Pelvic ring injuries have an estimated annual incidence of 14–37 per 100,000 inhabitants each year. Treatment can be either non-operative or operative, depending on the injury as well as patient characteristics. The operative treatment of pelvic ring injuries remains a challenging task for surgeons due to the complex three-dimensional (3D) shape of the pelvis, morphological variations, limited access to fracture sites, and narrow bone corridors for screw placement. The goal of operative treatment is to restore pelvic symmetry and achieve stable fracture fixation, which allows for early mobilization and good functional outcome at the long-term.
- pelvic ring injury
- sacroiliac screw
- three-dimensional
- 3D virtual surgical planning
- 3D printing
- navigation
1. Introduction
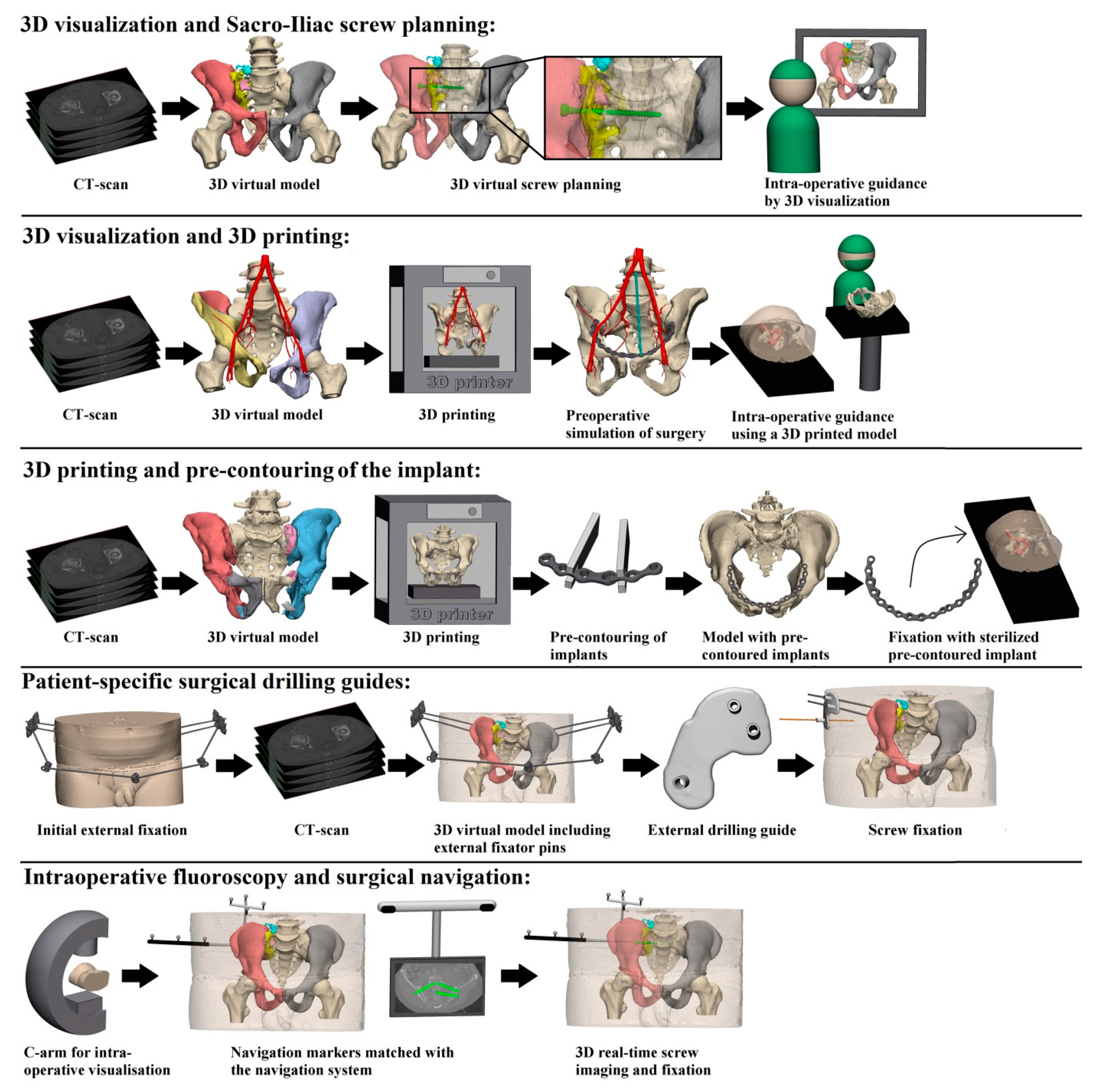
Progress in 3D imaging technologies has resulted in an exponential increase in the usage of these techniques—that is both industry- as well as surgeon-driven- for preoperative planning and for translation of the plan to the operative procedure [1]. In essence, 3D-assisted surgery encompasses a wide spectrum of modalities including 3D virtual preoperative planning, 3D-printed models for pre-contouring of osteosynthesis plates and 3D navigational tools. Some coin these 3D (printing) techniques the “second industrial revolution” in Orthopaedic Trauma Surgery . Nevertheless, the additional clinical value of 3D techniques in pelvic surgery has yet to be elucidated, both practically as well as scientifically.
