Osteoarthritis (OA) is a common health problem leading to pain, limitation in physical function, a decrease in the quality of life and disability. OA affects 60–70% of the population above 65 years of age all over the world, and is associated with a high cost of healthcare. The main method of treatment of OA, apart from pharmacotherapy and surgery, is comprehensive rehabilitation. Advances in medical technology have resulted in the possibility of using computer-assisted interventions in rehabilitation. There are no conclusive reports that interventions based on VR are more effective than standard physical therapy. Moreover, evidence regarding patients after total hip arthroplasty (THA) is very scarce. The effectiveness of VR-based rehabilitation is unclear, although interventions based on VR are promising in view of pain management, postural and proprioception training.
- rehabilitation
- knee osteoarthritis
- hip osteoarthritis
- knee arthroplasty
- hip arthroplasty
- virtual reality
- review
1. Definition
Degenerative joint disease or osteoarthrosis (OA) is a progressive joint disease characterized by the focal loss of cartilage, little evidence of the typical form of inflammation, and by the hypertrophy of adjacent bone and soft tissue.
2. Introduction
Such a definition is synonymous with the hypertrophic form of chronic (osteo)arthritis [1][2].
OA is a well known world-wide cause of a progressive disability [3]. OA is increasing in prevalence across the world mainly due to the aging population [4]. OA affects approximately 70% of women and 60% of men older than 65 years [4]. However, the estimated prevalence and incidence of OA may vary depending on the definition of the disease, the joints considered and the population being studied [3].
As a degenerative disease, OA increases with age, exacerbating the associated social and medical problems, leading in the long run to an extensive need of holistic treatment. The risk of OA increases considerably every decade after the age of about 45 years [5].
Osteoarthritis progressively degrades the patient’s independence, mobility and participation in social life, thus reducing the overall quality of life [5]. Dominant clinical problems related to OA include pain, limited joint mobility, decreased muscular strength, impaired proprioception and increased incidence of falls. OA also affects mental health, resulting primarily in depressive episodes [5][6].
Non-pharmacological methods of treatment of degenerative joint disease are aimed at pain control, improvement of function and the quality of life of the patient, with the goal of minimizing the adverse effects of the therapy [7][8][9].
Over the course of the recent decades, arthroplasty or joint replacement surgery became the principal method of orthopaedic surgical treatment of advanced degenerative joint disease, primarily in the case of the hip joint and the knee joint. However, the currently available total hip arthroplasty (THA) and total knee arthroplasty (TKA) indication criteria are based on limited evidence [10].
Rehabilitation, especially work-related rehabilitation (physical therapy) is widely employed as an element of complex therapy or as a standalone intervention during the treatment of degenerative joint disease. Kinesiotherapy on a regular basis and habitual physical activity are substantial in the prevention of OA and in managing the initial stages of the disease. Preoperative rehabilitation treatment, as a preparation for joint surgery, shows benefits with regards to the length of hospital stay and discharge destination (home/rehabilitation ward) [11]. Postoperative rehabilitation treatment is desirable after surgery in view of decreased morbidity, increased satisfaction and safety after discharge from the surgical ward [12].
Rehabilitation is widely used following joint replacement operations, allowing the restoration of the function of the affected joint and preservation of obtained results. A progressive exercise program is beneficial considering recovery after THA/TKA, allowing for a faster recovery and an increase in the range of motion [13][14].
Recent advances in medical technology resulted in a gradual introduction of computer-assisted interventions into rehabilitation. In recent decades, new technologies in rehabilitation were developed from the simplest forms of biofeedback implementations into hardware platforms and motion capture systems augmented by biofeedback, augmented reality (AR) systems and virtual reality (VR) systems. The range of employed technologies varies from non-expensive, popular gaming platforms to highly specialized systems with dedicated hardware and software platforms. Nowadays, the threat of the SARS-CoV-2 pandemic, where physical interactions could be prohibited, may result in an increased interest in contactless methods of rehabilitation, a condition fulfilled by telerehabilitation [15].
3. Results
3.1. Searching Results
A total of 394 articles was found, and after the removal of duplicates, 289 titles and abstracts were screened. From the screened abstracts, 29 studies were read in full text. Nineteen of those were excluded for the following reasons: conference papers, low quality randomized controlled trial (RCT) with insufficient data, intervention not relevant or wrong population (concerning also other types of OA, ankle arthroplasty, spondylarthritis or a not well defined population). The final ten randomized controlled trials were included for qualitative analysis. Figure 1 presents the PRISMA flowchart of the study selection.
