Low-grade inflammation (LGI) has been suggested to be involved in the development of chronic diseases. Healthy dietary patterns, such as the Mediterranean diet (MD), may decrease the markers of LGI. Healthy Nordic diet (HND) has many similarities with MD, but its effects on LGI are less well known. Both of these dietary patterns emphasize the abundant use of fruits and vegetables (and berries in HND), whole grain products, fish, and vegetable oil (canola oil in HND and olive oil in MD), but restrict the use of saturated fat and red and processed meat.
- Nordic diet
- low-grade inflammation
- human
- diet
1. Introduction
2. HND and LGI in Observational Studies
3. Nordic Diet and LGI in Randomized Dietary Trials
3.1. Studies Including Selected Key Components of the HND
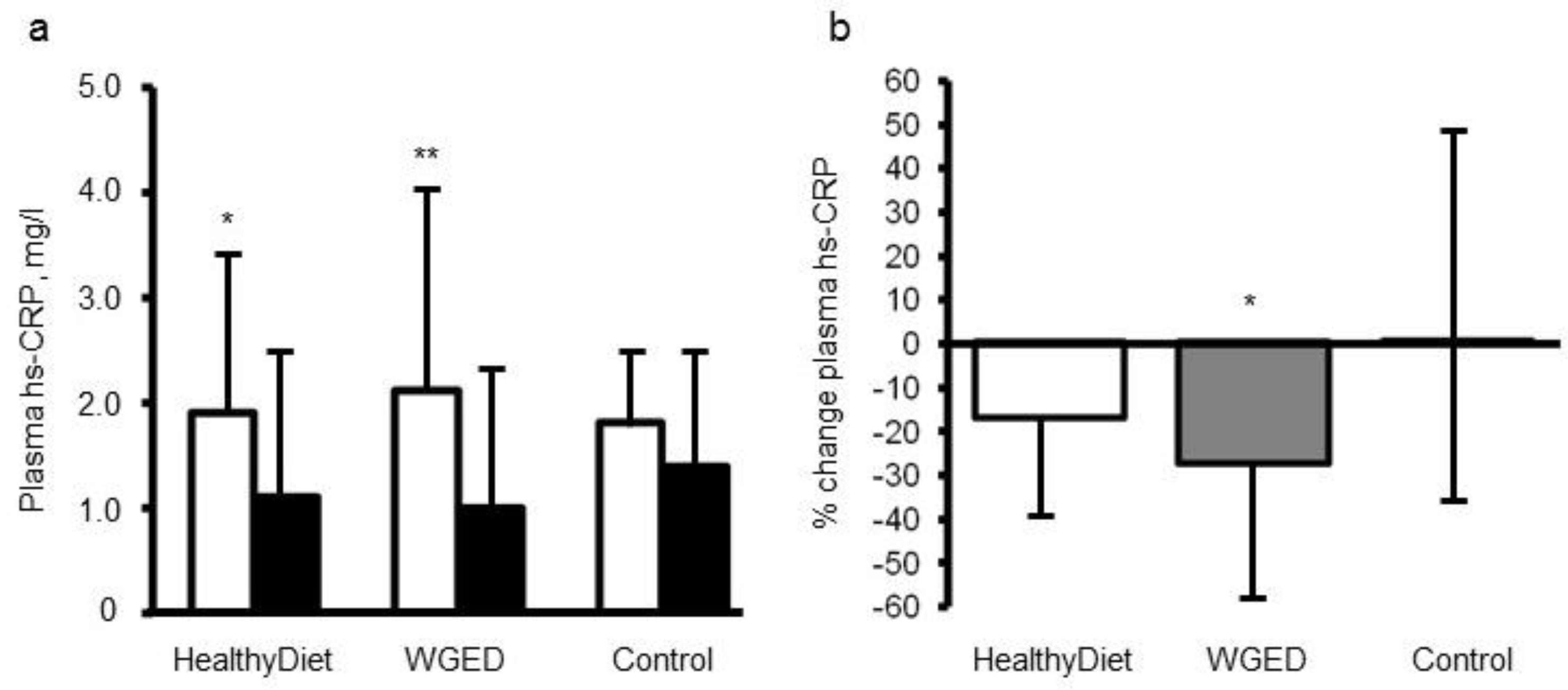 Figure 1. Plasma concentrations (a) and relative changes (b) of high sensitivity C-reactive protein (hsCRP) according to study group in the participants not using statins during the SYSDIMET intervention [25]. (a) White bars represent hsCRP concentrations at baseline and black bars after a 12 week consumption of HND (n = 27), Whole Grain Enriched Diet (WGED) (n = 24) or control diet (n = 25).* p < 0.05 and ** p < 0.001 for baseline vs. week 12 in Student’s paired test. (b) p = 0.04 for the group effect in general linear model univariate analysis. * p < 0.05 for the difference between WGED and control groups after Bonferroni correction for multiple comparisons. Values are median and interquartile range (IQR).
