This study described a novel optical coherence tomography (OCT) finding named “choroidal rift” which may be identified in the choroid of eyes with central serous chorioretinopathy (CSC). In this study we collected data from 357 patients (488 eyes) with CSC who had structural OCT and OCT angiography (OCTA) scans obtained. For each eye, OCT images were graded by two readers in order to assess the presence and the typical features of choroidal rifts. Choroidal rifts were identified as polygonal (and not round-shaped) hyporeflective lesions without hyperreflective margins. Choroidal rifts had to be characterized by a size superior to that of the largest choroidal vessel. Finally, hyporeflective lesions were graded as choroidal rifts only if these lesions had a main development perpendicular to the retinal pigment epithelium. OCT analysis allowed the identification of choroidal rifts in 10 eyes from 9 patients, all with chronic CSC, with an estimated prevalence rate of 2.1%. In 3 out of 10 cases with choroidal rifts, these lesions spanned all the choroidal layers. In the remaining cases, choroidal rifts only partially spanned the choroidal thickness. In OCTA, choroidal rifts were characterized by absence of flow. Combining structural OCT and OCTA information, we hypothesize that choroidal rifts may represent interruptions of the choroidal stroma in correspondence of fragile regions (in between expanded larger-sized choroidal vessels). In conclusion, choroidal rift represents a novel OCT feature which may characterize eyes with chronic CSC and may have a role in the development of irreversible chorio-retinal changes.
- central serous chorioretinopathy
- optical coherence tomography
- choroid
- imaging biomarker
1. Definition
Central serous chorioretinopathy (CSC) is a complex and not entirely understood retinal disease.
2. Introduction or History
Central serous chorioretinopathy (CSC) is a common chorioretinal disease included in the pachychoroid disease spectrum [1]. This disorder may be characterized by the accumulation of fluid in the subretinal and/or sub-retinal pigment epithelium (RPE) space [2]. The subretinal fluid (SRF) collection may cause photoreceptors’ dysfunction, this eventually resulting in visual symptoms such as blurred vision, metamorphopsia, micropsia and reduced contrast sensitivity [3].
Although CSC pathogenesis is multifactorial and not completely understood, the combination of a dysfunctional choroid, which is swollen and hyperpermeable, with an impaired RPE is widely considered as the primum movens eventually resulting in blood-retinal barrier malfunction and SRF accumulation. Furthermore, elevated levels of corticosteroids and/or catecholamine in the blood were demonstrated to be associated with dysfunction and ischemia of the choroidal capillaries, the latter process associated with a compensatory hyperpermeability and leakage of the sparing choroidal vessels [4]. Alternatively, an expansion of the larger-sized choroidal vessels may cause a choriocapillaris (CC) ischemia [5].
Optical coherence tomography (OCT) and OCT angiography (OCTA) technologies have significantly improved the choroidal characterization in eyes with CSC [6]. Importantly, en face OCT imaging displayed that areas of choroidal thickening in CSC eyes may be frequently topographically associated with pathologically dilated veins of the Haller’s layer (or “pachyvessels”) [5]. Notably, OCTA analysis granted the assessment of the choriocapillaris (CC) in eyes with pachychoroid disease, including CSC eyes [7,8]. In the latter studies, the authors demonstrated that the pathological choroidal thickening may be associated with inner choroidal (or CC) ischemia.
Previous important studies employing OCT technology demonstrated that CSC eyes may be characterized by two peculiar hyporeflective regions within the choroidal volume: (i) choroidal caverns and (ii) choroidal loculations. While the latter were described as hyporeflective regions between the outer segment of choroid and sclera [9], the former were described as irregularly small round-shaped hyporeflective spaces within the choroid [10,11,12].
3. Results
Our study cohort included 357 patients (488 eyes of 277 males and 80 females; the mean ± SD age was 53.2 ± 10.9 years), all with chronic CSC (persistent sub-retinal fluid for more than 6 months). Within this study cohort, OCT grading allowed the identification of choroidal rifts in ten eyes from nine patients (seven males and two females; the mean ± SD age was 55.9 ± 8.5 years) with an estimated prevalence rate of 2.1%.
No patient in this subgroup had a clinical history of diabetes or uncontrolled systemic hypertension. Within patients with choroidal rifts, three out of nine patients were previously treated with photodynamic therapy (PDT), while five out of nine patients had treatment with eplerenone. None of our patients had anti-vascular endothelial growth factor (VEGF) therapy at the time of inclusion.
The general appearances of these hyporeflective lesions are shown in Figure 1 and Figure 2. In three out of ten eyes with choroidal rifts, these lesions spanned all the choroidal layers, including the choriocapillaris (Figure 1). In the remaining cases, choroidal rifts only partially spanned the choroidal thickness (Figure 2). In six cases (Figure 1 and Figure 2), hyperreflective vertical filiform-shaped structures were identified within choroidal rifts and were speculated to represent intercapillary pillars of the choroidal vessels, which remained patulous within choroidal rifts. On OCT images, choroidal rifts, which per definition had an irregular shape without hyperreflective margins and they had dimensions superior to the largest choroidal vessels, presented a mean ± SD dimension of 215 ± 78.6 and 589 ± 374.7 μm on the vertical and horizontal diameters, respectively.

Figure 1. Multimodal imaging of a choroidal rift in a case of chronic central serous chorioretinopathy (CSC). (A) Optical coherence tomography (OCT) B-scan and relative IR image with the over-imposed line of scanning demonstrating the presence of a large choroidal rift (orange arrow) crossing all the choroidal layers and seen as a grossly empty prismatic space. A magnified visualization of this region (B) revealed the presence of hyperreflective vertical filiform-shaped structures (white asterisks) within choroidal rifts, which were speculated to represent the remnant of intercapillary pillars. Early (C) and intermediate (D) indocyanine green angiography (ICGA) images demonstrate that the region occupied by the choroidal rift (highlighted with the red arrows) is characterized by a reduced fluorescence because of an absent/reduced choroidal filling.
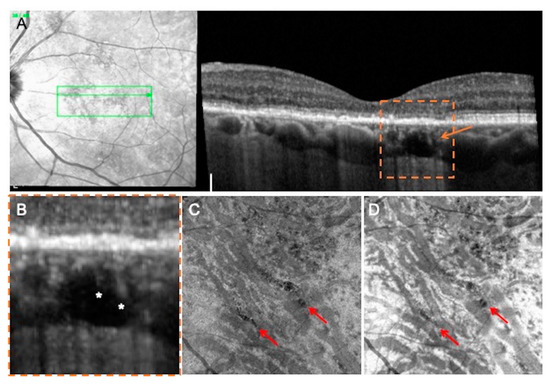
Figure 2. Multimodal imaging of a patient affected by chronic CSC and presenting a choroidal rift. (A) OCT B-scan and relative IR image shows the presence of a choroidal rift (orange arrow) crossing the outer choroidal layers. (A) magnified visualization of this region; (B) reveals the presence of hyperreflective vertical filiform-shaped structures (white asterisks). En face angiographic (C) and structural (D) OCT images revealed that choroidal rifts (highlighted with the red arrows) seem to be interruptions of the choroidal stroma in correspondence of fragile regions (in between major-sized choroidal vessels).
In the evaluation of the OCTA images, choroidal rifts were characterized by absence of flow. More importantly, in the combined evaluation of en face structural and angiographic OCT images, choroidal rifts seemed to be interruptions of the choroidal stroma in correspondence of fragile regions (in between expanded larger-sized choroidal vessels) (Figure 2).
This entry is adapted from the peer-reviewed paper 10.3390/jcm9072260