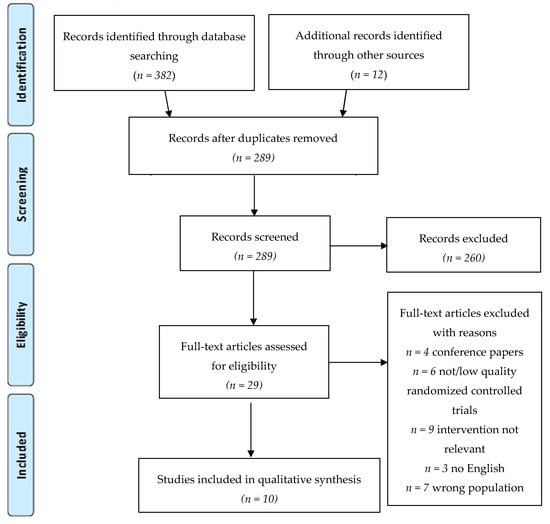
Figure 1. Flowchart of the article selection process (2009 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram).
3.2. Demographic Data
In the total 10 RCTs, there were 492 subjects with a mean age of 60.6 years. Nine of the trials included information regarding sex, and thus the percentage of male participants was 41.6%. The studies focused on the rehabilitation of the following orthopaedic conditions: seven total knee arthroplasty (TKA), two knee osteoarthritis (KOA), one total hip arthroplasty (THA). The authors decided to include one study [22] that compares two groups after knee surgery in view of the VR rehabilitation: patients after TKA and after anterior cruciate ligament (ACL) tear repair. It was considered desirable to include this study because of the valuable reports on the effectiveness of the VR training. In addition, in the study group, only two patients underwent ACL repair, and the remaining 15 subjects underwent TKA. It was recognized that the initial purpose of the intervention aimed solely at increasing the range of knee movement was the same for both conditions. Moreover, the specifics of rehabilitation aimed at increasing the range of knee movement are similar and should not affect the results of this study.
A detailed description of the studies included in the review is presented in Table 1.
Table 1. Characteristics of the included studies.
| No | First Author, Year, Country | PEDro Scale | Main Objective | Participants | Intervention/Technology | Outcomes | Research Tools | Main Results |
|---|---|---|---|---|---|---|---|---|
| 1 | Gianola et al. [23] 2020, Italy | 7/10 | The effectiveness of VR rehabilitation vs. standard rehabilitation for physical function after primary TKA | Adults 45–80 years old 3–4 days after primary unilateral TKA: all n = 74 study n = 35 controls n = 39 |
Sixty minute daily training for at least 5 days All participants performed passive ROM exercises on Kinetec knee continuous passive motion system and functional exercises. Study—VR games focused on balance, proprioception and function of lower limbs Controls—standard postoperative physiotherapy |
Pain; knee disability quality of life; patients’ assessment of their condition; functional performance; leg muscle strength; knee ROM; proprioception; balance; medication assumption |
VAS WOMAC EQ-5D GPE FIM dynamometer goniometer stabilometric platform VRRS |
No significant difference in pain reduction and other outcomes, except improved proprioception in the study VR group. |
| 2 | Lin et al. [24] 2020, Taiwan | 8/10 | A comparison of VR games exercises and standard physical exercises in patients with knee OA | Patients aged 40–85 with knee OA (Kellgren and Lawrence Score ≥ 2): all n = 80 study n = 40 controls n = 40 |
Three times a week for 4 weeks with a follow-up All received 20 min of hot packs and 20 min of TENS Study—active video games using the Hot Plus system focused on muscle strength, coordination and ROM of limbs Controls—standard exercises |
knee disability; quality of life; psychosocial distress; fatigue; pain; work ability; balance |
WOMAC WHOQOL-BREF HADS MFI CPG WAI Biodex Stability System |
No significant difference between VR training and standard exercises in improving knee disability, but games improved dynamic balance, physical functional performance, and physical health more than therapeutic exercises. |
| 3 | Jin et al. [25] 2018, China | 5/10 | The effects and benefits of VR training in postoperative patients after TKA | Patients after primary unilateral TKA: all n = 66 study n = 33 controls n = 33 |
Standard therapeutic exercises + 30 min three times a day: Study—VR training (Mide Technology) from the second day of therapy, focus on knee flexion (rowing boat) Controls—3 sets of active knee flexion exercises |
knee disability; evaluation of early results of TKA; pain; ROM |
WOMAC HSS VAS goniometer |
VR training effects better at improving knee functional recovery, ROM and relieving pain after TKA than standard exercises. |
| 4 | Koo et al. [26] 2018, South Korea | 6/10 | The effectiveness of enhanced reality on analgesia and physical function after TKA | Patients with unilateral TKA: all n = 42 study n = 22 controls n = 20 |
Enhanced reality analgesia visual biofeedback (combination of the VR, real-time motion capture, mirror therapy using real-time image processing technique) Study—intervention was provided shortly after physiotherapy for five times a week for 2 weeks Controls—intervention was provided for five times a week for 1 week |
Pain; ROM; knee disability; endurance and aerobic capacity; lower extremities; strength; medication assumption; |
VAS goniometer WOMAC 6MWT TST |
