The application of local anaesthetics is frequently involved in anaesthesia in the surgical treatment of various cancers. It is used in addition to or instead of general anaesthesia as a way to provide control of sensation and pain to specific regions or parts of the patients’ bodies. They are thought to reduce the requirement for volatile anaesthetics and opioids used in the surgery.
- Local anesthesia
- Cancer
- clinical
- Surgery
What is the local anaesthesia?
A prescription of clinical local anaesthetic usually includes the local anaesthetic agent, the vehicle, the antioxidant, the preservative, and the buffer. The application of local anaesthetics is frequently involved in anaesthesia in the surgical treatment of various cancers. In those cases, local anaesthesia is used in addition to or instead of general anaesthesia as a way to provide control of sensation and pain to specific regions or parts of the patients’ bodies. They are thought to reduce the requirement for inhaled general anaesthetics (volatile anaesthetics) and the dose of painkiller (opioids) and to control the stress response of neuroendocrine and immunosuppression caused by the surgery [1][2].
Use of local anaesthesia in cancer surgeries
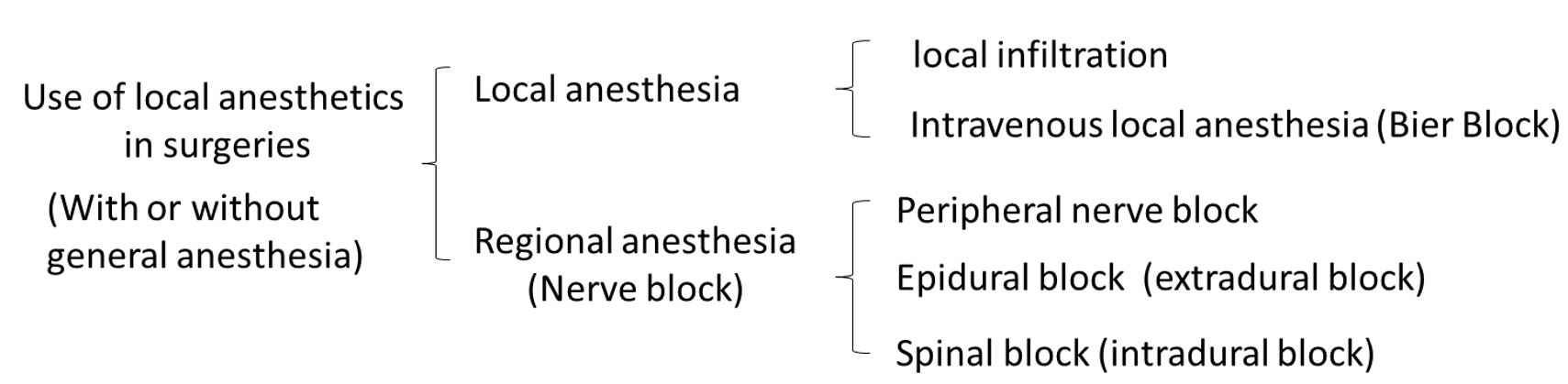
Local anaesthetics anaesthesia techniques frequently used in cancer surgeries include local infiltration, intravenous local anaesthesia, peripheral nerve blockade, epidural block, spinal anaesthesia, etc. This mini-review summarized and commented on the clinical use of Local anaesthetics in cancer surgeries.
local infiltration in cancer surgery
local infiltration is the injection of local anaesthetics into the tissues near the surgical site which may be used alone or in combination with sedation or general anaesthesia, depending on the size of the surgery, the time it will take, and the preferences of the patient. It is commonly applied in minor local surgeries like breast tumour biopsy or small melanoma resection. In local infiltrations, primary tumours directly exposed to local anaesthetics during the surgery period. The peak concentrations of local anaesthetics around the surgical site can reach an extremely high level and the anaesthetics can also enter the circulation leading to a prolonged effect. Although a large part of the infiltrated area will be resected with the tumor, the remains of the primary tumor and the circulating tumor cells may be influenced by the local anaesthetics. For example, after ropivacaine infiltration, the concentration of ropivacaine in circulation can remain around 3.5 to 3 μM after 24 hours [3]. Many in vitro and in vivo studies used 0.1 to 10 mM of local anaesthetics to mimic local infiltration clinical conditions [4]. Clinically relevant concentrations of the several local anaesthetics in blood and local tissues are presented in table 1.
