Around 20% of PDAC patients in the United States are diagnosed with localized disease and are therefore eligible for surgical resection [
2,
4]. However, the majority of patients are diagnosed with locally advanced or metastasized disease at diagnosis, which leaves these patients with a poor survival rate [
2]. Limited knowledge of both clinical symptoms and biomarkers in the early stages of PDAC are major obstacles for early disease stage diagnosis [
9]. A number of genomic alterations have been associated with PDAC, but our understanding of their precise role in the onset and progression of disease is limited as the genomic studies associated with disease progression are sparse due to the lack of suitable models. For example, PDAC-derived xenografts have been established in immunocompromised mice by using tumor tissues or cell lines [
10,
11,
12,
13,
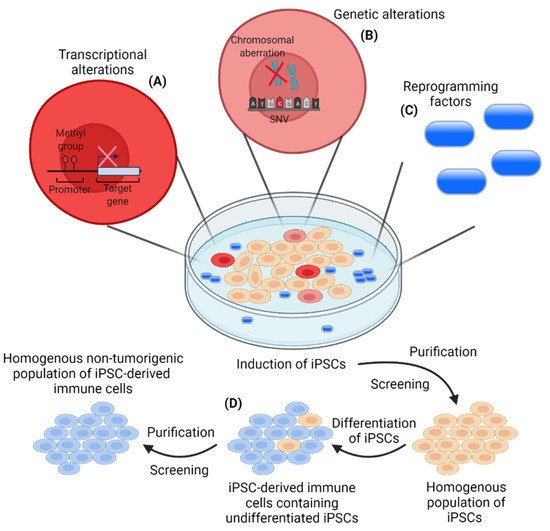
14]. These models solely reflect the invasive stages of PDAC and are not suitable for studies on the onset and early stages of PDAC. Novel models providing a better understanding of the biological processes at the basis of tumorigenesis are essential to improve diagnostics. To address this, iPSCs can provide a source of cells that better reflect the early stages of malignant transformation in PDAC.
iPSC-derived cancer-initiating cells have previously been reported for the establishment of xenograft models that reflect the malignant transformation in PDAC [
56,
71]. Mouse iPSCs from healthy cells have been differentiated in a controlled manner into PDAC progenitor cells [
56]. Xenograft models originating from these cells were able to give rise to precancerous lesions, including ADM and PanIN, as well as invasive PDAC. Exploiting a different approach, Kim et al. (2013) hypothesized that a subset of iPSCs induced from human PDAC cells would result in malignant iPSC lines, capable of undergoing early developmental stages of PDAC after engraftment into mice [
58]. One of the generated iPSC cell lines carried a
KRASG12D mutation and a deletion of
CDKN2A. The oncogenic
KRAS mutations are the most frequently detected oncogenic alteration in PDAC, being observed in >90% of patients [
72,
73,
74].
CDKN2A is a tumor suppressor in PDAC and has been described as being inactivated in approximately 50% of patients [
75,
76]. Xenografts originating from the
KRASG12D CDKN2A−\− iPSC cell line gave rise to PanIN-like lesions followed by progression to invasive PDAC [
58]. iPSC-based xenograft PDAC models originating from malignant cells demonstrate the potential of iPSCs to provide insights into PDAC onset and progression, including the identification of potential biomarkers for early diagnosis of PDAC. Another application where iPSCs might improve PDAC-modeling is the generation of iPSC-derived organoids containing different cell populations. iPSCs can be committed to a differentiation into the pancreatic exocrine lineage for the generation of acinar and ductal cells and, thus, provide great organoid-modeling possibilities for PDAC [
55,
57,
77,
78]. PDAC can develop from both acini and ducts, however knowledge on how these two cells of origin impact cell progression is scarce [
79]. Two studies recently assessed how the PDAC oncogenes
KRAS and
GNAS individually affect the growth and progression of PDAC in vitro and in vivo after engraftment of iPSC-derived acinar and ductal organoids in immunocompromised mice [
55,
57]. Both KRAS
G12D-mutated acinar and ductal organoids displayed proliferation in vivo, although the more invasive lesions were generated from acinar organoids. Phenotypically, both oncogenic alterations caused IPMN-like lesions in vivo. Furthermore, PanIN lesions and different stages of PDAC-like tumor formation were observed in xenografts from KRAS
G12D-mutated ductal and acinar organoids. In vitro, KRAS
G12D-mutated ductal organoids displayed epithelial-to-mesenchymal transition (EMT), which have been suggested to play a role in early tumor formation, metastasis, and chemoresistance in PDAC [
80,
81,
82]. In contrast, GNAS
R201C/H induced cystic growth in vitro in ductal organoids and to a lesser extend in acinar organoids. These iPSC-derived models provide vital knowledge of the malignant potential of different oncogenes in PDAC. Furthermore, the models provide great opportunities for in-depth assessment of early-stage disease development and progression.
In addition to the above-mentioned applications of iPSCs for disease modeling, iPSCs can also be differentiated into non-malignant cells of the TME. This opens up avenues for the development of complex multicellular models to test therapeutic interventions. For example, TAMs are thought to play an important role in PDAC tumorigenesis and may constitute promising clinical targets [
26]. Macrophage models for drug discovery have so far been dependent on a limited source of monocytes derived from PBMCs or animal bone marrow, which has limited the generation of models representative of tissue-resident macrophages (reviewed in [
83]). Gutbier and colleagues established a method for controlled large-scale iPSC-derived tissue-resident-resembling macrophages for efficient drug screening and discovery [
84]. Genetic manipulation of these iPSC-derived macrophages can be conducted to obtain the desired macrophage subtype. Additionally, cancer-initiating cells originating from iPSCs from healthy cells can also be differentiated into CAFs and vascular endothelial-like cells in vivo [
59,
60,
61]. Particularly, CAFs have been implicated as important players in the tumorigenesis of PDAC (reviewed in [
85]) [
86,
87]. CAFs constitute a promising therapeutic target in PDAC and several therapeutic strategies have been investigated preclinically and clinically (reviewed in [
88,
89]). The versatility of iPSCs to generate a variety of cells from the TME can support the development of models that include various cell types [
90]. Additionally, the directed differentiation towards a cell line of interest shows the potential of iPSC-derived models for drug screening at the molecular level.
iPSC-based xenografts and organoids provide excellent innovative possibilities for the modeling of PDAC, especially to study precancerous lesions and the development of this disease. Furthermore, the potential of iPSCs as a source for a variety of cells provides an opportunity for the establishment of multicellular models that better represent the PDAC TME. However, iPSC-based PDAC models are still in the early phase and further research is needed to fully exploit their potential.