Diabetic retinopathy (DR) is one of the leading matters of vision-loss globally.
Even though there have been extensive efforts to reduce vision loss, the prevalence of DR is still uprising.
There are several pharmacological and surgical therapies currently used in clinics, but none of them has not been used as effective therapies at the early stage of DR.
In this topic review (Tomita and Lee et al.), we cover currently available strategies for DR treatment and collect new evidence for promising therapeutic strategies (PPAR alpha agonists) for treatment of the early stage of DR.
- diabetic retinopathy
- diabetic macula edema
- anti-VEGF therapy
- vitrectomy
- laser photocoagulation
- fenofibrate
Introduction
Diabetic retinopathy (DR) is a severe complication of diabetes mellitus (DM) and the main cause of vision loss (Bourne et al.). A dramatic socioeconomic cost is needed for DR treatment. Its prevalence has continuously increased globally (Leasher et al.). The public burden of DR let medical scientists search for better therapeutic approaches, as well as the update of current standards of DR treatment, including laser, anti-vascular endothelial growth factor (VEGF) therapy, steroid, and vitrectomy (Tomita and Lee et al.). Despite the fact that surgical or pharmacological strategy in DR has been advanced, the pathological mechanisms of DR even have yet to be clearly unraveled. In this topic review (Tomita and Lee et al.), we cover currently available treatment for DR and summarize new evidence for future therapeutic strategies (PPAR alpha agonists) for treatment of the early stage of DR.
Pathophysiology of DR
There have been various insights into the pathophysiology of DR (Figure 1). At first, DR is a microvascular disease, and hyperglycemia is the leading cause of retinal microvascular damage (Barot et al.)(Lutty). In this point of view, pathological metabolic pathways such as accumulation of AGEs and induction of PKC, the polyol, and the hexosamine pathways have been suggested in retinal microvascular injury (Tomita and Lee et al.).
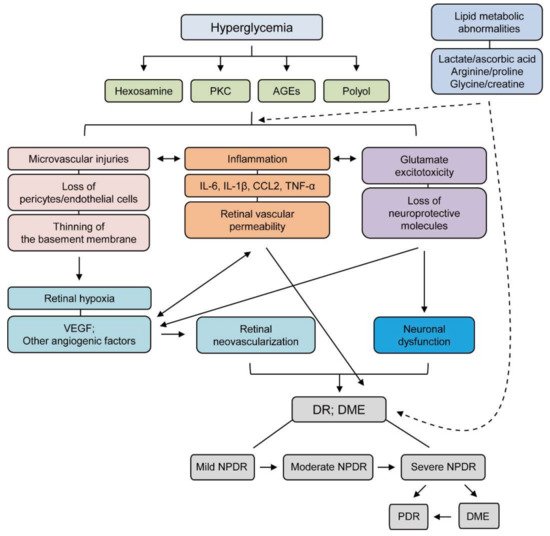
In the early stage of DR, pericyte loss leads to microvasculature destruction (Bergers and Song). It causes capillary occlusion, finally leading to retinal ischemia. Retinal ischemia induces retinal inflammation as well as retinal degeneration from the early stage to the chronic stage in DR (Wong et al.). Retinal inflammation under diabetic conditions is involved in a variety of inflammatory cytokines and chemokines such as (MCP-1/CCL2, TNF-α, IL-1β, IL-6). For retinal degeneration, various pro-apoptotic proteins such as Bax, caspase-3 have been nominated to induce retinal neuronal cell death in DR (Podesta et al.)(Kowluru and Koppolu). Taken together, various negative outcomes from microvascular abnormality to retinal cell death, are intermingled to the development and progression of DR. Recently, lipid metabolic dysregulation has been suggested for the development and progression of DR (Barba et al.)(Tomita et al.)(Haines et al.)(Paris et al.). Strong correlation of changes in plasma levels of HDL and LDL with the development of severities of DR as well as diabetes has been demonstrated. Dyslipidemia could be promoted under insulin-resistant conditions, which is important for the maintenance of glucose metabolism. Furthermore, increasing evidence showed that lipid-modifying drugs (fenofibrate and/or pemafibrate) could have possible therapeutic effects against DR conditions (Tomita and Lee et al.).
Current/Future Therapy in DR
At present, the most effective treatment for DR is blood glucose level control. More advanced conditions need laser, anti-VEGF therapy, steroid, and vitrectomy (Tomita and Lee et al.). However, lots of DR patients are still suffering from side effects of those treatments. In this regard, alternative promising treatments are needed in this current situation for DR treatment. As described in Figure 1, lipid and glucose dysregulations as well as retinal cell death, inflammation, and microvascular injury together affect the development and progression of DR. Furthermore, research outcomes from diabetic experimental models showed that peroxisome proliferator-activated receptor alpha (PPARα) activation showed promising therapeutic effects in cellular metabolism and inflammation, which can be used as a future promising treatment for DR.
For more information, please visit the following link (Tomita and Lee et al.).
This entry is adapted from the peer-reviewed paper 10.3390/jcm10204666
