Pelvic girdle pain (PGP) refers specifically to musculoskeletal pain localised to the pelvic ring and can be present at its anterior and/or posterior aspects. Causes such as trauma, infection and pregnancy have been well-established, while patients with hypermobile joints are at greater risk of developing PGP.
- pelvic girdle pain
- pelvic pain
- pelvic instability
- pubic symphysis
1. Introduction
Pelvic girdle pain (PGP) refers specifically to musculoskeletal pain localised to the level of the posterior iliac crest and the gluteal fold, and occasionally over the anterior and posterior elements of the bony pelvis[1]. There are many causes of pelvic pain overall, including trauma, infections of soft tissue, bone or underlying viscera, lower-back pain syndromes, pregnancy, joint hypermobility and disorders of connective tissues[1][2]. Given the broad range of possible causes, when managing these patients, it is important for an extensive history and clinical examination to be conducted, followed by appropriate investigations to facilitate accurate diagnosis—and to distinguish between aetiologies.
2. PGP, Hypermobility Spectrum Disorder & Hypermobility-Type Ehlers-Danlos Syndrome
Joint hypermobility (JH) places a great level of strain on an affected individual’s musculoskeletal system. JH occurs secondary to increased elasticity of the soft tissues that support a joint, tendons and ligaments, which allows a greater range of motion[3]. A tool such as the Beighton score which uses five simple manoeuvres can be used to screen individuals for hypermobile joints in clinical practice (Figure 1). Complications can include joint pain, dislocations and instability which can limit daily activities and quality of life. Previous research has highlighted that there may be a link between JH and development of osteoarthritis secondary to the increased stress placed on joints, however studies have reported mixed findings[4][5][6][7][8][9]. Although JH has disadvantages linked to increased risk of injury and anxiety, particularly in contact sports, in others such as gymnastics and ballet it may in fact be advantageous[10][11][12][13].
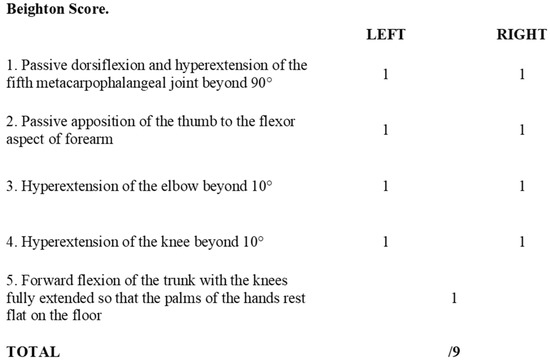
Figure 1. Beighton score. Adapted from Beighton et al., 1973[14].
Patients with joint hypermobility (JH) are classified according to their position on the hypermobility spectrum, which ranges in severity from asymptomatic joint hypermobility, to hypermobility-type Ehlers-Danlos Syndrome (hEDS)[15]. This allows for inclusion of patients with a less severe constellation of symptoms, who may not necessarily meet criteria for diagnosis of a specific connective tissue disorder (Table 1).
Table 1. Spectrum of joint hypermobility phenotypes. Adapted from Castori et al., 2017[15].
| Asymptomatic Generalised Joint Hypermobility (Asymptomatic GJH) |
| Asymptomatic Peripheral Joint Hypermobility (Asymptomatic PJH) |
| Asymptomatic Localised Joint Hypermobility (Asymptomatic LJH) |
| Generalised Hypermobility Spectrum Disorder (G-HSD) |
| Peripheral Hypermobility Spectrum Disorder (P-HSD) |
| Localised Hypermobility Spectrum Disorder (L-HSD) |
| Historical Hypermobility Spectrum Disorder (H-HSD) |
| Hypermobility-Type Ehlers-Danlos Syndrome (hEDS) |
The classification framework for overall Joint Hypermobility (JH) and Ehlers-Danlos Syndrome subtypes were updated in 2017, before which the definitions were quite different. Prior to this, the commonly used terms were ‘joint hypermobility syndrome’ and hEDS alone.[15][16] One must bear this in mind when reading older literature.
