1. Introduction
Since the first case of viral pneumonia was reported from Wuhan, China in late December of 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative pathogen for the Coronavirus disease 2019 (COVID-19) pandemic, has run rampant across the world
[1]. As of 30 September 2021, there have been 232,636,622 confirmed cases and 4,762,089 COVID deaths
[2]. As cases grew at an alarmingly exponential rate, it was quickly identified that COVID-19 could be transmitted through respiratory droplets and even through the aerosolization of droplet nuclei
[3][4]. Because of the pathology and progression of the disease towards respiratory failure, aerosol-generating medical procedures (AGMP) such as laryngoscopy, endotracheal intubation and extubation, tracheostomy, bronchoscopy and bronchoalveolar lavage, positive pressure ventilation, cardiopulmonary resuscitation with bag-valve-mask, suctioning, and nasopharyngeal aspiration and washing would be necessary to take care of patients with COVID-19 infection
[5]. Healthcare providers in the fields of anesthesiology, critical care medicine, emergency medicine, and otolaryngology, because of their roles in performing AGMPs for these patients, found themselves at risk of infection.
2. The Development of Barrier Systems
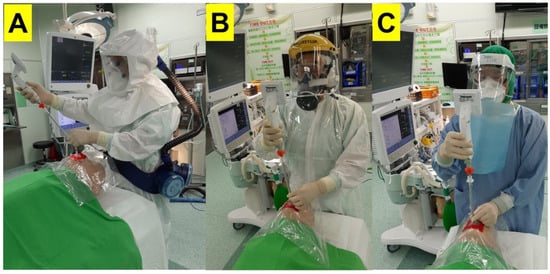
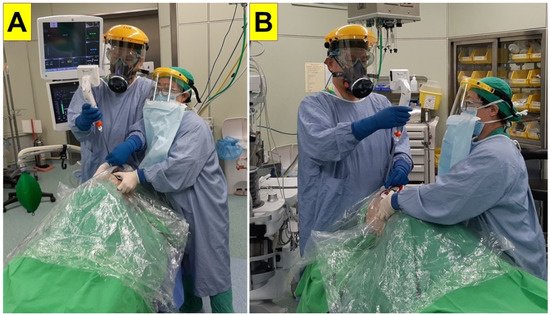
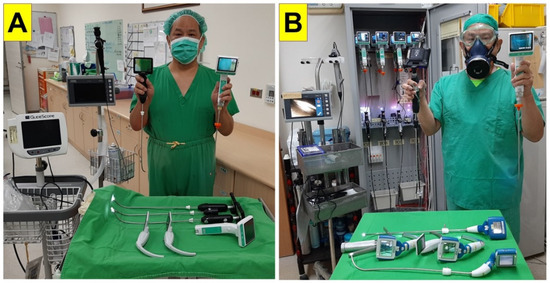
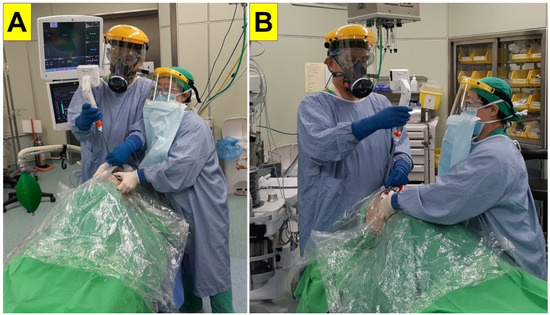
Personal protective equipment (PPE) is the primary basis for prevention of infection to healthcare workers while performing their tasks. Necessary PPE during the COVID-19 pandemic includes medical-grade masks, respirators, goggles, eye shields, face shields, gowns, gloves, shoe coverings, and head coverings
[6] (
Figure 1). Strict donning and doffing procedures are necessary to avoid accidental contamination of other work areas and the transmission to other patients and staff in the hospital
[7]. It was quickly realized that there were not sufficient stores of PPE to safely allow healthcare providers to perform daily patient care during the pandemic
[8]. Industry had a hard time ramping up production in a timely manner, and global disparities existed and have continued to exist. Without adequate PPE, coupled with other factors such as a lack of available testing, especially during the early stages of the pandemic
[9], the growing number of confirmed and suspected cases, as well as an overwhelming workload, frontline medical workers endured significant anxiety performing their expected duties as they worried about becoming infected, as well as transmitting the disease to family members
[10]. Currently, over 18 months into the pandemic, even with the rollout of vaccines, challenges to their widespread deployment as well as the proliferation of COVID-19 variants have prevented the world from curtailing the disease
[11].