Figure 1. Plasma concentrations (a) and relative changes (b) of high sensitivity C-reactive protein (hsCRP) according to study group in the participants not using statins during the SYSDIMET intervention [25]. (a) White bars represent hsCRP concentrations at baseline and black bars after a 12 week consumption of HND (n = 27), Whole Grain Enriched Diet (WGED) (n = 24) or control diet (n = 25).* p < 0.05 and ** p < 0.001 for baseline vs. week 12 in Student’s paired test. (b) p = 0.04 for the group effect in general linear model univariate analysis. * p < 0.05 for the difference between WGED and control groups after Bonferroni correction for multiple comparisons. Values are median and interquartile range (IQR).3.2. HND in Controlled Dietary Trials
4. Summary
Quite few studies have investigated the effect of HND on LGI so far. Two observational studies have shown an inverse association between the adherence to the HND and concentration of hsCRP. In the intervention studies, a significant decrease in the concentration of hsCRP has been reported in two studies [28][25] out of four studies measuring hsCRP [35][32][28][25]. Furthermore, the HND has had beneficial effects on concentrations of other inflammatory markers, such as IL-1Ra [35] and Cathepsin S [30], and it has been shown to downregulate the gene expression of inflammation related genes in adipose tissue and PBMC [39][40]. It is noteworthy that these positive effects have been seen without significant weight loss. These results suggest that the HND may have anti-inflammatory effects, but more carefully controlled studies are needed to confirm the anti-inflammatory effects of the HND.
This entry is adapted from the peer-reviewed paper 10.3390/nu11061369
References
- Hotamisligil, G.S. Inflammation and Metabolic Disorders. Nature 2006, 444, 860–867.
- Hansson, G.K. Inflammation, Atherosclerosis, and Coronary Artery Disease. N. Engl. J. Med. 2005, 352, 1685–1695.
- Kern, L.; Mittenbuhler, M.J.; Vesting, A.J.; Ostermann, A.L.; Wunderlich, C.M.; Wunderlich, F.T. Obesity-Induced TNFalpha and IL-6 Signaling: The Missing Link between Obesity and Inflammation-Driven Liver and Colorectal Cancers. Cancers 2018, 11, 24.
- Costantini, E.; D’Angelo, C.; Reale, M. The Role of Immunosenescence in Neurodegenerative Diseases. Mediat. Inflamm. 2018, 2018, 6039171.
- Yudkin, J.S. Adipose Tissue, Insulin Action and Vascular Disease: Inflammatory Signals. Int. J. Obes. Relat. Metab. Disord. 2003, 27 (Suppl. 3), S25–S28.
- Unamuno, X.; Gomez-Ambrosi, J.; Rodriguez, A.; Becerril, S.; Fruhbeck, G.; Catalan, V. Adipokine Dysregulation and Adipose Tissue Inflammation in Human Obesity. Eur. J. Clin. Investig. 2018, 48, e12997.
- Chmelar, J.; Chung, K.J.; Chavakis, T. The Role of Innate Immune Cells in Obese Adipose Tissue Inflammation and Development of Insulin Resistance. Thromb. Haemost. 2013, 109, 399–406.