Ehlers-Danlos Syndrome (EDS) is a genetically inherited connective tissue disorder characterised by hypermobile joints, friable tissues and hyperextensible skin. The first attempt to classify the condition was in 1936 by Weber, who termed it ‘Ehlers-Danlos Syndrome’ in honour of early published cases by these authors[17] In 2017, the current revised classification known as the international classification of EDS was created[16], which updated the previous set of definitions known as the 1998 Villefranche Nosology. This builds on an increased understanding of EDS: further subclassifications were generated, which refer to inheritance patterns, genetic abnormalities and affected proteins. The 2017 international classification lists clinical criteria that are suggestive of 13 EDS subtypes. The five most common subtypes are summarised in Table 2. The revised 2017 classification has clear, defined criteria for the diagnosis of hEDS, and a less-restrictive diagnosis criteria for HSD when patients may present with some features of hEDS, but not enough to be given a diagnosis of hEDS[15][16]. It is important to note that joint hypermobility (JH) can present in several subtypes of EDS, and not just hEDS[15][16].
Table 2. Summary of the five most common Ehlers-Danlos Syndrome (EDS) subtypes. Adapted from Malfait et al., 2017[16].
|
EDS Subtype |
Inheritance Pattern |
Genetic Basis |
Protein Affected |
Common Clinical Signs (Not Extensive) |
|
|
Classical EDS |
Autosomal dominant |
COL5A1 |
Type V collagen |
Skin: hyperextensible, fragile, soft, atrophic scarring |
|
|
COL1A1 |
Type I collagen |
Other: generalised-JH, hernias |
|
||
|
Classical-like EDS |
Autosomal recessive |
TNXB |
Tenascin XB |
Skin: hyperextensible, velvety, absence of atrophic scarring, easy bruising skin |
|
|
Other: generalised-JH, foot deformities, oedema, pelvic organ prolapse |
|
||||
|
Cardiac-Valvular EDS |
Autosomal recessive |
COL1A2 |
Type I collagen |
Progressive cardiac valve disease |
|
|
Skin: hyperextensible, atrophic scars, easy bruising |
|
||||
|
Other: Joint hypermobility, hernia, foot deformity |
|
||||
|
Vascular EDS |
Autosomal dominant |
COL3A1 |
Type III collagen |
Arterial rupture at young age, spontaneous sigmoid colon perforation, uterine rupture, peripartum perineal tears, carotid-cavernous sinus fistula, thin skin, varicose vein |
|
|
Type I collagen |
|||||
|
COL1A1 |
|
||||
|
Hypermobile EDS |
Autosomal dominant |
Unknown |
Unknown |
Generalised-JH, absence of skin fragility, mild skin hyperextensibility, unexplained striae, pelvic organ prolapse, dental crowding, hernias |
|
As there is no investigation to diagnose hEDS, it is still diagnosed clinically. Attempts to find a genetic test have proved difficult due to the clinical and genetic heterogeneity of this syndrome[18][19][20]. An in vitro study utilising skin biopsies from patients with hEDS and hypermobility spectrum disorder (HSD) has identified a possible signalling pathway (αvβ3-ILK-Snail1/Slug axis) which promotes the transition of fibroblasts to myofibroblasts in hEDS and HSD patients, which was absent in biopsies from patients with classical EDS and vascular EDS[21]. Although further research is required on a larger sample of patients, this provides some insight into future directions of molecular testing which could support a clinical diagnosis of hEDS and HSD. Interestingly, further research is still required to differentiate between hEDS and HSD.
Given the relatively recent changes in 2017 used to describe JH, HSD and hEDS, it is difficult to determine the exact prevalence of these conditions. The distribution of hypermobility between the genders is however well reported to show a female predominance[14][22][23][24][25][26][27]. This greater prevalence in females has identified an increased concern related to pregnancy. Studies have found that females with JH are at increased odds of developing PGP during pregnancy than those who do not have JH[28]. A study investigating pregnancy complications in those with EDS identified that the prevalence of pelvic pain and instability was almost four-times greater than those without EDS [29]. Small case series have further data to support this with up to 88% of hEDS patients experiencing PGP during pregnancy[30]. The current available data is limited by study design and would benefit from larger prospective studies using the newer 2017 EDS criteria for diagnosis. This may however prove challenging due to undiagnosed cases, limited understanding, and rarity of cases.