Table 1 Clinically relevant concentrations of the commonly used local anaesthetics [4].
|
Agents |
Blood concentration (μM) |
Local tissue concentration (μM) |
|
Chloroprocaine |
15 |
34,670 (1%) |
|
Levobupivacaine |
2.5 |
8667 (0.25%) |
|
Bupivacaine |
2.8 |
8667 (0.25%) |
|
Mepivacaine |
10 |
40,592 (1%) |
|
Lidocaine |
10 |
17,500 (0.5%) |
|
Ropivacaine |
3.5 |
7288 (0.2%) |
Intravenous local anaesthesia in cancer surgery
Intravenous local anaesthesia, also named Bier's block, is an anaesthetic technique on the body's extremities where a local anaesthetic is injected intravenously and isolated from circulation in a target area. It had been occasionally applied in cancer surgeries for relatively short procedures on the distal upper extremity, but it is superseded by other anaesthetics approaches since it will excessively increase the circulatory concentration of the local anaesthetics and lead to severe intoxication.
Regional anaesthesia in cancer surgery
Regional anaesthesia (nerve blockage) is the injection of local anaesthetics near specific nerves to decrease pain in a certain part of the body, type of which includes peripheral nerve blockage, epidural block, and spinal anaesthesia. Peripheral nerve blockade is an injection of local anaesthetic agents in proximity end of the limb to block signals travelling along a nerve for a regional surgery such as lung cancer surgeries or extremity bone cancer surgeries. Epidural block (extradural block) and Spinal blockage (spinal block, subarachnoid block, intradural block, and intrathecal block) are techniques that block the spinal nerves to achieve para-anaesthetics for colon cancer surgeries or lower extremity bone cancer surgeries. An epidural block is an injection of local anaesthetics into the epidural space around the spinal cord while the Spinal blockage is into the subarachnoid space inside the spinal cord. In nerve blockage, primary cancer cells do not directly expose to local anaesthetics, but the agents are distributed in patients’ circulation, which most metastatic cells journey through, thereby, in these cases, local anaesthetics may affect the colonization and migration of cancer cells. The practical clinical approach for regional anaesthesia is to give a bolus dose or a bolus dose followed by constant infusion, hence it will reach a peak circulation concentration. For example, after epidural anaesthesia with lidocaine and bupivacaine, the peak circulation concentrations are around 40 μM and 10 μM respectively [5].
The article has been published on
https://www.thegms.co/publications/archives/
PDF is available on
References
- Piegeler, T.; Votta-Velis, E.G.; Bakhshi, F.R.; Mao, M.; Carnegie, G.; Bonini, M.G.; Schwartz, D.E.; Borgeat, A.; Beck-Schimmer, B.; Minshall, R.D. Endothelial barrier protection by local anesthetics: ropivacaine and lidocaine block tumor necrosis factor-α-induced endothelial cell Src activation. Anesthesiology 2014, 120, 1414-1428, doi:10.1097/aln.0000000000000174.
- Votta-Velis, E.G.; Piegeler, T.; Minshall, R.D.; Aguirre, J.; Beck-Schimmer, B.; Schwartz, D.E.; Borgeat, A. Regional anaesthesia and cancer metastases: the implication of local anaesthetics. Acta Anaesthesiol Scand 2013, 57, 1211-1229, doi:10.1111/aas.12210.
- Gill, A.M.; Scott, N.B.; Abbas, M.; Watson, D.G.; Place, K.; McDonald, D.A. Ropivacaine plasma levels following local infiltration analgesia for primary total hip arthroplasty. Anaesthesia 2014, 69, 368-373, doi:10.1111/anae.12559.
- Li, R.; Xiao, C.; Liu, H.; Huang, Y.; Dilger, J.P.; Lin, J. Effects of local anesthetics on breast cancer cell viability and migration. BMC cancer 2018, 18, 666.
- Burm, A.G.; van Kleef, J.W.; Gladines, M.P.; Olthof, G.; Spierdijk, J. Epidural anesthesia with lidocaine and bupivacaine: effects of epinephrine on the plasma concentration profiles. Anesth Analg 1986, 65, 1281-1284.