Analgesia and improvement in ROM in both groups were achieved, but in the study group that lasted longer than in controls. |
| 5 | Ficklscherer et al. [22] 2016, Germany | 4/10 | The assessment of the Nintendo Wii as an appropriate and safe tool in rehabilitation after orthopedic knee surgery | Patients with TKA or anterior cruciate ligament (ACL) tear: all n = 30 study n = 17 controls = 13 |
Four weeks of intervention Study—exergames on The Nintendo Wii and standard physical therapy Controls—standard physical therapy |
Knee function and disability | IKDC MCKRS TLKS |
No significant difference between VR training and standard exercises in improving knee disability, but slightly greater improvement in the Wii group. Intervention without a negative influence on patients. |
| 6 | Elshazly et al. [27] 2016, Saudi Arabia | 7/10 | A comparison of the effectiveness of VR training over sensory motor training in the treatment of osteoarthritis |
Patients with chronic OA (> 3 mths) WOMAC: 71 points: all n = 60 virtual reality training n = 20 Qsensory motor training n = 20 controls n = 20 |
Three times per week for 8 weeks Study—virtual reality training Light Race VR interactive game 15-30′ ControlsI—sensory motor progressive training II—conventional exercise training warm-up, walking, cool-down |
Pain intensity; joint proprioception; knee disability; quality of life |
VAS perception sense WOMAC HRQOL |
Significant improvement in the outcome measures in all the training methods. VR training showed a substantial improvement over the other methods. |
| 7 | Christiansen et al. [28] 2015, USA | 7/10 | The effectiveness of weight-bearing (WB) biofeedback training on WB symmetry and functional joint moments following unilateral total knee arthroplasty |
Patients with unilateral TKA: all n = 26 study n = 13 controls n = 13 |
Study—weight-bearing biofeedback on the Nintendo Wii Fit Plus and Wii Balance Board and physical therapy daily for 6 weeks Controls—physical therapy twice per day for 6 weeks |
Gait/walking speed; lower limb; weight-bearing ratios (WBRs); lower limb joint movement |
12 m walkway—gait speed FTSST |
No significant difference between VR training and controls in WBR. FTSST time improved in the study group compared to the control group. The tendency for improved walking speed in the study group at 26 weeks (P = 0.068). |
| 8 | Ayoade et al. [29] 2014, Canada | 4/10 | The presentation of rehabilitation visualization system (RVS); the assessment of usability and feasibility of the RVS at home |
Patients with TKA in the early phase of post-operative rehabilitation: all n = 21 study n = 11 controls n = 10 |
Ten days of training in the hospital and then at home for up to 6 weeks Study—rehabilitation visualization system and exercise handbook Controls—exercise handbook only |
Knee ROM; functional performance; health surveys; rehabilitation experience; usability |
Goniometer OKS SF-12 survey IMI SUS |
Overall, no significant difference between RVS training and controls. However, RVS made home rehabilitation more engaging and improved the communication between patients and the therapist. |
| 9 | Fung et al. [30] 2012, Canada | 5/10 | The examination of the Nintendo Wii Fit as an acceptable adjunct to physiotherapy concerning balance, ROM, muscle strength and function in outpatients following TKA | Outpatients after TKA: all n = 50 study n = 27 controls n = 23 |
Twice a week for 75 min Study—15 min of exergames focused on postural control and balance in The Nintendo Wii Fit and 60 min of physical therapy Controls—60 min of physical therapy and 15 min of lower extremity strengthening and balance training |
Balance; knee ROM; postural control; lower leg function; pain |
2MWT Goniometer ABCS LFES NPRS satisfaction survey |
No significant difference between study and controls. Wii Fit is potentially acceptable as an adjunct to physical therapy intervention in view of balance, postural control and use of the lower extremities. |
| 10 | Lehrl et al. [31] 2012, Germany | 5/10 | The enhancing of rehabilitation using mental activation | Patients after THA: all n = 32 study n = 16 controls n = 16 |
Study—30 min per day for 12 days of video game Dr. Kawashima’s Brain Training: How Old Is Your Brain? Controls—without intervention |
Hip function and disability | HHS PMA |
Significant improvement in hip function obtained in the study group in HHS, but not in PMA. |
