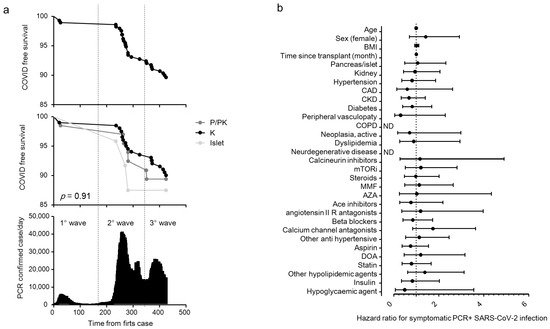
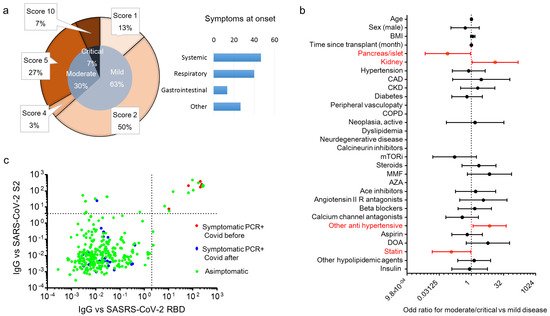
It is still uncertain whether recipients of solid organ transplant (SOT) are at increased risk of SARS-CoV-2 infection and/or poor outcomes due to COVID-19 in comparison to the general population. In this study, we report the cumulative incidence and outcomes of SARS-CoV-2 infection in a cohort of 291 SOT recipients. The COVID-19 cumulative incidence in SOT recipients resulted slightly higher compared to that of age-matched population during the study period. Moreover, the SARS-CoV-2 antibody frequency was around 2.6-fold higher than the incidence of cases who tested positive for SARS-CoV-2 RT-PCR, suggesting that the number of SOT recipients infected with SARS-CoV-2 is likely higher than described. In symptomatic recipients, kidney transplant was associated with a higher risk of developing moderate/critical disease, while common risk factors, including age and comorbidities, resulted less relevant for COVID-19 severity. Due to the high estimated crude mortality, symptomatic SOT recipients should be considered at high risk in case of SARS-CoV-2 infection.
- COVID-19
- pancreas transplantation
- islet transplantation
- seroprevalence
- SARS-CoV-2
1. Introduction
2. Current Researches and Results
| Items | All | Islet | Pancreas ± Kidney | Kidney | p |
|---|---|---|---|---|---|
| N | 291 | 24 | 66 | 201 | |
| Age in years, median (IQR) | 56 (47–65) | 51 (36–60) | 54 (47–59) | 57 (49–66) | 0.001 |
| Sex M/F | 179/112 | 11/13 | 41/25 | 127/74 | 0.264 |
| Race Caucasian (N (%)) | 284 (97.6) | 24 (100) | 64 (97) | 196 (97.5) | 0.631 |
| Body mass index (kg/m2) | 24.2 (21.8–26.6) | 22.2 (17.8–23.5) | 23.2 (20–26.7) | 25 (22.5–27) | <0.001 |
| Months since transplant, median (IQR) | 53.4 (17–121) | 79 (34–131) | 75 (24–160) | 48 (12–106) | 0.005 |
| Comorbidities (N (%)) | |||||
| Hypertension | 227 (78) | 11 (45.8) | 42 (63.6) | 174 (86.6) | <0.001 |
| Coronary artery disease | 35 (12) | 2 (8.3) | 11 (16.7) | 22 (10.9) | 0.392 |
| Chronic kidney disease | 156 (53.6) | 2 (8.3) | 29 (43.9) | 125 (62.2) | <0.001 |
| Diabetes | 140 (48.1) | 24 (100) | 66 (100) | 50 (24.9) | <0.001 |
| Peripheral vasculopathy | 30 (10.3) | 1 (4.2) | 7 (10.6) | 22 (10.9) | 0.585 |
| Chronic obstructive pulmonary disease | 1 (0.3) | 0 (0) | 0 (0) | 1 (0.5) | 0.799 |
| Neoplasia active | 27 (9.3) | 1 (4.2) | 3 (4.5) | 23 (11.4) | 0.164 |
| Dyslipidemia | 35 (12) | 2 (8.3) | 5 (7.6) | 28 (13.9) | 0.327 |
| Neuro degenerative disease | 2 (0.7) | 1 (4.2) | 1 (1.5) | 0 (0) | 0.043 |
| Baseline therapy | |||||
| Calcineurin inhibitor (CNI) | 270 (92.8) | 21 (87.5) | 64 (97) | 185 (92) | 0.235 |
| Mammalian target of rapamycin inhibitors (mTORi) | 58 (19.9) | 9 (37.5) | 3 (4.5) | 46 (22.9) | <0.001 |