- de Mello, V.D.; Kolehmainen, M.; Pulkkinen, L.; Schwab, U.; Mager, U.; Laaksonen, D.E.; Niskanen, L.; Gylling, H.; Atalay, M.; Rauramaa, R.; et al. Downregulation of Genes Involved in NFkappaB Activation in Peripheral Blood Mononuclear Cells After Weight Loss is Associated with the Improvement of Insulin Sensitivity in Individuals with the Metabolic Syndrome: The GENOBIN Study. Diabetologia 2008, 51, 2060–2067.
- Ferreira, C.M.; Vieira, A.T.; Vinolo, M.A.; Oliveira, F.A.; Curi, R.; Martins Fdos, S. The Central Role of the Gut Microbiota in Chronic Inflammatory Diseases. J. Immunol. Res. 2014, 2014, 689492.
- Telle-Hansen, V.H.; Holven, K.B.; Ulven, S.M. Impact of a Healthy Dietary Pattern on Gut Microbiota and Systemic Inflammation in Humans. Nutrients 2018, 10, 1786.
- Minihane, A.M.; Vinoy, S.; Russell, W.R.; Baka, A.; Roche, H.M.; Tuohy, K.M.; Teeling, J.L.; Blaak, E.E.; Fenech, M.; Vauzour, D.; et al. Low-Grade Inflammation, Diet Composition and Health: Current Research Evidence and its Translation. Br. J. Nutr. 2015, 114, 999–1012.
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jonsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary Factors and Low-Grade Inflammation in Relation to Overweight and Obesity. Br. J. Nutr. 2011, 106 (Suppl. 3), S5–S78.
- Madsen, E.L.; Rissanen, A.; Bruun, J.M.; Skogstrand, K.; Tonstad, S.; Hougaard, D.M.; Richelsen, B. Weight Loss Larger than 10% is Needed for General Improvement of Levels of Circulating Adiponectin and Markers of Inflammation in Obese Subjects: A 3-Year Weight Loss Study. Eur. J. Endocrinol. 2008, 158, 179–187.
- Ziccardi, P.; Nappo, F.; Giugliano, G.; Esposito, K.; Marfella, R.; Cioffi, M.; D’Andrea, F.; Molinari, A.M.; Giugliano, D. Reduction of Inflammatory Cytokine Concentrations and Improvement of Endothelial Functions in Obese Women After Weight Loss Over One Year. Circulation 2002, 105, 804–809.
- Esposito, K.; Pontillo, A.; Di Palo, C.; Giugliano, G.; Masella, M.; Marfella, R.; Giugliano, D. Effect of Weight Loss and Lifestyle Changes on Vascular Inflammatory Markers in Obese Women: A Randomized Trial. JAMA 2003, 289, 1799–1804.
- Neale, E.P.; Batterham, M.J.; Tapsell, L.C. Consumption of a Healthy Dietary Pattern Results in Significant Reductions in C-Reactive Protein Levels in Adults: A Meta-Analysis. Nutr. Res. 2016, 36, 391–401.
- Schwingshackl, L.; Hoffmann, G. Mediterranean Dietary Pattern, Inflammation and Endothelial Function: A Systematic Review and Meta-Analysis of Intervention Trials. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 929–939.
- Uusitupa, M.; Schwab, U. Diet, Inflammation and Prediabetes-Impact of Quality of Diet. Can. J. Diabetes 2013, 37, 327–331.
- Kaluza, J.; Harris, H.; Melhus, H.; Michaelsson, K.; Wolk, A. Questionnaire-Based Anti-Inflammatory Diet Index as a Predictor of Low-Grade Systemic Inflammation. Antioxid. Redox Signal. 2018, 28, 78–84.
- Kanerva, N.; Loo, B.M.; Eriksson, J.G.; Leiviska, J.; Kaartinen, N.E.; Jula, A.; Mannisto, S. Associations of the Baltic Sea Diet with Obesity-Related Markers of Inflammation. Ann. Med. 2014, 46, 90–96.
- Joosten, M.M.; Witkamp, R.F.; Hendriks, H.F. Alterations in Total and High-Molecular-Weight Adiponectin After 3 Weeks of Moderate Alcohol Consumption in Premenopausal Women. Metabolism 2011, 60, 1058–1063.