2. PGP Challenges
PGP is a complex disorder that is difficult to diagnose when considering its overlap in presentation with pathology of the pelvic viscera and spinal pathologies, making it primarily a diagnosis by exclusion. Assessment of existing literature is further challenged by the variety of names used to describe this condition, with similar difficulties associated with HSD and hEDS. Modern literature has however become more standardised by using PGP and HSD since the creation of newer classifications and guidelines[16][31]. This proved challenging when conducting a literature search for this review, where many papers were excluded due to being irrelevant. The broad search implemented was necessary, as when searching with the correct terms as discussed above, no results were found. It is for this reason that a broader search was conducted, with a screening process to filter the many publications relating to other causes of pelvic pain, which were not musculoskeletal.
Regardless, this review has identified HSD as a potential risk factor for the development of PGP, requiring a multidisciplinary approach to manage, provide adequate support, and appropriately diagnose rare conditions such as EDS. If not already incorporated into current clinical care pathways, a suggestion would be made to involve a rheumatologist if there is suspicion of HSD/hEDS, in order to ensure a holistic approach is pursued to identify any associated connective tissue problems, particularly those that are life-threatening such as aortic dilatations. Increasing awareness of patients and clinicians is also vital to ensure appropriate labelling of diagnoses related to PGP or HSD, as there is concern of incorrect or underdiagnosis of disease, with unknown exact prevalence[24].
A further challenge we face when interpreting current literature on management of outcomes is related to the broad variety of PROMs used in studies, particularly global health measures such as the SF-36, ODI, EQ-5D and Short Musculoskeletal Function Assessment which are not disease-specific as well as limiting translation and comparison of study findings, particularly where identical questionnaires were reported on differently[32][33]. PROMs related to the pelvis exist, such as the Pelvic Girdle Questionnaire, Majeed, Iowa and Orlando scores[34][35][36][37]. The latter three have been reviewed with concerns highlighted lack of emotional and mental health assessment and limited by floor and ceiling effects where individuals with impaired function may score well and vice versa. Moreover, they have unknown reliability and responsiveness particularly in longitudinal studies[38][39]. The Pelvic Girdle Questionnaire has been widely validated for use in pelvic pain in pregnant and postpartum individuals, however its use has not been validated in patients with PGP secondary to trauma and other causes[34][40][41][42][43][44][45][46]. The Pelvic Girdle Questionnaire does not contain any items that are gender or pregnancy specific. A future study exploring its validity as a functional outcome measure in trauma, pubic symphysis and SIJ dysfunction patients may highlight it as a suitable tool for such patients after its success in pregnant and postpartum women, potentially preventing the need to develop a new measure.
Several recommendations can be made based on the findings of this literature review. Upon diagnosis of PGP, completion of appropriate PROMs would be advised to monitor global health, functional status, and mental health using validated measures. This allows further assessment as to whether patients with impaired mental health would benefit from a psychological or psychiatric referral to improve their symptoms and rehabilitation. In addition, it would allow monitoring of functional status which can be repeated throughout treatment and allow more meaningful assessment of post-intervention outcomes. For pregnancy-related PGP, we would advise the use of the Pelvic Girdle Questionnaire as it is well-validated as previously discussed. For other causes of PGP we advise the use of validated global measures such as the VAS, EQ-5D and SF-36 or ODI, which can be compared to population norms, as the application of pelvic-specific outcomes for this population require further assessment[33][47][48]
It would also be advised to screen patients for JH in a formal manner using the Beighton score, or Five-Point Questionnaire if the Beighton score cannot be applied in clinic, or due to contraindications described earlier in the ‘Diagnosis’ section. Patients should be screened for further features of EDS to assist in the decision to make a referral to a Rheumatologist or EDS specialist, so patients have access to appropriate support services.
This entry is adapted from the peer-reviewed paper 10.3390/jcm9123992
References
- Verstraete, E.; Vanderstraeten, G.; Parewijck, W. Pelvic Girdle Pain during or after Pregnancy: A review of recent evidence and a clinical care path proposal. Facts Views Vis. Obgyn. 2013, 5, 33–43.
