Neuroblastoma is the most common extracranial solid tumor of childhood, with a median age at diagnosis of 17 months. Its incidence is 10.2 cases per million children aged <15 years. Neuroblastoma arises in tissues of the sympathetic nervous system, mostly in the adrenal medulla or paraspinal ganglia. It appears as a mass in the abdomen, pelvis, neck, or chest, with about half of the patients having metastatic disease at diagnosis. The presence of metastatic diseases over the age of 12 or 18 months and aggressive biological features (e.g., MYCN oncogene amplification) define high-risk neuroblastoma. The prognosis for such patients is poor, with a long-term survival rate of only 40%.
- dinutuximab
- neuropathic pain
- peripheral neuropathy
- neuroblastoma
- pediatric cancer
- molecular mechanisms
- treatment
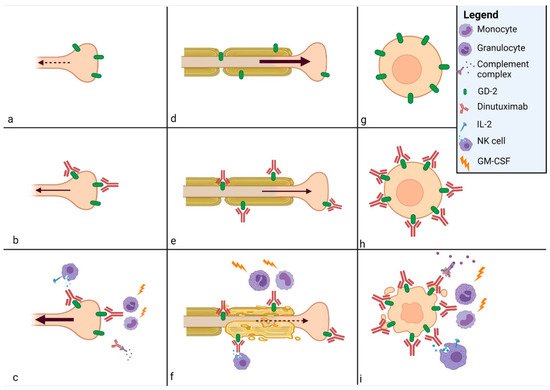
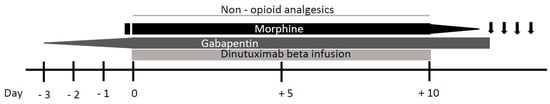
1. Dinutuximab Induced Neuropathic Pain
Prevention and Treatment
2. Dinutuximab Induced Peripheral Neuropathy
Treatment
This entry is adapted from the peer-reviewed paper 10.3390/ijms222312648
References
- Yu, A.L.; Gilman, A.L.; Ozkaynak, M.F.; London, W.B.; Kreissman, S.G.; Chen, H.X.; Smith, M.; Anderson, B.; Villablanca, J.G.; Matthay, K.K.; et al. Anti-GD2 Antibody with GM-CSF, Interleukin-2, and Isotretinoin for Neuroblastoma. N. Engl. J. Med. 2010, 363, 1324–1334.
- Anghelescu, D.L.; Bs, J.L.G.; Faughnan, L.; Wu, J.; Mao, S.; Furman, W.L.; Santana, V.M.; Navid, F. Comparison of pain outcomes between two anti-GD2 antibodies in patients with neuroblastoma. Pediatr. Blood Cancer 2015, 62, 224–228.
- Gilman, A.L.; Ozkaynak, M.F.; Matthay, K.K.; Krailo, M.; Yu, A.L.; Gan, J.; Sternberg, A.; Hank, J.A.; Seeger, R.; Reaman, G.H.; et al. Phase I Study of Ch14.18 with Granulocyte-Macrophage Colony-Stimulating Factor and Interleukin-2 in Children with Neuroblastoma after Autologous Bone Marrow Transplantation or Stem-Cell Rescue: A Report from the Children’s Oncology Group. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2009, 27, 85–91.
- Blom, T.; Lurvink, R.; Aleven, L.; Mensink, M.; Wolfs, T.; Dierselhuis, M.; van Eijkelenburg, N.; Kraal, K.; van Noesel, M.; van Grotel, M.; et al. Treatment-Related Toxicities During Anti-GD2 Immunotherapy in High-Risk Neuroblastoma Patients. Front. Oncol. 2021, 10, 601076.
- Ozkaynak, M.F.; Sondel, P.M.; Krailo, M.D.; Gan, J.; Javorsky, B.; Reisfeld, R.A.; Matthay, K.K.; Reaman, G.H.; Seeger, R.C. Phase I Study of Chimeric Human/Murine Anti-Ganglioside G(D2) Monoclonal Antibody (Ch14.18) with Granulocyte-Macrophage Colony-Stimulating Factor in Children with Neuroblastoma Immediately after Hematopoietic Stem-Cell Transplantation: A Children’s Cancer Group Study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2000, 18, 4077–4085.