Conventional X-rays and two-dimensional (2D) computed tomography (CT) images are to date widely used to assess fracture characteristics, reduction quality and positions of osteosynthesis materials in pelvic ring injury treatment [2]. However, 3D virtual models may allow the surgeon to gain more insight in the fracture pattern, surgical approach, and positions of osteosynthesis materials. It has been reported that pre-operative virtual simulation and 3D printing-assisted pre-contoured plate fixation of pelvic ring injuries resulted in precise pre-operative planning and accurate execution of the operative procedures [2]. Moreover, 3D-assisted surgery for percutaneous screw placement may lower the risk of complications and decrease the need for revision surgery due to a lower rate of screw malposition [3]. However, there is a lack of studies with sufficient statistical power to provide evidence on superiority of the available 3D technologies compared to conventional (2D) techniques in different types of pelvic ring injuries.
2. Does 3D-Assisted Operative Treatment of Pelvic Ring Injuries Improve Patient Outcome?
3. Conclusions
Overall, five different techniques of 3D-assisted surgery were identified and are currently in use for pelvic ring injury treatment. These included ‘3D virtual fracture visualization and preoperative planning’, ‘3D printed model assisted surgery’, ‘pre-contouring of osteosynthesis material’, ‘3D printed surgical guides’, and ‘intra-operative 3D imaging’. These 3D-based techniques offer additional tools to improve intra-operative efficiency in terms of operation time, blood loss, fluoroscopy dose, time and frequency as well as accuracy of screw placement. However, improved anatomical reduction or functional outcome following 3D-assisted surgery has not been established so far.
This entry is adapted from the peer-reviewed paper 10.3390/jpm11090930
References
- Balling, H. 3D image-guided surgery for fragility fractures of the sacrum. Oper. Orthop. Traumatol. 2019, 31, 491–502.
- Hung, C.-C.; Li, Y.T.; Chou, Y.-C.; Chen, J.-E.; Wu, C.-C.; Shen, H.-C.; Yeh, T.-T. Conventional plate fixation method versus pre-operative virtual simulation and three-dimensional printing-assisted contoured plate fixation method in the treatment of anterior pelvic ring fracture. Int. Orthop. 2019, 43, 425–431.
- Zwingmann, J.; Konrad, G.; Kotter, E.; Südkamp, N.P.; Oberst, M. Computer-navigated iliosacral screw insertion reduces malposition rate and radiation exposure. Clin. Orthop. Relat. Res. 2009, 467, 1833–1838.
- Zhang, Y.D.; Wu, R.Y.; Xie, D.D.; Zhang, L.; He, Y.; Zhang, H. Effect of 3D printing technology on pelvic fractures:A meta-analysis. Zhongguo Gu Shang = China J. Orthop. Traumatol. 2018, 31, 465–471.
- Berger-Groch, J.; Lueers, M.; Rueger, J.M.; Lehmann, W.; Thiesen, D.; Kolb, J.P.; Hartel, M.J.; Grossterlinden, L.G. Accuracy of navigated and conventional iliosacral screw placement in B- and C-type pelvic ring fractures. Eur. J. Trauma Emerg. Surg. 2018, 46, 107–113.
- Li, B.; He, J.; Zhu, Z.; Zhou, N.; Hao, Z.; Wang, Y.; Li, Q. Comparison of 3D C-arm fluoroscopy and 3D image-guided navigation for minimally invasive pelvic surgery. Int. J. Comput. Assist. Radiol. Surg. 2015, 10, 1527–1534.
- Privalov, M.; Beisemann, N.; Swartman, B.; Vetter, S.Y.; Grützner, P.A.; Franke, J.; Keil, H. First experiences with intraoperative CT in navigated sacroiliac (SI) instrumentation: An analysis of 25 cases and comparison with conventional intraoperative 2D and 3D imaging. Injury 2020.
- Zwingmann, J.; Hauschild, O.; Bode, G.; Südkamp, N.P.; Schmal, H. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: A systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2013, 133, 1257–1265.
- Lefaivre, K.A.; Blachut, P.A.; Starr, A.J.; Slobogean, G.P.; O’Brien, P.J. Radiographic Displacement in Pelvic Ring Disruption. J. Orthop. Trauma 2014, 28, 160–166.