- Kanerva, N.; Kaartinen, N.E.; Rissanen, H.; Knekt, P.; Eriksson, J.G.; Saaksjarvi, K.; Sundvall, J.; Mannisto, S. Associations of the Baltic Sea Diet with Cardiometabolic Risk Factors—A Meta-Analysis of Three Finnish Studies. Br. J. Nutr. 2014, 112, 616–626.
- Tian, Y.; Liimatainen, J.; Alanne, A.L.; Lindstedt, A.; Liu, P.; Sinkkonen, J.; Kallio, H.; Yang, B. Phenolic Compounds Extracted by Acidic Aqueous Ethanol from Berries and Leaves of Different Berry Plants. Food Chem. 2017, 220, 266–281.
- Kolehmainen, M.; Mykkanen, O.; Kirjavainen, P.V.; Leppanen, T.; Moilanen, E.; Adriaens, M.; Laaksonen, D.E.; Hallikainen, M.; Puupponen-Pimia, R.; Pulkkinen, L.; et al. Bilberries Reduce Low-Grade Inflammation in Individuals with Features of Metabolic Syndrome. Mol. Nutr. Food Res. 2012, 56, 1501–1510.
- De Mello, V.D.; Schwab, U.; Kolehmainen, M.; Koenig, W.; Siloaho, M.; Poutanen, K.; Mykkanen, H.; Uusitupa, M. A Diet High in Fatty Fish, Bilberries and Wholegrain Products Improves Markers of Endothelial Function and Inflammation in Individuals with Impaired Glucose Metabolism in a Randomised Controlled Trial: The Sysdimet Study. Diabetologia 2011, 54, 2755–2767.
- Adamsson, V.; Reumark, A.; Marklund, M.; Larsson, A.; Riserus, U. Role of a Prudent Breakfast in Improving Cardiometabolic Risk Factors in Subjects with Hypercholesterolemia: A Randomized Controlled Trial. Clin. Nutr. 2015, 34, 20–26.
- Fritzen, A.M.; Lundsgaard, A.M.; Jordy, A.B.; Poulsen, S.K.; Stender, S.; Pilegaard, H.; Astrup, A.; Larsen, T.M.; Wojtaszewski, J.F.; Richter, E.A.; et al. New Nordic Diet-Induced Weight Loss is Accompanied by Changes in Metabolism and AMPK Signaling in Adipose Tissue. J. Clin. Endocrinol. Metab. 2015, 100, 3509–3519.
- Poulsen, S.K.; Due, A.; Jordy, A.B.; Kiens, B.; Stark, K.D.; Stender, S.; Holst, C.; Astrup, A.; Larsen, T.M. Health Effect of the New Nordic Diet in Adults with Increased Waist Circumference: A 6-Mo Randomized Controlled Trial. Am. J. Clin. Nutr. 2014, 99, 35–45.
- Mithril, C.; Dragsted, L.O.; Meyer, C.; Tetens, I.; Biltoft-Jensen, A.; Astrup, A. Dietary Composition and Nutrient Content of the New Nordic Diet. Public Health Nutr. 2013, 16, 777–785.
- Jobs, E.; Adamsson, V.; Larsson, A.; Jobs, M.; Nerpin, E.; Ingelsson, E.; Arnlov, J.; Riserus, U. Influence of a Prudent Diet on Circulating Cathepsin S in Humans. Nutr. J. 2014, 13, 84.
- Poulsen, S.K.; Crone, C.; Astrup, A.; Larsen, T.M. Long-Term Adherence to the New Nordic Diet and the Effects on Body Weight, Anthropometry and Blood Pressure: A 12-Month Follow-Up Study. Eur. J. Nutr. 2015, 54, 67–76.
- Adamsson, V.; Reumark, A.; Fredriksson, I.B.; Hammarstrom, E.; Vessby, B.; Johansson, G.; Riserus, U. Effects of a Healthy Nordic Diet on Cardiovascular Risk Factors in Hypercholesterolaemic Subjects: A Randomized Controlled Trial (NORDIET). J. Intern. Med. 2011, 269, 150–159.
- Gupta, S.; Singh, R.K.; Dastidar, S.; Ray, A. Cysteine Cathepsin S as an Immunomodulatory Target: Present and Future Trends. Expert Opin. Ther. Targets 2008, 12, 291–299.