| Steroids | 133 (45.7) | 1 (4.2) | 31 (47) | 101 (50.2) | <0.001 |
| Mycophenolate mofetil | 218 (74.9) | 11 (45.8) | 59 (89.4) | 148 (73.6) | <0.001 |
| Azathioprine | 18 (6.2) | 6 (25) | 4 (6.1) | 8 (4) | <0.001 |
| “Intensity” of immunosuppression | |||||
| - Triple regimen | 122 (41.9) | 1 (4.2) | 30 (45.5) | 91 (45.3) | |
| ○ CNI+antimetabolite+steroid | 102 (83.6) | 0 (0) | 28 (93.3) | 74 (81.3) | |
| ○ CNI+mTORi+steroid | 14 (11.5) | 0 (0) | 1 (3.3) | 13 (14.3) | |
| ○ mTORi+antimetabolite+steroid | 5 (4.1) | 0 (0) | 1 (3.3) | 4 (4.4) | |
| ○ mTORi+CNI+antimetabolite | 1 (0.8) | 1 (100) | 0 (0) | 0 (0) | |
| - Double regimen | 162 (55.7) | 22 (91.7) | 36 (54.5) | 104 (51.7) | |
| ○ CNI+antimetabolite | 118 (72.8) | 13 (59.1) | 34 (94.4) | 71 (68.3) | |
| ○ CNI+mTORi | 28 (17.3) | 6 (27.3) | 0 (0) | 22 (21.2) | |
| ○ CNI+steroid | 5 (3.1) | 1 (4.5) | 1 (2.8) | 3 (2.9) | |
| ○ mTORi+steroid | 5 (3.1) | 0 (0) | 0 (0) | 5 (4.8) | |
| ○ mTORi+antimetabolite | 4 (2.5) | 2 (9.1) | 1 (2.8) | 1 (1) | |
| ○ antimetabolite+steroid | 2 (1.2) | 0 (0) | 0 (0) | 2 (1.9) | |
| - Single regimen | 7 (2.4) | 1 (4.2) | 0 (0) | 6 (3) | |
| ○ Antimetabolite | 4 (57.1) | 1 (100) | 0 (0) | 3 (50) | |
| ○ CNI | 2 (28.6) | 0 (0) | 0 (0) | 2 (33.3) | |
| ○ mTORi | 1 (14.3) | 0 (0) | 0 (0) | 1 (16.7) | |
| Ace inhibitors | 51 (17.5) | 6 (25) | 7 (10.6) | 38 (18.9) | 0.185 |
| Angiotensin II receptor type 1 antagonists | 26 (8.9) | 1 (4.2) | 5 (7.6) | 20 (10) | 0.584 |
| Beta blockers | 157 (54) | 6 (25) | 33 (50) | 118 (58.7) | 0.006 |
| Calcium channel antagonists | 125 (43) | 3 (12.5) | 26 (39.4) | 96 (47.8) | 0.003 |
| Other anti-hypertensive | 106 (36.4) | 2 (8.3) | 20 (30.3) | 84 (41.8) | 0.003 |
| Aspirin | 185 (63.6) | 6 (25) | 45 (68.2) | 134 (66.7) | <0.001 |
| Direct oral anticoagulant | 44 (15.1) | 4 (16.7) | 12 (18.2) | 28 (13.9) | 0.688 |
| Statin | 134 (46) | 7 (29.2) | 27 (40.9) | 100 (49.8) | 0.102 |
| Other hypolipidemic agents | 61 (21) | 2 (8.3) | 8 (12.1) | 51 (25.4) | 0.02 |
| Insulin | 69 (23.7) | 18 (75) | 19 (28.8) | 32 (15.9) | <0.001 |
| Hypoglycemic agent | 19 (6.5) | 0 (0) | 5 (7.6) | 14 (7) | 0.395 |
| Items | SARS-CoV-2 RT-PCR Negative | SARS-Cov-2 RT-PCR Positive | p |
|---|---|---|---|
| N | 261 | 30 | |
| Age in years, median (IQR) | 56 (47–65) | 52 (48–61) | 0.341 |
| Sex M/F | 163/98 | 16/14 | 0.331 |
| Race Caucasian (N (%)) | 256 (98.1) | 28 (93.3) | 0.156 |
| Body mass index (kg/m2) | 24.2 (21.8–26.6) | 24 (21.9–26.9) | 0.817 |
| Type of transplant | |||
| - Kidney | 181 (69.3) | 20 (66.7) | 0.924 |
| - Pancreas ± kidney | 59 (22.6) | 7 (23.3) | |
| - Islets | 21 (8) | 3 (10) | |
| Comorbidities (N (%)) | |||
| - Hypertension | 205 (78.5) | 22 (73.3) | 0.492 |
| - Coronary artery disease | 33 (12.6) | 2 (6.7) | 0.552 |