Abbreviations: VR—virtual reality, TKA—total knee arthroplasty, THA—total hip arthroplasty, ROM—range of motion, VAS—Visual Analogue Scale, WOMAC—Western Ontario and McMaster Universities osteoarthritis index, EQ-5D EuroQol five-dimensional questionnaire, GPE—the global perceived effect score, FIM—functional independence measure questionnaire, VRRS—Virtual Reality Rehabilitation System, OA – osteoarthritis, TENS—Transcutaneous Electrical Nerve Stimulation, WHOQOL-BREF—World Health Organization Quality of Life-Brief Vision, HADS—Hospital Anxiety and Depression Scale, MFI—Multidimensional Fatigue Inventory, CPGQ—Chronic Pain Grade Questionnaire, WAI—Work Ability Index, HSS—Hospital for Special Surgery knee score, 6MWT—6 min walk test, TST—timed-stands test, IKDC—International Knee Documentation Committee score, mCKRS—Modified Cincinnati Knee Rating System, TLKS—Tegner Lysholm Knee Score, HRQOL—health-related quality of life, FTSST—Five Times Sit-to-Stand Test, OKS—Oxford knee score, SF-12 survey—short form survey from the SF-36 Health Survey, IMI—Intrinsic Motivation Inventory, SUS—system usability scale, 2MWT—2 min walk test, ABCS—Activity-Specific Balance Confidence Scale, LFES—Lower Extremity Functional Scale, NPRS—Numeric Pain Rating Scale, HHS—Harris Hip Score, PMA—Merle d’Aubigné score.
3.3. Methodological Evaluation
The methodological quality of the analysed research rated on the PEDro scale ranged from moderate quality—4 points [22][29]—to high quality—8 points [24]—with a mean score of 5.9 points (moderate quality). Four studies were high quality above 7 points on the PEDro scale [22][23][27][28].
The most common type of bias was due to the lack of participants and therapists blinding (in all studies). In most physiotherapy research, blinding is difficult due to the specifics of carrying out interventions. However, blinding all test assessors is possible and should be used in RCT, which concerned about half of the included studies [23][24][26][28][30]. The highest quality in evidence-based medicine and evidence-based practice is obtained by randomized double-blind or triple-blind control trials. Blinding prevents bias caused by the expectations of the patients or therapists (performance bias) and in the assessment by assessors (detection bias) [32].[32][33][34][35][36][37][38] However, double or triple blinding in rehabilitation studies is often difficult or impossible because the patient and the therapist are aware of the intervention [33]. However, a single blinding in physical therapy is possible if the investigator does not have information about the intervention and the randomization of patients [34]. Some studies indicate that the absence of blinding affects the overestimation of the results [35] and the level of blinding of rehabilitation studies is poor [36].
Another limitation was the lack of the intention-to-treat analysis which concerned eight out of 10 included RCTs (it occurred only in [24][27]). The intention to treat is necessary to maintain a prognostic balance in the results between groups. Results of participants who did not complete the intervention but were initially assigned by randomization should be included in the analysis to maintain the similarity of the compared groups, which minimizes the risk of bias [37]. Missing data can be considered as treatment failure [38].
The main limitations of the included trials were the small sample size [22][24][26][28][29][30][31]and the lack of long-term follow up [22][24][27][28][29].
3.4. Type of Technology
3.4.1. Exergames
Physical exercises in the form of exergames and virtual reality are increasingly used in rehabilitation. Among the included studies, eight described games and virtual reality training in patients after TKA and THA. Gianola et al. [23] used the Virtual Reality Rehabilitation System (VRRS, Khymeia, Italy) in rehabilitation after TKA. The VRRS is a device that allows the correct performance of exercises based on visual and auditory biofeedback and a system of interactive games focused on body balance.
Lin et al. [24] applied exercises based on interactive games using the Hot Plus system (Supreme Investment Co., Taipei, Taiwan). The patients with knee OA participated in the game by moving the legs and tilting the torso in each direction, transferring the weight of the body to the sensory pillows that they were standing on. Exercises were regulated at three levels of difficulty and visual and auditory biofeedback informed about their correct performance. The purpose of VR exercises was to increase the range of motion and muscular strength of lower extremities and to improve body balance and coordination. A similar type of game, aimed at increasing muscle strength, body balance and the leg range of motion was applied by Elshazly et al. [27]. The patients with knee OA played the Light Race game, consisting of balancing the body weight from one leg to the other in the right direction, to move on a virtual platform displayed on the TV screen.
