Obstructive sleep apnea (OSA) is a form of sleep-disordered breathing consisting of upper airway collapse during sleep that results in repetitive arousals and desaturations. Estimates of disease prevalence range between 1% and 3% of the general pediatric population, with significant associated clinical consequences on individual morbidity. Consequences of untreated pediatric OSA include metabolic, endocrine, cardiovascular, and neurobehavioral implications with potential for long-term consequences. However, many pathogenic features of this syndrome in children remain unclear. Understanding principal mechanisms of OSA is critical for ultimately allowing for the development of therapeutic strategies. Much of the pathogenic mechanisms of OSA currently center around upper airway collapsibility.
1. Critical Pressure
Patients with OSA have been found to have increased pharyngeal critical pressure, resulting in upper airway collapsibility [
14,
15]. It is broadly recognized that pharyngeal collapse involves a complex interplay of neuromuscular and mechanical factors [
16]. The biomechanics of pharyngeal airflow obstruction is distinguished by upper airway occlusion and collapse during sleep followed by reopening upon wakefulness [
2,
17]. Occlusion and the stoppage of flow transpire when upstream pressure falls below critical pressure (Pcrit) [
18]. Pcrit is the pressure at which airway collapse occurs [
12,
19]. Adult OSA patients have significantly greater Pcrit levels [
20]. Similarly, children with OSA have positive Pcrit values, while children without OSA have the ability to maintain inspiratory airflow even at strikingly sub atmospheric pressures [
19].
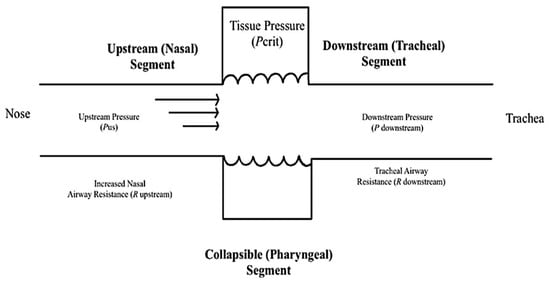
Pediatric airways have been observed to correlate to the Starling resistor model and Pcrit has been correlated with the degree of upper airway obstruction [
20,
21]. The notable features of the Starling resistor model include a collapsible segment dividing the fixed resistances of the rigid segments of the upstream nasal passages and downstream trachea (
Figure 2) [
2,
12,
16,
22]. These rigid segments are distinguished by intraluminal pressures, or upstream and downstream pressure, as well as upstream and downstream resistance to airflow. When the downstream and upstream pressures are less than the critical pressure, the airway closes. When the upstream pressure is greater than the critical pressure and the downstream pressure is below the critical pressure, the airway experiences inspiratory flow limitation (IFL) and can undergo a rapid oscillatory pattern between an open and a closed airway [
2]. When both the upstream and downstream pressures are above the critical pressure, the airway remains open and patent [
2,
23].
Figure 2. The Starling Resistor Model is a diagram that assists with the explanation of upper airway dynamics and the management of obstructive sleep apnea. The oropharynx is presented as a collapsible tube. Increased nasal airway resistance increases the probability that pharyngeal pressure will decrease below the CRITICAL pressure (Pcrit) and close the pharynx, which is a large proponent of obstructive events [
2].
IFL during sleep is a common occurrence that results from upper airway narrowing [
24]. IFL is described as the plateauing or flattening of inspiratory flow curve over time and is a non-invasive indicator of elevated upper airway resistance [
25]. Flow limitation can be found when a more negative intrathoracic pressure does not result in a corresponding increase in airflow [
24]. IFL is associated with a reduction in airflow, which is then followed by arousals and leads to the activation of upper airway dilator muscles for a compensatory increase in respiratory effort [
24]. Persistent airflow limitation leads to sleep fragmentation [
26]. Patients with IFL or upper airway resistance syndrome have been noted to present with hypotension and elevated vagal tone [
27]. Nonetheless, although critical pressure and flow limitation do not provide an indication of OSA severity, these characteristics have become highly recognized as patterns for the identification and analysis of sleep-disordered breathing [
14].
2. Oscillatory Patterns
In contrast to smooth oscillations in airflow, OSA features sudden variances in ventilatory compliance and upper airway patency [
2]. This notably deviates from the principles of time-invariance and linearity. Under these circumstances, ventilation is not determined by ventilatory drive, rather by the degree of upper airway patency. If ventilatory supply cannot match the demand required, the ventilatory drive significantly increases [
2].
There are two primary assumptions that assist with the determination of oscillatory sleep patterns. The first point explains that ventilation responses are determined by the ventilatory demand. Inherently, when an individual experiences periodic hypoventilation and their carbon dioxide concentration increases, it leads to a linear increase in ventilatory drive [
28]. Secondly, the mechanical components of respiration and ventilatory control remain comparatively constant across breathing cycles [
2,
28]. These two principles comprise the models that predict the smooth sinusoidal oscillations as observed in Cheyne–Stokes breathing.
OSA is notably a departure from the typical ventilatory pattern of smooth oscillations in airflow. It has been shown that obstructive apneas are characterized by dynamic pharyngeal obstruction during sleep with abrupt re-opening upon arousal [
29,
30]. The patency of the upper airway is quickly restored when arousal occurs, or apnea terminates, as it moves from a flow-limited-state to a non-flow-limited state [
2]. These repetitive demonstrations of mismatch between ventilatory demand and ventilatory supply, created by the mechanoreceptors, chemoreceptors, ventilatory drive, and transition between the flow limited state and non-flow limited state in the upper airway, are the primary mechanism behind the oscillatory pattern in the disruption of sleep.
Interventions such as surgical interventions, positional therapy, oral sleep appliances, and pharmacotherapy conjointly assist with combating the disturbances of upper airway mechanical loads or neuromuscular compensations [
31]. A comprehensive approach to treatment with multidisciplinary knowledge of the multiple intrinsic features that are responsible for upper airway collapsibility is crucial when treating these airway abnormalities [
32].
This entry is adapted from the peer-reviewed paper 10.3390/children8111032