| - Chronic kidney disease | 143 (54.8) | 13 (43.3) | 0.251 |
| - Diabetes | 127 (48.7) | 13 (43.3) | 0.7 |
| - Peripheral vasculopathy | 29 (11.1) | 1 (3.3) | 0.337 |
| - Chronic obstructive pulmonary disease | 1 (0.4) | 0 (0) | 1 |
| - Neoplasia active | 25 (9.6) | 2 (6.7) | 1 |
| - Dyslipidemia | 32 (12.3) | 3 (10) | 1 |
| - Neuro degenerative disease | 2 (0.8) | 0 (0) | 1 |
| Baseline therapy | |||
| - Calcineurin inhibitor (CNI) | 242 (92.7) | 28 (93.3) | 1 |
| - Mammalian target of rapamycin inhibitors (mTORi) | 51 (19.5) | 7 (23.3) | 0.631 |
| - Steroids | 119 (45.6) | 14 (46.7) | 1 |
| - Antimetabolites | 211 (80.8) | 25 (83.3) | 1 |
| “Intensity” of immunosuppression | |||
| - Triple regimen | 108 (41.4) | 14 (46.7) | 0.421 |
| - Double regimen | 146 (55.9) | 16 (50.2) | |
| - Single regimen | 7 (2.7) | 0 (0) |
This entry is adapted from the peer-reviewed paper 10.3390/biology10121349
References
- Unim, B.; Palmieri, L.; Lo Noce, C.; Brusaferro, S.; Onder, G. Prevalence of COVID-19-related symptoms by age group. Aging Clin. Exp. Res. 2021, 33, 1145–1147.
- Palmieri, L.; Vanacore, N.; Donfrancesco, C.; Lo Noce, C.; Canevelli, M.; Punzo, O.; Raparelli, V.; Pezzotti, P.; Riccardo, F.; Bella, A. Clinical characteristics of hospitalized individuals dying with COVID-19 by age group in Italy. J. Gerontol. Ser. A 2020, 75, 1796–1800.
- Wingert, A.; Pillay, J.; Gates, M.; Guitard, S.; Rahman, S.; Beck, A.; Vandermeer, B.; Hartling, L. Risk factors for severity of COVID-19: A rapid review to inform vaccine prioritisation in Canada. BMJ Open 2021, 11, e044684.
- Azzi, Y.; Bartash, R.; Scalea, J.; Loarte-Campos, P. Akalin E COVID-19 and Solid Organ Transplantation: A Review Article. Transplantation 2021, 105, 37–55.
- Pereira, M.R.; Mohan, S.; Cohen, D.J.; Husain, S.A.; Dube, G.K.; Ratner, L.E.; Arcasoy, S.; Aversa, M.M.; Benvenuto, L.J.; Dadhania, D.M.; et al. COVID-19 in solid organ transplant recipients: Initial report from the US epicenter. Am. J. Transpl. 2020, 20, 1800–1808.
- Akalin, E.; Azzi, Y.; Bartash, R.; Seethamraju, H.; Parides, M.; Hemmige, V.; Ross, M.; Forest, S.; Goldstein, Y.D.; Ajaimy, M.; et al. Covid-19 and Kidney Transplantation. N. Engl. J. Med. 2020, 382, 2475–2477.
- Caillard, S.; Anglicheau, D.; Matignon, M.; Durrbach, A.; Greze, C.; Frimat, L.; Thaunat, O.; Legris, T.; Moal, V.; Westeel, P.F.; et al. An initial report from the French SOT COVID Registry suggests high mortality due to COVID-19 in recipients of kidney transplants. Kidney Int. 2020, 98, 1549–1558.
- Roberts, M.B.; Izzy, S.; Tahir, Z.; Al Jarrah, A.; Fishman, J.A.; El Khoury, J. COVID-19 in solid organ transplant recipients: Dynamics of disease progression and inflammatory markers in ICU and non-ICU admitted patients. Transpl. Infect. Dis. 2020, 22, e13407.