Jin et al. [25] used virtual reality (Mide Technology Inc., Cangzhou, China) on the second day after surgery as a supplement to early rehabilitation in patients after TKA. The patients put on a virtual reality headset and had motion sensors connected to the operated limb. They performed exercises that consisted of playing a game simulating boat rowing, using active flexion and extension of the operated knee.
On the other hand, Lehrl et al. [31] used an interactive cognitive game, Kawashima’s Brain Training: How Old Is Your Brain? (Nintendo; Kyoto, Japan), for patients after THA. The goal was to improve the executive functions—memory length and information processing speed. The stimulation of cognitive functions had a positive effect on the physical state, as patients were more willing to perform the exercises.
Christiansen et al. [28] used The Nintendo Wii Fit Plus game associated with Wii Balance Board (Nintendo of America, Inc., Redmond, WA, USA) to aid the recovery of the operated lower limb weight-bearing symmetry in the home rehabilitation system. The patients played interactive games with the progression of the operated limb load and the level of difficulty ranging from static to dynamic exercises. They received visual and auditory biofeedback after correctly completing the task. Ficklscherer et al. [22] also applied the Nintendo Wii in the rehabilitation of patients after knee surgeries—TKA (n = 26) and ACL plastic surgery (n = 4). The aim of this study was to assess the usability and safety of this device, considering the age of the participants and their experience with modern technology. Fung et al. [30] also evaluated the effectiveness of the therapy on the function of the operated limb, body balance, mobility and muscle strength in people after TKA using the Nintendo Wii.
3.4.2. Feedback
Koo et al. [26] studied the effectiveness of analgesic therapy using augmented reality, which was a combination of mirror therapy and virtual reality (enhanced reality using real-time image processing technique). The patients after TKA performed exercises based on visual biofeedback, in which the image of the operated leg’s movement was replaced by a visualization of the movement of the healthy leg. Another kind of visual feedback was applied by Ayoade et al. [29] as home physical therapy for patients after TKA. It consisted of a knee joint exercise system based on the use of motion sensors and real-time visual biofeedback (Rehabilitation Visualization System, RVS). The exercises were focused on strengthening the muscles and increasing the range of motion.
3.5. Effects of Intervention—Primary Outcomes
3.5.1. Physical Function
The evaluation of the condition of the knee after TKA and with OA were conducted in eight out of 10 studies. Among the most commonly used scales [24][25][26][27] was the WOMAC scale (The Western Ontario and McMaster Universities Osteoarthritis Index), which includes the assessment of pain, stiffness, and physical functioning [39]. Two studies [23][25] showed a statistically greater improvement of knee condition in the VR training group than in the controls for patients after TKA. However, in one trial [23], improvement was obtained only in reducing joint stiffness. On the other hand, the authors [22][23][26][29][30] presented no major functional improvement in VR rehabilitation for TKA patients. For patients with knee OA, VR rehabilitation had good results for physical function [27] and for initial improvement in pain reduction [24].
In contrast, one of the included studies concerning THA [31] showed that the gaming group had a much better improvement in hip function than the control group in the Harris Hip Score (HHS). Despite the observed improvement in function and mobility, there was no statistically significant improvement in the second scale of hip function—Merle d’Aubigné score (PMA). However, the contrast in the statistical significance of the results of hip functional assessment in these two scales may be due to the variance in their scores, as the more detailed HHS has 0–100 point scale, and PMA, which is less detailed, has 0–18 point scale.
3.5.2. Balance
Three included studies evaluated the impact of VR training on body balance. For this purpose, stabilometric platforms [23][24] or the Activity-Specific Balance Confidence Scale (ABCS) [30] were used. Two studies [23][30] showed no statistically significant improvement in the exergames training group for the patients after TKA. Additionally, Christiansen et al. In [28], the load on the operated limb after TKA was evaluated, using the peak vertical ground reaction force (vGRF) on a stabilometric platform during the Five Times Sit-to-Stand Test (FTSST). No better results were obtained in the study group. However, the speed of FTSST test performance was statistically better in the study group than in the control group.
On the other hand, one study [24] indicated a greater increase in dynamic stability in the group of knee OA patients that performed VR training.
3.5.3. Gait
Four studies assessed the gait, using marching tests of varying duration: 2 min [30], 6 min [26], 10 min [24] and 12 min [28]. In addition, one study [28] assessed the gait pattern, including the mobility of the joints of the operated extremity. Only in one study [24] was an increase in the gait efficiency achieved in the group of VR training for the patients with knee OA. Three other studies [26]28][30] consisting of patients after TKA showed no improvement in gait performance.