- Simon, T.; Hero, B.; Faldum, A.; Handgretinger, R.; Schrappe, M.; Niethammer, D.; Berthold, F. Consolidation Treatment with Chimeric Anti-GD2-Antibody ch14.18 in Children Older Than 1 Year with Metastatic Neuroblastoma. J. Clin. Oncol. 2004, 22, 3549–3557.
- Sorkin, L.S.; Yu, A.L.; Junger, H.; Doom, C.M. Antibody Directed against GD(2) Produces Mechanical Allodynia, but Not Thermal Hyperalgesia When Administered Systemically or Intrathecally despite Its Dependence on Capsaicin Sensitive Afferents. Brain Res. 2002, 930, 67–74.
- Qarziba (Dinutuximab Beta)—Summary of Product Characteristics (SmPC)—(Emc). Available online: https://www.medicines.org.uk/emc/product/9441/smpc (accessed on 28 September 2021).
- Sorkin, L.S. Antibody Activation and Immune Reactions: Potential Linkage to Pain and Neuropathy. Pain Med. 2000, 1, 296–302.
- Terzic, T.; Cordeau, M.; Herblot, S.; Teira, P.; Cournoyer, S.; Beaunoyer, M.; Peuchmaur, M.; Duval, M.; Sartelet, H. Expression of Disialoganglioside (GD2) in Neuroblastic Tumors: A Prognostic Value for Patients Treated with Anti-GD2 Immunotherapy. Pediatr. Dev. Pathol. 2018, 21, 355–362.
- Schumacher-Kuckelkorn, R.; Volland, R.; Gradehandt, A.; Hero, B.; Simon, T.; Berthold, F. Lack of immunocytological GD2 expression on neuroblastoma cells in bone marrow at diagnosis, during treatment, and at recurrence. Pediatr. Blood Cancer 2016, 64, 46–56.
- Duman, B.B.; Sahin, B.; Ergin, M.; Güvenç, B. Loss of CD20 antigen expression after rituximab therapy of CD20 positive B cell lymphoma (diffuse large B cell extranodal marginal zone lymphoma combination): A case report and review of the literature. Med. Oncol. 2011, 29, 1223–1226.
- Sotillo, E.; Barrett, D.M.; Black, K.L.; Bagashev, A.; Oldridge, D.A.; Wu, G.; Sussman, R.T.; LaNauze, C.; Ruella, M.; Gazzara, M.R.; et al. Convergence of Acquired Mutations and Alternative Splicing of CD19 Enables Resistance to CART-19 Immunotherapy. Cancer Discov. 2015, 5, 1282–1295.
- Mukohara, T. Mechanisms of resistance to anti-human epidermal growth factor receptor 2 agents in breast cancer. Cancer Sci. 2010, 102, 1–8.
- Mueller, I.; Ehlert, K.; Endres, S.; Pill, L.; Siebert, N.; Kietz, S.; Brock, P.; Garaventa, A.; Valteau-Couanet, D.; Janzek, E.; et al. Tolerability, response and outcome of high-risk neuroblastoma patients treated with long-term infusion of anti-GD2 antibody ch14.18/CHO. mAbs 2018, 10, 55–61.
- Sorkin, L.S.; Otto, M.; Baldwin, W.M.; Vail, E.; Gillies, S.D.; Handgretinger, R.; Barfield, R.C.; Yu, H.M.; Yu, A.L. Anti-GD2 with an FC point mutation reduces complement fixation and decreases antibody-induced allodynia. Pain 2010, 149, 135–142.
- Ahmed, M.; Cheung, N.-K.V. Engineering anti-GD2 monoclonal antibodies for cancer immunotherapy. FEBS Lett. 2014, 588, 288–297.
