produce different visuals and, in some situations, diagnoses. This general weakness naturally also has an influence on the use of ultrasound in telemedicine and must always be taken into account in all applications.
The latest developments in the field of telecommunication have paved the way for several attempts to test tele-ultrasound with mobile device application
[9] or via web-based applications
[14]. These studies have shown that commercially available video chat software can transmit high-quality and clinically useful ultrasound images. For nearly every anatomic location assessed in these studies, images obtained by means of this method were non-inferior to images obtained directly from a stationary ultrasound machine. There were also mobile ultrasound apps that went beyond simply projecting live images, with built-in tools to grade the images that study participants took and determined whether they passed or failed.
Data transfer rates have come a long way since the early stages of telemedicine two decades ago, when devices with a bandwidth of 2 Mbit/s were used successfully for obstetric tele-ultrasound
[6]. Nowadays, the transmission of real-time ultrasound video footage to a remote iPhone using inexpensive technology is feasible, as shown in the literature. It can be accomplished without the loss of image quality and a minimal delay and works even with 3G mobile connection
[15].
6. Safety of Data
As the value of personalized data increases and cheap data storage is abundantly available, telemedicine companies can record and analyze a complete set of parameters longitudinally in real-time, which is an unprecedented feat in the history of medicine. However, patients’ access to and control over these stored data are not always guaranteed. In Western societies, where people are wary of privacy violations, these developments should spark an intense public discourse, which seems to lag behind the staggering pace of the technological advancement.
In a tele-guided setting, there are several ways to document the obtained images and results. There are various ultrasound documentation programs on portable devices and guidelines on how to appropriately document an ultrasound examination
[16]. Moreover, there are cloud-based monitoring systems that do not require bedside supervision and documentation, which may enhance the ability of physicians to study and document ultrasound images
[17]. Data protection is an important issue related to these cloud-based documentation applications. Although recent cloud-based products comply with EU regulations regarding data privacy and protection, this remains a hot topic.
This entry is adapted from the peer-reviewed paper 10.3390/app12030958