Figure 1. Examples of personal protective equipment (PPE) used by medical staff while caring for patients undergoing aerosol generating medical procedures (AGMP) during the COVID-19 pandemic.
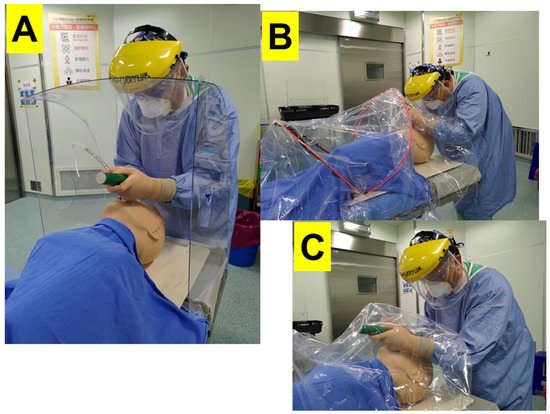
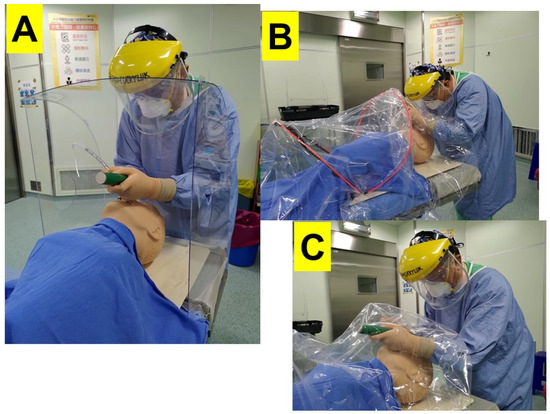
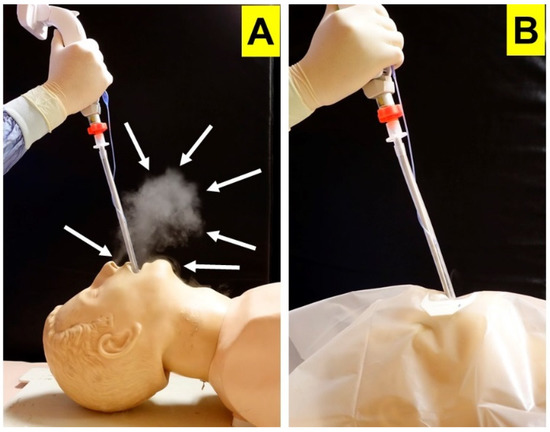
Without adequate PPE, health care professionals quickly looked to alternative means of protection against viral transmission. One strategy was the use of a transparent physical barriers. The first reported model was designed by a Taiwanese anesthesiologist who constructed a transparent four-sided box made of plexiglass that was placed between the patient and the airway manager during tracheal intubation
[12] (
Figure 2A). The plans for this structure were quickly shared on social media
[13], and Canneli et al. were the first to report on its use in the scientific literature
[14]. Subsequently, after this idea was promoted by news and social media and the device was proliferated and distributed to some users, multiple variations of barrier devices were introduced
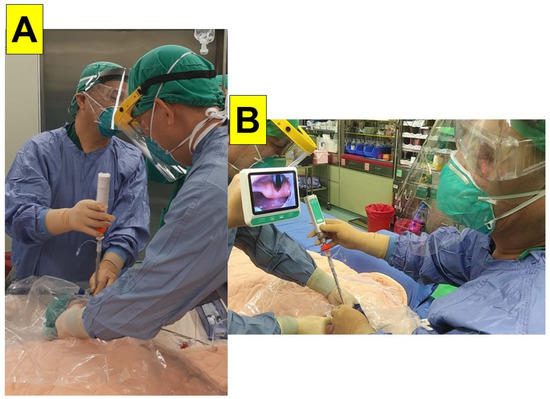
[15][16][17][18][19][20][21]. These barriers were applied not just for endotracheal intubation and airway management (
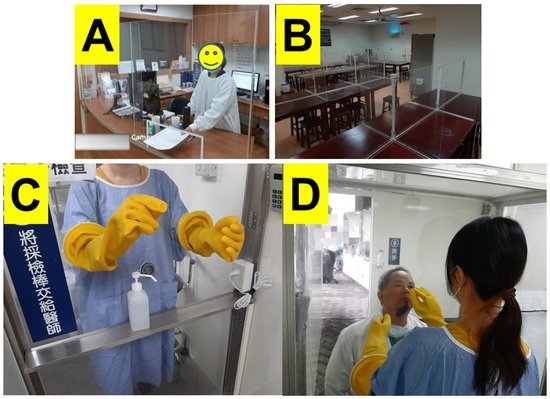
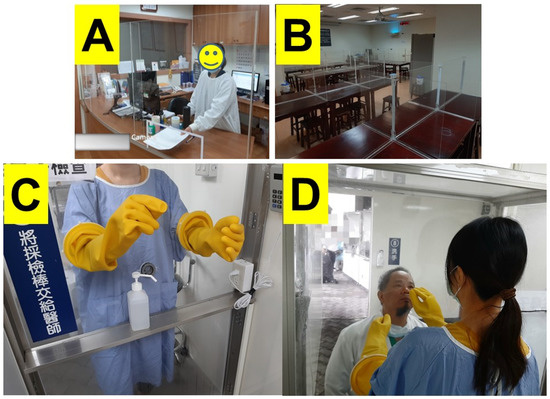
Figure 2B,C) but were utilized in various aspects of medical care, as well as applied to facilitate other forms of human interaction during the pandemic (
Figure 3). On 1 May 2020, the United States Food and Drug Administration (FDA) issued an emergency use authorization (EUA) for protective barrier enclosures
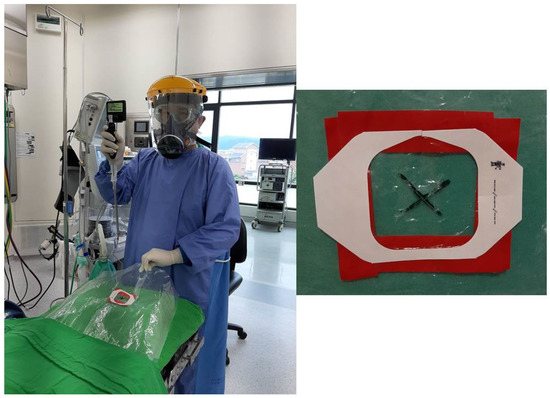