- Jobs, E.; Riserus, U.; Ingelsson, E.; Helmersson, J.; Nerpin, E.; Jobs, M.; Sundstrom, J.; Lind, L.; Larsson, A.; Basu, S.; et al. Serum Cathepsin S is Associated with Serum C-Reactive Protein and Interleukin-6 Independently of Obesity in Elderly Men. J. Clin. Endocrinol. Metab. 2010, 95, 4460–4464.
- Uusitupa, M.; Hermansen, K.; Savolainen, M.J.; Schwab, U.; Kolehmainen, M.; Brader, L.; Mortensen, L.S.; Cloetens, L.; Johansson-Persson, A.; Onning, G.; et al. Effects of an Isocaloric Healthy Nordic Diet on Insulin Sensitivity, Lipid Profile and Inflammation Markers in Metabolic Syndrome—A Randomized Study (SYSDIET). J. Intern. Med. 2013, 274, 52–66.
- Marklund, M.; Magnusdottir, O.K.; Rosqvist, F.; Cloetens, L.; Landberg, R.; Kolehmainen, M.; Brader, L.; Hermansen, K.; Poutanen, K.S.; Herzig, K.H.; et al. A Dietary Biomarker Approach Captures Compliance and Cardiometabolic Effects of a Healthy Nordic Diet in Individuals with Metabolic Syndrome. J. Nutr. 2014, 144, 1642–1649.
- Herder, C.; Brunner, E.J.; Rathmann, W.; Strassburger, K.; Tabak, A.G.; Schloot, N.C.; Witte, D.R. Elevated Levels of the Anti-Inflammatory Interleukin-1 Receptor Antagonist Precede the Onset of Type 2 Diabetes: The Whitehall II Study. Diabetes Care 2009, 32, 421–423.
- Lankinen, M.; Schwab, U.; Kolehmainen, M.; Paananen, J.; Nygren, H.; Seppanen-Laakso, T.; Poutanen, K.; Hyotylainen, T.; Riserus, U.; Savolainen, M.J.; et al. A Healthy Nordic Diet Alters the Plasma Lipidomic Profile in Adults with Features of Metabolic Syndrome in a Multicenter Randomized Dietary Intervention. J. Nutr. 2016, 146, 662–672.
- Kolehmainen, M.; Ulven, S.M.; Paananen, J.; de Mello, V.; Schwab, U.; Carlberg, C.; Myhrstad, M.; Pihlajamaki, J.; Dungner, E.; Sjolin, E.; et al. Healthy Nordic Diet Downregulates the Expression of Genes Involved in Inflammation in Subcutaneous Adipose Tissue in Individuals with Features of the Metabolic Syndrome. Am. J. Clin. Nutr. 2015, 101, 228–239.
- Myhrstad, M.C.W.; de Mello, V.D.; Dahlman, I.; Kolehmainen, M.; Paananen, J.; Rundblad, A.; Carlberg, C.; Olstad, O.K.; Pihlajamaki, J.; Holven, K.B.; et al. Healthy Nordic Diet Modulates the Expression of Genes Related to Mitochondrial Function and Immune Response in Peripheral Blood Mononuclear Cells from Subjects with Metabolic Syndrome-A SYSDIET Sub-Study. Mol. Nutr. Food Res. 2019, e1801405.
- de Mello, V.D.; Paananen, J.; Lindstrom, J.; Lankinen, M.A.; Shi, L.; Kuusisto, J.; Pihlajamaki, J.; Auriola, S.; Lehtonen, M.; Rolandsson, O.; et al. Indolepropionic Acid and Novel Lipid Metabolites are Associated with a Lower Risk of Type 2 Diabetes in the Finnish Diabetes Prevention Study. Sci. Rep. 2017, 7, 46337.
- Tuomainen, M.; Lindstrom, J.; Lehtonen, M.; Auriola, S.; Pihlajamaki, J.; Peltonen, M.; Tuomilehto, J.; Uusitupa, M.; de Mello, V.D.; Hanhineva, K. Associations of Serum Indolepropionic Acid, a Gut Microbiota Metabolite, with Type 2 Diabetes and Low-Grade Inflammation in High-Risk Individuals. Nutr. Diabetes 2018, 8, 35.