- Navid, F.; Sondel, P.M.; Barfield, R.; Shulkin, B.L.; Kaufman, R.A.; Allay, J.A.; Gan, J.; Hutson, P.; Seo, S.; Kim, K.; et al. Phase I Trial of a Novel Anti-GD2 Monoclonal Antibody, Hu14.18K322A, Designed to Decrease Toxicity in Children with Refractory or Recurrent Neuroblastoma. J. Clin. Oncol. 2014, 32, 1445–1452.
- Federico, S.M.; McCarville, M.B.; Shulkin, B.L.; Sondel, P.M.; Hank, J.A.; Hutson, P.; Meagher, M.; Shafer, A.; Ng, C.Y.; Leung, W.; et al. A Pilot Trial of Hu-manized Anti-GD2 Monoclonal Antibody (Hu14.18K322A) with Chemotherapy and Natural Killer Cells in Children with Re-current/Refractory Neuroblastoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2017, 23, 6441–6449.
- Ozkaynak, M.F.; Gilman, A.L.; London, W.B.; Naranjo, A.; Diccianni, M.B.; Tenney, S.C.; Smith, M.; Messer, K.S.; Seeger, R.; Reynolds, C.P.; et al. A Comprehensive Safety Trial of Chimeric Antibody 14.18 With GM-CSF, IL-2, and Isotretinoin in High-Risk Neuroblastoma Patients Following Myeloablative Therapy: Children’s Oncology Group Study ANBL0931. Front. Immunol. 2018, 9, 1355.
- Mastrangelo, S.; Capozza, M.A.; Triarico, S.; Attinà, G.; Maurizi, P.; Romano, A.; Ruggiero, A. Opioid transdermal delivery system: A useful method for pain management in children. Ann. Transl. Med. 2021, 9, 185.
- Attinà, G.; Romano, A.; Triarico, S.; Mastrangelo, S.; Maurizi, P.; Ruggiero, A. Transdermal buprenorphine for pain management in children. Drugs Context 2021, 10, 1–8.
- Görges, M.; West, N.; Deyell, R.; Winton, P.; Cheung, W.; Lauder, G. Dexmedetomidine and Hydromorphone: A Novel Pain Management Strategy for the Oncology Ward Setting during Anti-GD2 Immunotherapy for High-Risk Neuroblastoma in Children. Pediatr. Blood Cancer 2015, 62, 29–34.
- Bertolizio, G.; Otis, A.; Tam, K.; Aswar, S.; Garbin, M.; Ingelmo, P. Multimodal Analgesic Plan for Children Undergoing Chimeric 14.18 Immunotherapy. J. Pediatr. Hematol. Oncol. 2021, 43, e169–e172.
- Sheehy, K.A.; Muller, E.A.; Lippold, C.; Nouraie, M.; Finkel, J.C.; Quezado, Z.M.N. Subanesthetic ketamine infusions for the treatment of children and adolescents with chronic pain: A longitudinal study. BMC Pediatr. 2015, 15, 198.
- Garrovillo, K.; Garrett, J.; Bollin, K.; Nasraty, F.; Sikand, H. Dinutuximab in adult-onset chemotherapy refractory high-risk neuroblastoma. J. Oncol. Pharm. Pract. 2020, 26, 2058–2065.
- Davies, A.J.; Kim, H.W.; Gonzalez-Cano, R.; Choi, J.; Back, S.K.; Roh, S.E.; Johnson, E.; Gabriac, M.; Kim, M.-S.; Lee, J.; et al. Natural Killer Cells Degenerate Intact Sensory Afferents following Nerve Injury. Cell 2019, 176, 716–728.
- Park, S.B.; Lin, C.S.-Y.; Krishnan, A.; Goldstein, D.; Friedlander, M.L.; Kiernan, M.C. Oxaliplatin-induced neurotoxicity: Changes in axonal excitability precede development of neuropathy. Brain 2009, 132, 2712–2723.
- Triarico, S.; Romano, A.; Attinà, G.; Capozza, M.A.; Maurizi, P.; Mastrangelo, S.; Ruggiero, A. Vincristine-Induced Peripheral Neuropathy (VIPN) in Pediatric Tumors: Mechanisms, Risk Factors, Strategies of Prevention and Treatment. Int. J. Mol. Sci. 2021, 22, 4112.