[22]. Over time, three general device types were identified: (1) rigid transparent box, (2) plastic sheet with frame, and (3) plastic sheet without frame (
Figure 2).
Figure 2. Various barrier systems utilized during performance of direct laryngoscopy and endotracheal intubation. (A) Rigid plastic box, (B) Plastic sheet with frame, (C) Plastic sheet without frame.
Figure 3. Various applications of transparent plastic barriers during the COVID-19 pandemic. (A) Front desk, (B) Cafeteria, (C,D) Nasopharyngeal COVID-19 testing.
Meanwhile, some airway management experts expressed their serious concerns on such a MacGyverism-style improvised medical device (e.g., the “aerosol box”) and argued about the untested effectiveness and safety issues of this EUA device
[23][24][25][26][27]. The main concerns raised against such physical barrier enclosure include the following: (1) restriction of hand movement of the intubator and assistants; (2) heavy and bulky plexiglass is difficult to carry and position or reposition in emergency situations; (3) limited for certain body habitus and positions; (4) confined space for airway maneuvering; (5) ergonomically difficult to manipulate airway equipment; (6) introducing other new risks of cross-contamination during the use, disinfection, and disposal processes; (7) increases the cognitive load of the staff and the risk of subsequent contamination; and (8) breaches in PPE due to a tear cut by the box edge. Some pointed out that such an unvalidated box design does not reduce risks (of being infected) and probably has unintended safety consequences to the airway managers, medical staff, and the patients.