3.5.4. Range of Motion
Assessment of the range of motion of the operated joint after TKA using goniometer was performed in five studies [23][25][26][29][30]. In three trials [25][26][29], a statistically significant increase in the movements of the operated knee was obtained in the exergame groups. Furthermore, the patients increased the knee range of motion faster, as assessed by the time needed to reach 60 and 90 degrees of flexion [25]. In the control group, there were cases of deterioration of the motion during therapy, which was not noted in the experimental group [29]. In two studies [23][30], no statistically significant differences in the range of motion were noticed.
3.5.5. Proprioception
Knee joint proprioception was evaluated for patients with knee OA [27] and after TKA [23] and in both studies, significant improvement was obtained in the group using VR training compared to the control group.
3.5.6. Muscular Strength
The muscular strength of the operated leg was examined by a dynamometer [23] or by using the timed-stands test (TST) [26]. In both trials, there were no statistically significant differences in the improvement of muscle strength between the study groups and controls for the patients after TKA.
3.5.7. Pain
The level of pain was assessed by five researchers using the following scales: Visual Analog Scale [23][25][26][27] and Numeric Pain Rating Scale [30]. In two trials [25][26] statistically significant greater pain reduction was demonstrated in the VR training group, as well as the analgesic effect related to the length of training [26] was longer for the patients after TKA. However, the other two studies [23][30] did not show such a difference for these patients, which in one of them [23] may be due to the initial disproportion in the results of the assessment of the level of pain between the test and control group. Only one study [27] assessed the level of pain in patients with knee OA and suggests improvement in favour of VR rehabilitation.
3.6. Effect of Intervention—Secondary Outcomes
3.6.1. Quality of Life
The impact of VR training on increasing the quality of life was tested by various scales: EuroQoL five-dimensional (EQ-5D) [23], World Health Organization Quality of Life-Brief Vision (WHOQOL-BREF [24], short form survey from the SF-36 Health Survey (SF-12) [29] and health-related quality of life (HRQOL) [27]. Lin et al. [24] emphasized a significant improvement in the physical health domain of WHOQOL-BREF in the VR-training group compared to the control group for patients with knee OA. The beneficial effect of VR training on the quality of life for knee OA is proved also by Elshazly’s research [27]. In contrast, the other two studies [23][29] concerning patients after TKA did not show the impact of VR training on increasing the quality of life of patients.
3.6.2. Adherence and Motivation
Four trials [22][24][29][30] focused on the acceptance and adaptation of patients for VR-based rehabilitation. Lin et al. [24] emphasized that the 4 week VR rehabilitation program had a 100% degree of adherence, and in the control group where standard exercises were performed, the rate was 93%. Ficklscherer et al. [22] payed attention to the lack of side effects, safety and acceptance of exergames as a form of physiotherapy. Fung et al. [30] stated that gaming rehabilitation is a satisfactory and acceptable form of treatment. However, Ayoade et al. [29] assessed the level of adherence and the involvement of patients in the rehabilitation process by assessing the number of days in which they participated in the planned exercises. The level of involvement in both groups was the same. In addition, the patients’ experiences regarding the type of home rehabilitation were assessed using the Intrinsic Motivation Inventory (IMI) questionnaire and there was no difference between the degree of interest and motivation between the VR rehabilitation and standard exercises.
3.6.3. Inpatient/Outpatient/Home Physical Therapy
Seven trials [22][23][24][26][27][30] performed the intervention in a hospital or clinic assisted by a therapist/researcher, while two trials [28][29] carried out the intervention as a home rehabilitation program for patients after TKA. Christiansen et al. [28] offered the patients a therapist’s control 1–3 times a week and provided them with instructions on how to perform the exercises. Ayoade et al. [29] also assessed the effectiveness of exercises at home using a visual communication system with the therapist (video conferences). In addition, Ayoade et al. [29] assessed the usability of VR rehabilitation using the System Usability Scale (SUS) questionnaire and obtained results suggesting that home VR rehabilitation was associated with greater patient involvement, was motivating because it yielded information about the progress of exercises and improved communication between the therapist and the patient.