- Kanakaris, N.K.; Roberts, C.S.; Giannoudis, P.V. Pregnancy-related pelvic girdle pain: An update. BMC Med. 2011, 9, 15.
- Shirley, E.D.; DeMaio, M.; Bodurtha, J. Ehlers-Danlos Syndrome in Orthopaedics: Etiology, Diagnosis, and Treatment Implications. Sports Health 2012, 4, 394–403.
- Gürer, G.; Bozbas, G.T.; Tuncer, T.; Unubol, A.I.; Ucar, U.G.; Memetoglu, O.I. Frequency of joint hypermobility in Turkish patients with knee osteoarthritis: A cross sectional multicenter study. Int. J. Rheum. Dis. 2018, 21.
- Gullo, T.R.; Golightly, Y.M.; Flowers, P.; Jordan, J.M.; Renner, J.B.; Schwartz, T.A.; Kraus, V.B.; Hannan, M.T.; Cleveland, R.J.; Nelson, A.E. Joint hypermobility is not positively associated with prevalent multiple joint osteoarthritis: A cross-sectional study of older adults. BMC Musculoskelet. Disord. 2019, 20.
- Flowers, P.P.E.; Cleveland, R.J.; Schwartz, T.A.; Nelson, A.E.; Kraus, V.B.; Hillstrom, H.J.; Goode, A.P.; Hannan, M.T.; Renner, J.B.; Jordan, J.M.; et al. Association between general joint hypermobility and knee, hip, and lumbar spine osteoarthritis by race: A cross-sectional study. Arthritis Res. Ther. 2018, 20.
- Goode, A.P.; Cleveland, R.J.; Schwartz, T.A.; Nelson, A.E.; Kraus, V.B.; Hillstrom, H.J.; Hannan, M.T.; Flowers, P.; Renner, J.B.; Jordan, J.M.; et al. Relationship of joint hypermobility with low Back pain and lumbar spine osteoarthritis. BMC Musculoskelet. Disord. 2019, 20.
- Dolan, A.L.; Hart, D.J.; Doyle, D.V.; Grahame, R.; Spector, T.D. The relationship of joint hypermobility, bone mineral density, and osteoarthritis in the general population: The Chingford Study. J. Rheumatol. 2003, 30, 799–803.
- Reinstein, E.; Pariani, M.; Lachman, R.S.; Nemec, S.; Rimoin, D.L. Early-Onset Osteoarthritis in Ehlers-Danlos Syndrome type VIII. Am. J. Med. Genet. A. 2012, 158A, 938–941.
- Briggs, J.; McCormack, M.; Hakim, A.J.; Grahame, R. Injury and joint hypermobility syndrome in ballet dancers--a 5-year follow-up. Rheumatology 2009, 48, 1613–1614.
- Grahame, R.; Jenkins, J.M. Joint hypermobility—Asset or liability? A study of joint mobility in ballet dancers. Ann. Rheum. Dis. 1972, 31, 109–111.
- Bulbena, A.; Duro, J.C.; Mateo, A.; Porta, M.; Vallejo, J. Joint hypermobility syndrome and anxiety disorders. Lancet 1988, 332, 694.
- Nicholas, J.A. Injuries to knee ligaments. Relationship to looseness and tightness in football players. JAMA 1970, 212, 2236–2239.
- Beighton, P.; Solomon, L.; Soskolne, C.L. Articular mobility in an African population. Ann. Rheum. Dis. 1973, 32, 413–418, Epub 01 September 1973.
- Castori, M.; Tinkle, B.; Levy, H.; Grahame, R.; Malfait, F.; Hakim, A. A framework for the classification of joint hypermobility and related conditions. Am. J. Med Genet. Part C Semin. Med Genet. 2017, 175.
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 International Classification of the Ehlers-Danlos Syndromes. Am. J. Med. Genet. Part C Semin. Med. Genet. 2017, 175, 8–26.
- Parapia, L.A.; Jackson, C. Ehlers-Danlos syndrome—A historical review. Br. J. Haematol. 2008, 141, 32–35.