3. Tracheal Intubation during the COVID-19 Pandemic
Tracheal or endotracheal intubation, the process of placing a breathing tube in the patient’s airway in order to maintain patency of the airway and provide oxygenation and ventilation, is often necessary in patients with critical respiratory illness
[28]. Traditionally, the intubation process involves manipulating the head and neck to align the oral, laryngeal, and pharyngeal axes, the placement of a laryngoscope into the oropharynx to retract the tongue and soft tissues of the mouth, and the introduction of an endotracheal tube (ETT), loaded onto a stylet, past the glottic opening
[29]. This procedure can be performed by a single operator, but an assistant often helps with the optimization of patient positioning such as jaw lift and lip retraction, handing the ETT-mounted stylet to the intubator, removing the stylet after the ETT has passed the vocal cords, and/or inflating the cuff of the endotracheal tube.
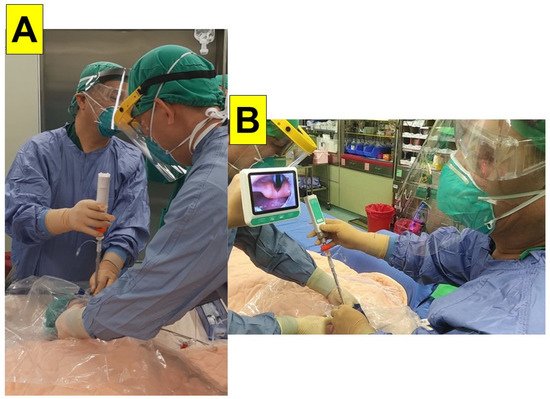
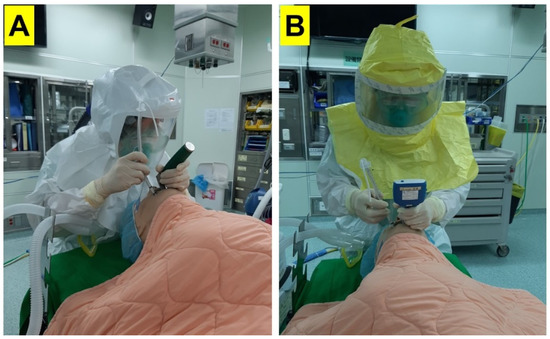
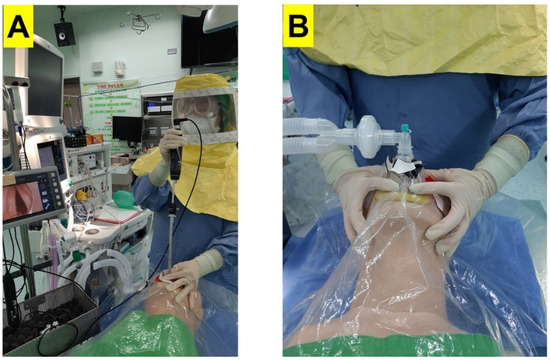
The intubation process places the healthcare professional at risk for COVID-19 infection as during traditional direct laryngoscopy, the anesthesia provider may need to be very close to the patient’s mouth in order to obtain a view of the glottis to advance the ETT (
Figure 2 and
Figure 4A). During the COVID-19 pandemic, it was subsequently recommended that videolaryngoscopy be preferentially utilized for tracheal intubation
[5][30][31]. The technology behind a videolaryngoscope is that a camera is placed at the tip of the device, which is projected to a monitor, either mounted on the device itself or on an independent stand. The airway manager is able to obtain a view of the patient’s airway and guide the ETT through the patient’s glottis without placing his or her face in close proximity to the patient’s airway (
Figure 4B). A recent Cochrane review had concluded that videolaryngoscopy may improve the success of tracheal intubation in adult patients, especially in difficult airways situations
[32]. However, it should be noted that because of the significant increased costs of a videolaryngoscope, this device may not be available in every setting across the world.
Figure 4. Proximity of the anesthesia provider to the patient’s airway during: (A) direct laryngoscopy, (B) indirect laryngoscopy using a videolaryngoscope (Courtesy photos reproduced from Cell Transplantation, SAGE Journals).