- Fishman, J.A. The Immunocompromised Transplant Recipient and SARS-CoV-2 Infection. J. Am. Soc. Nephrol. 2020, 31, 1147–1149.
- Fernandez-Ruiz, M.; Andres, A.; Loinaz, C.; Delgado, J.F.; Lopez-Medrano, F.; San Juan, R.; Gonzalez, E.; Polanco, N.; Folgueira, M.D.; Lalueza, A.; et al. COVID-19 in solid organ transplant recipients: A single-center case series from Spain. Am. J. Transpl. 2020, 20, 1849–1858.
- Crespo, M.; Perez-Saez, M.J.; Redondo-Pachon, D.; Llinas-Mallol, L.; Montero, M.M.; Villar-Garcia, J.; Arias-Cabrales, C.; Buxeda, A.; Burballa, C.; Vazquez, S.; et al. COVID-19 in elderly kidney transplant recipients. Am. J. Transpl. 2020, 20, 2883–2889.
- Kates, O.S.; Haydel, B.M.; Florman, S.S.; Rana, M.M.; Chaudhry, Z.S.; Ramesh, M.S.; Safa, K.; Kotton, C.N.; Blumberg, E.A.; Besharatian, B.D.; et al. COVID-19 in solid organ transplant: A multi-center cohort study. Clin. Infect. Dis. 2020, 73, 4090–4099.
- Aversa, M.; Benvenuto, L.; Anderson, M.; Shah, L.; Robbins, H.; Pereira, M.; Scheffert, J.; Carroll, M.; Hum, J.; Nolan, M.; et al. COVID-19 in lung transplant recipients: A single center case series from New York City. Am. J. Transpl. 2020, 20, 3072–3080.
- Cravedi, P.; Mothi, S.S.; Azzi, Y.; Haverly, M.; Farouk, S.S.; Perez-Saez, M.J.; Redondo-Pachon, M.D.; Murphy, B.; Florman, S.; Cyrino, L.G.; et al. COVID-19 and kidney transplantation: Results from the TANGO International Transplant Consortium. Am. J. Transpl. 2020, 20, 3140–3148.
- Avery, R.K.; Chiang, T.P.; Marr, K.A.; Brennan, D.C.; Sait, A.S.; Garibaldi, B.T.; Shah, P.; Ostrander, D.; Steinke, S.M.; Permpalung, N.; et al. Inpatient COVID-19 outcomes in solid organ transplant recipients compared to non-solid organ transplant patients: A retrospective cohort. Am. J. Transpl. 2021, 21, 2498–2508.
- Bossini, N.; Alberici, F.; Delbarba, E.; Valerio, F.; Manenti, C.; Possenti, S.; Econimo, L.; Maffei, C.; Pola, A.; Terlizzi, V.; et al. Kidney transplant patients with SARS-CoV-2 infection: The Brescia Renal COVID task force experience. Am. J. Transpl. 2020, 20, 3019–3029.
- Fava, A.; Cucchiari, D.; Montero, N.; Toapanta, N.; Centellas, F.J.; Vila-Santandreu, A.; Coloma, A.; Meneghini, M.; Manonelles, A.; Sellares, J.; et al. Clinical characteristics and risk factors for severe COVID-19 in hospitalized kidney transplant recipients: A multicentric cohort study. Am. J. Transpl. 2020, 20, 3030–3041.
- Molnar, M.Z.; Bhalla, A.; Azhar, A.; Tsujita, M.; Talwar, M.; Balaraman, V.; Sodhi, A.; Kadaria, D.; Eason, J.D.; Hayek, S.S.; et al. Outcomes of critically ill solid organ transplant patients with COVID-19 in the United States. Am. J. Transpl. 2020, 20, 3061–3071.
- Avery, R.K. COVID-19 Therapeutics for Solid Organ Transplant Recipients; 6 Months Into the Pandemic: Where Are We Now? Transplantation 2021, 105, 56–60.
- Hadi, Y.B.; Naqvi, S.F.Z.; Kupec, J.T.; Sofka, S.; Sarwari, A. Outcomes of COVID-19 in Solid Organ Transplant Recipients: A Propensity-matched Analysis of a Large Research Network. Transplantation 2021, 105, 1365–1371.
- Marshall, J.C.; Murthy, S.; Diaz, J.; Adhikari, N.K.; Angus, D.C.; Arabi, Y.M.; Baillie, K.; Bauer, M.; Berry, S.; Blackwood, B.; et al. A minimal common outcome measure set for COVID-19 clinical research. Lancet Infect. Dis. 2020, 20, 192–197.