- De Wandele, I.; Rombaut, L.; Malfait, F.; De Backer, T.; De Paepe, A.; Calders, P. Clinical heterogeneity in patients with the hypermobility type of Ehlers-Danlos syndrome. Res. Dev. Disabil. 2013, 34, 873–881.
- Tinkle, B.T.; Bird, H.A.; Grahame, R.; Lavallee, M.; Levy, H.P.; Sillence, D. The lack of clinical distinction between the hypermobility type of Ehlers-Danlos syndrome and the joint hypermobility syndrome (a.k.a. hypermobility syndrome). Am. J. Med. Genet. A 2009, 149a, 2368–2370.
- Forghani, I. Updates in Clinical and Genetics Aspects of Hypermobile Ehlers Danlos Syndrome. Balk. Med. J. 2019, 36, 12–16.
- Zoppi, N.; Chiarelli, N.; Binetti, S.; Ritelli, M.; Colombi, M. Dermal fibroblast-to-myofibroblast transition sustained by αvß3 integrin-ILK-Snail1/Slug signaling is a common feature for hypermobile Ehlers-Danlos syndrome and hypermobility spectrum disorders. Biochim. Biophys. Acta Mol. Basis Dis. 2018, 1864, 1010–1023.
- Mulvey, M.R.; Macfarlane, G.J.; Beasley, M.; Symmons, D.P.M.; Lovell, K.; Keeley, P.; Woby, S.; McBeth, J. Modest association of joint hypermobility with disabling and limiting musculoskeletal pain: Results from a large-scale general population-based survey. Arthritis Care Res. 2013, 65, 1325–1333.
- Larsson, L.G.; Baum, J.; Mudholkar, G.S. Hypermobility: Features and differential incidence between the sexes. Arthritis Rheum. 1987, 30, 1426–1430.
- Demmler, J.C.; Atkinson, M.D.; Reinhold, E.J.; Choy, E.; Lyons, R.A.; Brophy, S.T. Diagnosed prevalence of Ehlers-Danlos syndrome and hypermobility spectrum disorder in Wales, UK: A national electronic cohort study and case–control comparison. BMJ Open 2019, 9.
- Al-Rawi, Z.S.; Al-Aszawi, A.J.; Al-Chalabi, T. Joint mobility among university students in Iraq. Br. J. Rheumatol. 1985, 24, 326–331.
- Gedalia, A.; Person, D.A.; Brewer, E.J., Jr.; Giannini, E.H. Hypermobility of the joints in juvenile episodic arthritis/arthralgia. J Pediatr. 1985, 107, 873–876.
- Decoster, L.C.; Vailas, J.C.; Lindsay, R.H.; Williams, G.R. Prevalence and features of joint hypermobility among adolescent athletes. Arch. Pediatr. Adolesc. Med. 1997, 151, 989–992.
- Ahlqvist, K.; Bjelland, E.K.; Pingel, R.; Schlager, A.; Nilsson-Wikmar, L.; Kristiansson, P. The Association of Self-Reported Generalized Joint Hypermobility with pelvic girdle pain during pregnancy: A retrospective cohort study. BMC Musculoskelet. Disord. 2020, 21, 474.
- Lind, J.; Wallenburg, H.C. Pregnancy and the Ehlers-Danlos syndrome: A retrospective study in a Dutch population. Acta Obstet. Gynecol. Scand. 2002, 81, 293–300.
- Karthikeyan, A.; Venkat-Raman, N. Hypermobile Ehlers-Danlos syndrome and pregnancy. Obstet. Med. 2018, 11, 104–109.
- Vleeming, A.; Albert, H.B.; Östgaard, H.C.; Sturesson, B.; Stuge, B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur. Spine J. 2008, 17, 794–819.
- Wuytack, F.; O’Donovan, M. Outcomes and outcomes measurements used in intervention studies of pelvic girdle pain and lumbopelvic pain: A systematic review. Chiropr. Man. Ther. 2019, 27, 62.
- Banierink, H.; Ten Duis, K.; Wendt, K.; Heineman, E.; Ijpma, F.; Reininga, I. Patient-reported physical functioning and quality of life after pelvic ring injury: A systematic review of the literature. PLoS ONE 2020, 15, e0233226.