This entry is adapted from the peer-reviewed paper 10.3390/jcm9082639
References
- Attur, M.G.; Dave, M.; Akamatsu, M.; Katoh, M.; Amin, A.R. Osteoarthritis or osteoarthrosis: The definition of inflammation becomes a semantic issue in the genomic era of molecular medicine. Osteoarthr. Cartil. 2002, 10, 1–4. [Google Scholar] [CrossRef]
- Berenbaum, F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis!). Osteoarthr. Cartil. 2013, 21, 16–21. [Google Scholar] [CrossRef]
- Vina, E.R.; Kent Kwoh, C. Epidemiology of Osteoarthritis: Literature Update Ernest. Physiol. Behav. 2018, 30, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Sarzi-Puttini, P.; Cimmino, M.A.; Scarpa, R.; Caporali, R.; Parazzini, F.; Zaninelli, A.; Atzeni, F.; Canesi, B. Osteoarthritis: An overview of the disease and its treatment strategies. Semin. Arthritis Rheum. 2005, 35, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Moskowitz, R.W. The burden of osteoarthritis: Clinical and quality-of-life issues. Am. J. Manag. Care 2009, 15, 223–229. [Google Scholar]
- World Health Organization. World Report on Ageing and Health 2015; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Jordan, K.M.; Arden, N.K.; Doherty, M.; Bannwarth, B.; Bijlsma, J.W.J.; Dieppe, P.; Gunther, K.; Hauselmann, H.; Herrero-Beaumont, G.; Kaklamanis, P.; et al. EULAR Recommendations 2003: An evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann. Rheum. Dis. 2003, 62, 1145–1155. [Google Scholar] [CrossRef]
- Zhang, W.; Doherty, M.; Arden, N.; Bannwarth, B.; Bijlsma, J.; Gunther, K.P.; Hauselmann, H.J.; Herrero-Beaumont, G.; Jordan, K.; Kaklamanis, P.; et al. EULAR evidence based recommendations for the management of hip osteoarthritis: Report of a task force of the EULAR Standing Committee for International Clinical Studies Including Therapeutics (ESCISIT). Ann. Rheum. Dis. 2005, 64, 669–681. [Google Scholar] [CrossRef]
- Hochberg, M.C.; Altman, R.D.; April, K.T.; Benkhalti, M.; Guyatt, G.; McGowan, J.; Towheed, T.; Welch, V.; Wells, G.; Tugwell, P. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012, 64, 465–474. [Google Scholar] [CrossRef]
- Gademan, M.G.J.; Hofstede, S.N.; Vliet Vlieland, T.P.M.; Nelissen, R.G.H.H.; Marang-Van de Mheen, P.J. Indication criteria for total hip or knee arthroplasty in osteoarthritis: A state-of-the-science overview. BMC Musculoskelet. Disord. 2016, 17, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Coudeyre, E.; Jardin, C.; Givron, P.; Ribinik, P.; Revel, M.; Rannou, F. Could preoperative rehabilitation modify postoperative outcomes after total hip and knee arthroplasty? Elaboration of French clinical practice guidelines. Ann. Readapt. Med. Phys. 2007, 50, 189–197. [Google Scholar] [CrossRef] [PubMed]
- Kehlet, H.; Wilmore, D.W. Multimodal strategies to improve surgical outcome. Am. J. Surg. 2002, 183, 630–641. [Google Scholar] [CrossRef]
- Lenssen, A.F.; De Bie, R.A. Role of physiotherapy in peri-operative management in total knee and hip surgery. Injury 2006, 37, 41–43. [Google Scholar] [CrossRef]
- Pozzi, F.; Snyder-Mackler, L.; Zeni, J. Physical exercise after knee arthroplasty: A systematic review of controlled trials. Eur. J. Phys. Rehabil. Med. 2013, 49, 877–892. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.S.Y.; Teo, W.Z.W.; Teo, W.Z.Y.; Chai, Y.W. Virtual Reality as a Bridge in Palliative Care during COVID-19. J. Palliat. Med. 2020, 23, 756. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Riva, J.J.; Malik, K.M.P.; Burnie, S.J.; Endicott, A.R.; Busse, J.W. What is your research question? An introduction to the PICOT format for clinicians. J. Can. Chiropr. Assoc. 2012, 56, 167–171. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Olivo, S.A.; Macedo, L.G.; Gadotti, I.C.; Fuentes, J.; Stanton, T.; Magee, D.J. Scales to Assess the Quality of Randomized Controlled Trials: A Systematic Review. Phys. Ther. 2008, 88, 156–175. [Google Scholar] [CrossRef]