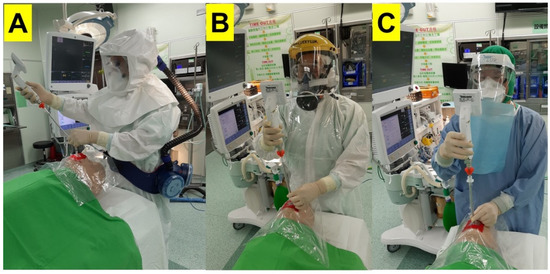
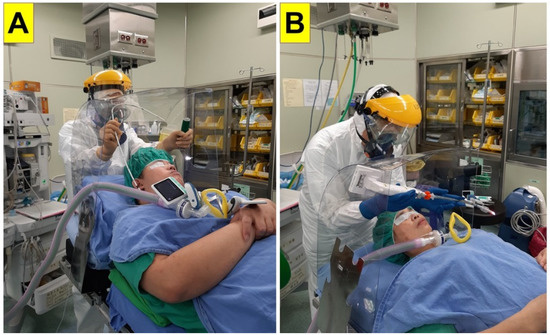
There are many videolaryngoscopes on the market today, with regional preferences in a range of designs and costs. A subset of the videolaryngoscope is the video intubating stylet. This device is a rigid or semi-rigid stylet equipped with a camera at the tip projecting to a separate monitor (
Figure 5 and
Figure 6). The ETT is mounted onto the video stylet in a similar fashion to a traditional stylet. The tip of the stylet may be designed to be malleable and anteflex. Because the camera resides within the stylet as opposed to on a separate videoscope, a laryngoscope is not necessary to perform endotracheal intubation (
Figure 6 and
Figure 7). “To see is to intubate” and “to see is to believe” are the mottos of the design of a video-assisted intubating stylet, a pioneering work that could change the face of airway management
[33].
Figure 5. Prevalence of using video intubating stylet technique for tracheal intubation in Taiwan. (A) Department of Anesthesia in a 729-bed community hospital; (B) Department of Anesthesia in a 1110-bed tertiary medical Center.
Figure 6. Real-world demonstration of endotracheal intubation utilizing the video intubating stylet and plastic sheet. A camera on the tip of the stylet captures a view of the glottis, which is projected to a separate monitor (For a demonstration video clip, see
Supplementary Material). (
A) Front view; (
B) Side view.
Figure 7. Mannequin demonstration of endotracheal intubation using the video intubating stylet through a piece of plastic sheet. (A) Stylet with loaded endotracheal tube introduced into patient’s mouth. (B) Stylet directed towards vocal cords under visual guidance from the monitor on the proximal end. (C) Endotracheal tube advanced off the stylet once past the vocal cords. PPE with powered air-purifying respirator, P-100, and N-95 respirators were shown in this figure. (Courtesy photos reproduced from Asian Journal of Anesthesiology, Taiwan Society of Anaesthesiologists with permission).
A potential benefit of the intubating stylet is that it may be a more economical alternative to the videolaryngoscope. In addition, many videolaryngoscopes utilize disposal laryngoscope tips/blades, which can minimize infection but are also recurring costs. Other potential benefits of the intubating stylet include a small profile, which results in less overall patient airway manipulation, such as less opening of the mouth and less lifting of the tongue. Because of its slim profile, the video stylet is more easily sanitized compared to other videolaryngoscopes. Even prior to the COVID-19 pandemic, at many institutions, the video intubating stylet had become the preferred modality for performing tracheal intubation
[34][35][36][37].
Table 1 and
Figure 5 show examples of high use coverage of video-assisted intubating stylets in the departments of anesthesia in Taiwan. Moreover, among 24 medical centers in Taiwan, the departments of anesthesia in 20 of them are equipped with video-assisted intubating stylets.
Table 1. Use coverage of video-assisted intubating stylet in the Hualien Tzu-Chi Medical Center, Hualien, Taiwan.
| |
2016 |
2017 |
2018 |
2019 |
2020 |
| Anesthesia Number |
16,077 |
17,831 |
17,998 |
19,307 |
19,721 |
| General Anesthesia Number |
15,339 |
16,893 |
17,497 |
18,481 |
19,009 |
| Laryngeal Mask Airway Number |
5544 |
5134 |
5816 |
5902 |
5863 |
| Endotracheal Tube Number |
5953 |
6504 |
6920 |
6966 |
7418 |
| Video Laryngoscope Number |
0 |
0 |
20 |
100 |
635 |
| Video Intubating Stylet Number |
5953
(100%) |
6504
(100%) |
6900
(99.7%) |
6866
(98.6%) |
6783
(91.4%) |