- Fukuda, Y.; Li, Y.; Segal, R.A. A Mechanistic Understanding of Axon Degeneration in Chemotherapy-Induced Peripheral Neuropathy. Front. Neurosci. 2017, 11, 481.
- Zingoni, A.; Fionda, C.; Borrelli, C.; Cippitelli, M.; Santoni, A.; Soriani, A. Natural Killer Cell Response to Chemotherapy-Stressed Cancer Cells: Role in Tumor Immunosurveillance. Front. Immunol. 2017, 8, 1194.
- Fine, J.H.; Chen, P.; Mesci, A.; Allan, D.S.; Gasser, S.; Raulet, D.; Carlyle, J.R. Chemotherapy-Induced Genotoxic Stress Promotes Sensitivity to Natural Killer Cell Cytotoxicity by Enabling Missing-Self Recognition. Cancer Res. 2010, 70, 7102–7113.
- Xiao, W.-H.; Yu, A.L.; Sorkin, L.S. Electrophysiological characteristics of primary afferent fibers after systemic administration of anti-GD2 ganglioside antibody. Pain 1997, 69, 145–151.
- Ladenstein, R.; Pötschger, U.; Valteau-Couanet, D.; Luksch, R.; Castel, V.; Yaniv, I.; Laureys, G.; Brock, P.; Michon, J.M.; Owens, C.; et al. Interleukin 2 with Anti-GD2 Antibody Ch14.18/CHO (Dinutuximab Beta) in Patients with High-Risk Neuroblastoma (HR-NBL1/SIOPEN): A Multicentre, Randomised, Phase 3 Trial. Lancet Oncol. 2018, 19, 1617–1629.
- Mody, R.; Naranjo, A.; Van Ryn, C.; Yu, A.; London, W.B.; Shulkin, B.; Parisi, M.T.; Servaes, S.-E.-N.; Diccianni, M.B.; Sondel, P.M.; et al. Irinotecan–temozolomide with temsirolimus or dinutuximab in children with refractory or relapsed neuroblastoma (COG ANBL1221): An open-label, randomised, phase 2 trial. Lancet Oncol. 2017, 18, 946–957.
- Slart, R.; Yu, A.L.; Yaksh, T.L.; Sorkin, L.S. An Animal Model of Pain Produced by Systemic Administration of an Immuno-therapeutic Anti-Ganglioside Antibody. Pain 1997, 69, 119–125.
- Saleh, M.N.; Khazaeli, M.B.; Wheeler, R.H.; Dropcho, E.; Liu, T.; Urist, M.; Miller, D.M.; Lawson, S.; Dixon, P.; Russell, C.H. Phase I trial of the murine monoclonal anti-GD2 antibody 14G2a in metastatic melanoma. Cancer Res. 1992, 52, 4342–4347.
- Davies, A.J.; Rinaldi, S.; Costigan, M.; Oh, S.B. Cytotoxic Immunity in Peripheral Nerve Injury and Pain. Front. Neurosci. 2020, 14, 142.
- Yuki, N.; Yamada, M.; Tagawa, Y.; Takahashi, H.; Handa, S. Pathogenesis of the neurotoxicity caused by anti-GD2 antibody therapy. J. Neurol. Sci. 1997, 149, 127–130.
- Ohmi, Y.; Ohkawa, Y.; Yamauchi, Y.; Tajima, O.; Furukawa, K.; Furukawa, K. Essential Roles of Gangliosides in the Formation and Maintenance of Membrane Microdomains in Brain Tissues. Neurochem. Res. 2012, 37, 1185–1191.
- De Bernardi, B.; Quaglietta, L.; Haupt, R.; Castellano, A.; Tirtei, E.; Luksch, R.; Mastrangelo, S.; Viscardi, E.; Indolfi, P.; Cellini, M.; et al. Neuroblastoma with symptomatic epidural compression in the infant: The AIEOP experience. Pediatr. Blood Cancer 2014, 61, 1369–1375.