- Ficklscherer, A.; Stapf, J.; Meissner, K.M.; Niethammer, T.; Lahner, M.; Wagenhäuser, M.; Müller, P.E.; Pietschmann, M.F. Testing the feasibility and safety of the Nintendo Wii gaming console in orthopedic rehabilitation: A pilot randomized controlled study. Arch. Med. Sci. 2016, 6, 1273–1278. [Google Scholar] [CrossRef]
- Gianola, S.; Stucovitz, E.; Castellini, G.; Mascali, M.; Vanni, F.; Tramacere, I.; Banfi, G.; Tornese, D. Effects of early virtual reality-based rehabilitation in patients with total knee arthroplasty: A randomized controlled trial. Medicine (U.S.) 2020, 99. [Google Scholar] [CrossRef]
- Lin, Y.-T.; Lee, W.-C.; Hsieh, R.-L. Active video games for knee osteoarthritis improve mobility but not WOMAC score: A randomized controlled trial. Ann. Phys. Rehabil. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Feng, Y.; Ni, Y.; Shan, Z. Virtual reality intervention in postoperative rehabilitation after total knee arthroplasty: A prospective and randomized controlled clinical trial. Int. J. Clin. Exp. Med. 2018, 11, 6119–6124. [Google Scholar]
- Koo, K.I.; Park, D.K.; Youm, Y.S.; Do Cho, S.; Hwang, C.H. Enhanced Reality Showing Long-Lasting Analgesia after Total Knee Arthroplasty: Prospective, Randomized Clinical Trial. Sci. Rep. 2018, 8, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Elshazly, F.A.A.; Nambi, G.S.; Elnegamy, T.E. Comparative study on Virtual Reality Training (VRT) over Sensory Motor Training (SMT) in Unilateral Chronic Osteoarthritis—A Randomized Control Trial. Int. J. Med. Res. Health Sci. 2016, 5, 7–16. [Google Scholar]
- Christiansen, C.L.; Bade, M.J.; Davidson, B.S.; Dayton, M.R.; Stevens-Lapsley, J.E. Effects of weight-bearing biofeedback training on functional movement patterns following total knee arthroplasty: A randomized controlled trial. J. Orthop. Sports Phys. Ther. 2015, 45, 647–655. [Google Scholar] [CrossRef]
- Ayoade, M.; Baillie, L. A novel knee rehabilitation system for the home. In Proceedings of the 32nd Annual ACM Conference on Human Factors in Computing Systems—CHI’14, Toronto Ontario, Canada, April 2014; ACM Press: New York, NY, USA, 2014; pp. 2521–2530. [Google Scholar]
- Fung, V.; Ho, A.; Shaffer, J.; Chung, E.; Gomez, M. Use of Nintendo Wii FitTM In the rehabilitation of outpatients following total knee replacement: A preliminary randomised controlled trial. Physiotherapy (U.K.) 2012, 98, 183–188. [Google Scholar] [CrossRef]
- Lehrl, S.; Gusinde, J.; Schulz-Drost, S.; Rein, A.; Schlechtweg, P.M.; Jacob, H.; Krinner, S.; Gelse, K.; Pauser, J.; Brem, M.H. Advancement of physical process by mental activation: A prospective controlled study. J. Rehabil. Res. Dev. 2012, 49, 1221.
- Gluud, L.L. Bias in clinical intervention research. Am. J. Epidemiol. 2006, 163, 493–501. [Google Scholar] [CrossRef]
- Villamar, M.F.; Contreras, V.S.; Kuntz, R.E.; Fregni, F. The reporting of blinding in physical medicine and rehabilitation randomized controlled trials: A systematic review. J. Rehabil. Med. 2013, 45, 6–13. [Google Scholar] [CrossRef]
- Kucio, C.; Pilch, J. Metody zaślepiania badań klinicznych w fizjoterapii. Physiotherapy 2013, 62–64. [Google Scholar] [CrossRef]
- Nüesch, E.; Reichenbach, S.; Trelle, S.; Rutjes, A.W.S.; Liewald, K.; Sterchi, R.; Altman, D.G.; Jüni, P. The importance of allocation concealment and patient blinding in osteoarthritis trials: A meta-epidemiologic study. Arthritis Care Res. 2009, 61, 1633–1641. [Google Scholar] [CrossRef] [PubMed]
- Saltaji, H.; Armijo-olivo, S.; Cummings, G.G.; Amin, M.; Costa, B.R.; Flores-mir, C. Influence of blinding on treatment effect size estimate in randomized controlled trials of oral health interventions. BMC Med. Res. Methodol. 2018, 18, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Dettori, J.R.; Norvell, D.C. Intention-to-Treat: Is That Fair ? Glob. Spine J. 2020, 10, 361–363. [Google Scholar] [CrossRef]
- Kovach, C.R. Intention to Treat Necessary But Not Sufficient. Res. Gerontol. Nurs. 2020, 13, 62–63.