- Stuge, B.; Garratt, A.; Krogstad Jenssen, H.; Grotle, M. The pelvic girdle questionnaire: A condition-specific instrument for assessing activity limitations and symptoms in people with pelvic girdle pain. Phys. Ther. 2011, 91, 1096–1108.
- Majeed, S.A. Grading the outcome of pelvic fractures. J. Bone Joint Surg. Br. 1989, 71, 304–306.
- Nepola, J.V.; Trenhaile, S.W.; Miranda, M.A.; Butterfield, S.L.; Fredericks, D.C.; Riemer, B.L. Vertical shear injuries: Is there a relationship between residual displacement and functional outcome? J. Trauma 1999, 46, 1024–1029; discussion 9–30.
- Cole, J.D.; Blum, D.A.; Ansel, L.J. Outcome after fixation of unstable posterior pelvic ring injuries. Clin. Orthop. Relat. Res. 1996, 160–179.
- Lefaivre, K.A.; Slobogean, G.P.; Ngai, J.T.; Broekhuyse, H.M.; O’Brien, P.J. What outcomes are important for patients after pelvic trauma? Subjective responses and psychometric analysis of three published pelvic-specific outcome instruments. J. Orthop. Trauma 2014, 28, 23–27.
- Bajada, S.; Mohanty, K. Psychometric properties including reliability, validity and responsiveness of the Majeed pelvic score in patients with chronic sacroiliac joint pain. Eur. Spine J. 2016, 25, 1939–1944.
- Rejano-Campo, M.; Ferrer-Peña, R.; Urraca-Gesto, M.A.; Gallego-Izquierdo, T.; Pecos-Martín, D.; Stuge, B.; Plaza-Manzano, G. Transcultural adaptation and psychometric validation of a Spanish-language version of the “Pelvic Girdle Questionnaire”. Health Qual Life Outcomes 2017, 15, 30.
- Grotle, M.; Garratt, A.M.; Krogstad Jenssen, H.; Stuge, B. Reliability and construct validity of self-report questionnaires for patients with pelvic girdle pain. Phys. Ther. 2012, 92, 111–123, Epub 22 October 2011.
- Rashidi Fakari, F.; Kariman, N.; Ozgoli, G.; Ghare Naz, M.S.; Ghasemi, V.; Ebadi, A. Iranian version of Pelvic Girdle Questionnaire: Psychometric properties and cultural adaptation. J. Res. Med. Sci. 2019, 24, 43.
- Fagundes, F.M.L.; Cabral, C.M.N. Cross-cultural adaptation of the Pelvic Girdle Questionnaire (PGQ) into Brazilian Portuguese and clinimetric testing of the PGQ and Roland Morris questionnaire in pregnancy pelvic pain. Braz. J. Phys. Ther. 2019, 23, 132–139.
- Starzec, M.; Truszczyńska-Baszak, A.; Stuge, B.; Tarnowski, A.; Rongies, W. Cross-cultural Adaptation of the Pelvic Girdle Questionnaire for the Polish Population. J. Manip. Physiol. Ther. 2018, 41, 698–703.
- Gutke, A.; Stuge, B.; Elden, H.; Sandell, C.; Asplin, G.; Fagevik Olsén, M. The Swedish version of the pelvic girdle questionnaire, cross-cultural adaptation and validation. Disabil. Rehabil. 2020, 42, 1013–1020.
- Acharya, R.; Tveter, A.T.; Grotle, M.; Khadgi, B.; Koju, R.; Eberhard-Gran, M.; Stuge, B. Cross-Cultural Adaptation and Validation of the Nepali Version of the Pelvic Girdle Questionnaire. J. Manip. Physiol. Ther. 2020.
- Lefaivre, K.A.; Slobogean, G.P.; Valeriote, J.; O’Brien, P.J.; Macadam, S.A. Reporting and interpretation of the functional outcomes after the surgical treatment of disruptions of the pelvic ring: A systematic review. J. Bone Joint Surg. Br. 2012, 94, 549–555.
- Copay, A.G.; Cher, D.J. Is the Oswestry Disability Index a valid measure of response to sacroiliac joint treatment? Qual. Life Res. 2016, 25, 283–292.
